Features of the disease in newborn infants
Newborn babies most often develop purulent meningitis due to birth trauma, prematurity or sepsis.
Often the infection enters through the umbilical vessels or placenta during the mother's illness with pyelitis or pyelocystitis during pregnancy. Infectious agents: streptococci, staphylococci and Escherichia coli, other types of bacteria are rare.
Meningitis in infants is characterized by a severe form of the disease, dehydration, disturbances in the gastrointestinal tract, and the absence of high temperature.
This is a dangerous disease for newborns - in 50% of cases, meningitis in infancy ends in death, while in adults 90 percent of patients survive.
Severe excitability or complete lethargy - these manifestations are similar to other pathologies, so the diagnosis can be confirmed in a hospital setting by taking cerebrospinal fluid for examination.
It is not always possible to completely cure such a small patient. They have a high percentage of complications in the form of central nervous system disorders:
- hydrocephalus;
- epilepsy;
- mental retardation;
- paralysis;
- paresis of limbs and cranial nerves.
These children have been under the supervision of specialists for a long time and undergo regular examinations to avoid re-infection.
Reactive form of the disease
The most dangerous type of disease is reactive. This form of the disease can lead to death just a day after the onset of the inflammatory process. For small children this period is reduced to three hours.
The disease begins due to the same pathogens as purulent or serous meningitis. The difference lies in the development of an aseptic inflammatory process, which provokes autoimmune processes in the brain.
The disease is accompanied by the rapid development of cerebral edema, dropsy, and against this background, intracranial pressure significantly increases. The disease can develop as a complication of the following diseases and conditions:
- allergic reaction to injections of certain drugs;
- vasculitis;
- AIDS;
- polio;
- tumor diseases of the central nervous system;
- major stroke;
- brain abscess;
- fetal hypoxia.
When the fetus is hypoxic when passing through the birth canal, a reactive form of meningitis often develops. In this case, it is necessary to begin treatment immediately, otherwise death will occur within a few hours.
The symptoms of this form of the disease repeat the symptoms of purulent meningitis, but add to them:
- temperature 400C and above;
- toxic shock;
- gray skin color;
- numbness of the limbs.
If immediate action is not taken, a complication develops within a few hours due to septic shock, which leads to tissue necrosis on the fingers. Death occurs quickly due to septic shock.
Treatment of the pathology is based on hourly administration of a large dose of antibiotics and supportive care. The drugs are injected directly into the spinal canal, while supplementing therapy with agents to reduce brain swelling.
Danger of disease
Meningitis in infants from birth to one year is very dangerous because half of the cases of the disease end in death, and the other half, having recovered from the disease, receive complications leading to disability: deafness, blindness, mental retardation.
After treatment, the baby begins long-term rehabilitation, the first 2 years of which he must be under the constant supervision of specialists, since there is a risk of an abscess in the brain - a complication can develop at any age and lead to a sharp deterioration in the child’s health.
The danger of this disease is also that the child does not always have pronounced symptoms, for example, high fever. This is due to the lack of established temperature regulation. Therefore, if symptoms similar to meningitis occur, immediately call an ambulance rather than self-medicate.
Signs of meningitis in children
At an early stage of the disease, the clinical picture is represented by nonspecific symptoms. It is difficult to recognize meningitis in an infant, since general lethargy, drowsiness and high body temperature (up to 39°C) occur with many pathologies. The newborn refuses breast milk, his motor activity decreases, and his limbs twitch convulsively.
In later stages, meningitis manifests itself as neurological syndromes.
Nonspecific symptoms
The initial manifestations of the disease are nonspecific for all children. The first signs of meningitis in babies under one year of age:
- incessant high-pitched crying;
- unnaturally pale skin;
- intolerance to loud sounds, bright light;
- skin rash;
- change in breathing rhythm.
Signs of later stages
Meningeal symptoms of late stages of the disease:
- Brudzinsky. When the doctor tries to bring his chin closer to the chest of a sick baby, there is resistance from the neck muscles.
- Kernig. It is impossible to straighten the bent leg of a newborn at a right angle if the baby is lying on his back.
- Lessage. The doctor lifts the baby by the armpits, holding the back of the head with his fingers. A sick newborn child involuntarily pulls his legs towards his stomach and keeps them bent for a long time.
Articles on the topic
- The first signs of meningitis in a child: how the infectious disease manifests itself
- Signs of viral meningitis - how the disease is detected in a child and an adult
- Bacterial meningitis - routes of infection, signs, manifestations and methods of treatment
Risk factors
In a newborn baby, meningitis develops as an independent disease; the cause of its occurrence is infection in the infant’s body. The most common pathogens in this case are staphylococcus, E. coli and streptococcus.
There is a high likelihood of the disease in those children who have suffered damage to the central nervous system before or during childbirth. If a child has a weakened immune system or has developed a pathology in utero, the child is at greater risk of developing meningitis.
Children born prematurely are at risk. Statistics show that meningitis affects boys more often than girls.
Intrauterine infections
The presence of intrauterine infection in a newborn may be suspected already during childbirth. Intrauterine infection may be indicated by the outpouring of turbid amniotic fluid, contaminated with meconium and having an unpleasant odor, and the condition of the placenta (plethora, microthrobosis, micronecrosis). Children with intrauterine infection are often born in a state of asphyxia, with prenatal malnutrition, an enlarged liver, malformations or stigmata of dysembryogenesis, microcephaly, and hydrocephalus. From the first days of life, they have jaundice, elements of pyoderma, roseolous or vesicular rashes on the skin, fever, convulsive syndrome, respiratory and cardiovascular disorders.
The early neonatal period with intrauterine infections is often aggravated by interstitial pneumonia, omphalitis, myocarditis or carditis, anemia, keratoconjunctivitis, chorioretinitis, hemorrhagic syndrome, etc. During instrumental examination, congenital cataracts, glaucoma, congenital heart defects, cysts and brain calcifications may be detected in newborns.
In the perinatal period, the child experiences frequent and profuse regurgitation, muscle hypotension, central nervous system depression syndrome, and gray skin color. In the later stages, with a long incubation period of intrauterine infection, the development of late meningitis, encephalitis, and osteomyelitis is possible.
Let us consider the manifestations of the main intrauterine infections that make up the TORCH syndrome.
Congenital toxoplasmosis
Intrauterine infection with the single-celled protozoan parasite Toxoplasma Gondii leads to severe damage to the fetus - developmental delay, congenital malformations of the brain, eyes, heart, and skeleton.
After birth in the acute period, intrauterine infection manifests itself as fever, jaundice, edematous syndrome, exanthema, hemorrhages, diarrhea, convulsions, hepatosplenomegaly, myocarditis, nephritis, pneumonia. In the subacute course, signs of meningitis or encephalitis dominate. With chronic persistence, hydrocephalus with microcephaly, iridocyclitis, strabismus, and optic nerve atrophy develop. Sometimes monosymptomatic and latent forms of intrauterine infection occur.
Late complications of congenital toxoplasmosis include mental retardation, epilepsy, and blindness.
Congenital rubella
Intrauterine infection occurs due to rubella during pregnancy. The probability and consequences of fetal infection depend on the gestational age: in the first 8 weeks the risk reaches 80%; The consequences of intrauterine infection can include spontaneous abortion, embryo- and fetopathy. In the second trimester, the risk of intrauterine infection is 10-20%, in the third – 3-8%.
Babies with intrauterine infection are usually born premature or at low birth weight. The neonatal period is characterized by a hemorrhagic rash and prolonged jaundice.
The classic manifestations of congenital rubella are represented by Greg's triad: eye damage (microphthalmia, cataracts, glaucoma, chorioretinitis), congenital heart disease (patent ductus arteriosus, ASD, VSD, pulmonary stenosis), auditory nerve damage (sensorineural deafness). If an intrauterine infection develops in the second half of pregnancy, the child usually has retinopathy and deafness.
In addition to the main manifestations of congenital rubella, the child may also have other anomalies: microcephaly, hydrocephalus, cleft palate, hepatitis, hepatosplenomegaly, malformations of the genitourinary system and skeleton. In the future, the intrauterine infection reminds itself of the child’s lag in physical development, mental retardation, or mental retardation.
Congenital cytomegaly
Intrauterine infection with cytomegalovirus infection can lead to local or generalized damage to many organs, immunodeficiency, and purulent-septic complications. Congenital developmental defects usually include microcephaly, microgyria, microphthalmia, retinopathy, cataracts, congenital heart disease, etc. The neonatal period of congenital cytomegaly is complicated by jaundice, hemorrhagic syndrome, bilateral pneumonia, interstitial nephritis, and anemia.
Long-term consequences of intrauterine infection include blindness, sensorineural deafness, encephalopathy, liver cirrhosis, and pneumosclerosis.
Congenital herpetic infection
Intrauterine herpes infection can occur in a generalized (50%), neurological (20%), mucocutaneous form (20%).
Generalized intrauterine congenital herpetic infection occurs with severe toxicosis, respiratory distress syndrome, hepatomegaly, jaundice, pneumonia, thrombocytopenia, hemorrhagic syndrome. The neurological form of congenital herpes is clinically manifested by encephalitis and meningoencephalitis. Intrauterine herpes infection with the development of skin syndrome is accompanied by the appearance of a vesicular rash on the skin and mucous membranes, including internal organs. When a bacterial infection develops, neonatal sepsis develops.
Intrauterine herpes infection in a child can lead to the formation of developmental defects - microcephaly, retinopathy, limb hypoplasia (cortical dwarfism). Late complications of congenital herpes include encephalopathy, deafness, blindness, and delayed psychomotor development.
Features of the clinical picture
The clinical picture of meningitis in newborns is manifested by general neurological symptoms:
- lethargy;
- decreased motor activity;
- drowsiness;
- frequent regurgitation and vomiting;
- breast refusal;
- breathing with a groan and signs of suffocation.
Children weighing more than 2 kilograms may suffer from a rapid rise in temperature up to 39 degrees. In infants, signs of meningitis can be seen in swelling and increased pulsation of the fontanelle, convulsions and throwing the head back.
In premature babies and those with low weight, the clinical picture may look different, proceed in a sluggish form and manifest itself only at the height of the disease. This applies to the absence of bulging and pulsation of the fontanel, throwing back the head. This “erased” clinic occurs with children who were born prematurely and received antibiotics from birth.
The disease can develop rapidly, or it can be protracted, depending on the age, weight and condition of the child. This creates difficulties in diagnosis, but a correct diagnosis can be made by performing a spinal tap.
How to recognize the disease
With intrauterine infection, the disease makes itself felt in the first two days after the birth of the child. If the baby becomes infected while passing through the birth canal, the first symptoms appear somewhat later, but the disease is successfully diagnosed in the early stages. In rare cases, the infection may not be felt for many years.
Symptoms of meningitis in an infant:
- heat;
- fever;
- convulsions;
- increase in the size of the fontanelle;
- pulsation of the fontanel;
- refusal to feed;
- diarrhea;
- general malaise.
Diagnosis is complicated by the fact that such symptoms are a sign of any infectious disease in a newborn. The diagnosis is confirmed by the presence of meningeal syndrome and Lesage syndrome.
Meningeal syndrome allows you to confirm the diagnosis based on the specific reflex activity of a small patient.
To check for the presence of this syndrome, it is necessary to tilt the baby's head to the chest in a supine position. At this time, uncontrolled reflex bending of the knees occurs. This syndrome is characteristic of meningitis in both children and adults.
Lesage's symptoms also refer to specific reflex effects of inflammation of the meninges. If you take a child by the arms and lift him up, he will reflexively throw his head back, while tucking his legs in and bending them at the knees.
The diagnosis can be confirmed by examining the fontanel. When the meninges are inflamed, this part of the skull swells, increases in size and pulsates strongly. Externally, the fontanel looks inflamed.
Premature babies often lack some characteristic symptoms, such as an enlarged fontanelle, which makes timely diagnosis difficult. In this case, the disease often manifests itself as sudden convulsive seizures. The diagnosis can be confirmed and the causative agent of inflammation can be determined using a lumbar puncture.
Types of disease
The following types of meningitis most often develop in infants:
- Viral - occurs against the background of influenza, measles, chickenpox and paratitis, so it is difficult to diagnose.
- Fungal – occurs in newborns born prematurely and in children with weakened immune systems. A child runs the risk of contracting it right in the maternity hospital if hygiene rules are not followed.
- Bacterial - occurs most often, caused by any purulent inflammation if an infection has penetrated. With blood, it reaches the membranes of the brain and creates purulent foci. Purulent meningitis in newborns is formed due to infection with such types of bacteria as Haemophilus influenzae, meningococcus and pneumococcus. In 70% of cases, infection occurs with meningococcal infection, which can be transmitted by airborne droplets, through the mouth or nose, and from there into the blood. A large number of bacteria entering the blood causes a rapid progression of the disease and after 10-12 hours the child may die.
All types of diseases require different treatment methods, which must be prescribed by a doctor, making an accurate diagnosis.
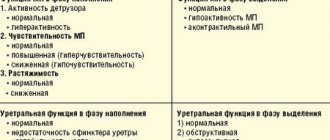
Forms and causes of meningitis
By nature, brain inflammation in newborns can be purulent or serous. The first is caused by a bacterial infection. Serous meningitis of newborns occurs after penetration of the virus. Less commonly, a fungal type of inflammation of the meninges develops. It appears in children with weak immune systems. Doctors identify risk groups for the occurrence of the disease:
- Injuries during childbirth. Damage to the membranes of the brain or nerve trunks during expulsion of the fetus.
- Low birth weight or premature babies. Their immune and nervous systems have not yet developed. Harmful microorganisms easily penetrate the meninges.
- Acquired or congenital immunodeficiency. There is a danger of a severe course of any infection, even a mild one.
- Chronic diseases, operations. The weakened body of newborns is not able to cope with meningococcal infection.
Serous
This form of the disease is mainly caused by viruses (cytomegalovirus, herpes, Epshein-Barr and others). In children with low immunity, inflammation of the brain can be caused by influenza or enterovirus infection. Rarely, serous meningitis in children is of a bacterial or fungal nature. The disease is transmitted from person to person by air, water, household or intrauterine means.
The incubation period is 5-7 days.
Purulent
The causative agents of this form of the disease are pathogenic bacteria. In 70% of cases, purulent meningitis is caused by meningococcal infection. Such inflammation is characterized by the development of severe complications. Reactive ones are especially dangerous. Its incubation period can last several minutes.
The reactive form of the disease begins suddenly, is acute, and has an extremely unfavorable prognosis for children.
Purulent meningitis in newborns is transmitted through air, water and food from the mother. The incubation period lasts from 2 to 5 days. The purulent form of the disease in newborns develops due to factors such as:
- prematurity;
- birth injury;
- sepsis.
Candida
In an organism with weak immunity, the opportunistic fungus Candida quickly spreads. If it enters the membranes of the brain through the bloodstream, it causes severe inflammation - candidal meningitis. At risk are children with diabetes or babies who are prescribed steroid hormones from birth.
The incubation period of the disease is 5-7 days.
Diagnosis and differentiation
Diagnosis of meningitis in a newborn is carried out based on identified symptoms and blood sampling for general, biochemical analysis and PCR testing.
A puncture is also performed to collect cerebrospinal fluid for examination, and a diagnosis is made based on the presence of an inflammatory process.
In special and advanced cases, computed tomography can be performed, and it is also prescribed for differential diagnosis. It is necessary to identify the causative agent of the disease in order to select the appropriate antibiotic for the treatment of meningitis.
Differential diagnosis is carried out according to signs that are specific to this type of meningitis. For example, meningococcal meningitis manifests itself with an acute onset, vomiting, high fever, and convulsions and impaired consciousness appear later.
Moreover, in the absence of pathology of internal organs, meningococci and an increase in protein in the cerebrospinal fluid are present in the baby’s blood. So, all types of meningitis have their own characteristic symptoms, which are used to determine an accurate diagnosis.
Types of meningitis and diagnosis
To diagnose the disease, a puncture is performed, that is, a small amount of cerebrospinal fluid is collected for analysis. The type of disease is determined by the composition of the cerebrospinal fluid.
If more than half of the cells are represented by leukocytes, this is bacterial purulent meningitis, provoked by pathogenic microflora.
In the case when the main part of the structure of the cerebrospinal fluid is represented by lymphocytes, meningitis is serous in nature, that is, provoked by viruses or fungi.
A special approach to therapy
It is important to know that treatment of meningitis occurs only in a hospital setting. You cannot self-medicate or use folk remedies. Therapy should begin by establishing the cause of the disease.
In case of bacterial infection, broad-spectrum antibiotics are used that pass well through the BBB (blood-brain barrier):
- Ceftriaxone;
- Cefotaxime;
- Gentamicin;
- Amoxicillin and other similar drugs.
Medications are administered in maximum doses for a long course, changing them after 12 weeks. If the disease is viral or fungal, then antiviral or antifungal agents are administered. Intravenous injections.
The baby is also given detoxification, anticonvulsant and dehydration therapy. If cerebral edema occurs, Dexamethasone is used.
In case of a viral or fungal infection, the baby recovers in one to two weeks. Bacterial meningitis in infants takes much longer to treat and depends on the severity of the disease and the body’s resistance to the disease.
Treatment
In case of meningitis, the newborn is placed in the infectious diseases department of the hospital. It is prohibited to treat a child at home, since the risk of severe complications and death is high. Therapy depends on the cause of the disease. The main principle of treating meningitis is eliminating the pathogen:
- If a meningococcal or other bacterial infection is detected, doctors prescribe a course of antibiotics.
- For a viral disease, doctors prescribe treatment for the symptoms of the disease.
- For the fungal form, the basis of treatment is antimycotic agents.
Antibiotics
For meningitis, the basis of treatment is taking antibacterial drugs. Doctors prescribe broad-spectrum medications. They cause the death of harmful microorganisms. Antibiotics ( Amoxicillin, Cefotaxime, Gentamicin ) are administered intravenously to newborns. The course of treatment with drugs is long - until the child recovers.
Anticonvulsants
Doctors prescribe this group of medications to eliminate seizures that occur in an infant due to damage to the central nervous system. The action of anticonvulsants is aimed at suppressing its work. Medicines prevent nerve impulses from traveling through the brain and spinal cord. Anticonvulsant treatment consists of intravenous administration of Seduxen and Sibazon.
Diuretics
To reduce brain swelling, doctors prescribe diuretics for children. They help eliminate headaches, nausea, and reduce intracranial pressure. To prevent dehydration, diuretics are administered into the child’s body along with plenty of fluid. For the treatment of newborns, doctors prescribe Veroshpiron, Furosemide, Diacarb.
Severe consequences and poor prognosis
This dangerous disease for newborns does not always end favorably, complications always occur in young children, even long-term therapy in this case is powerless, the consequences are disorders in the central nervous system, mental retardation, deafness, blindness, hydrocephalus, and blood clotting disorders.
Within two years there is a risk of a brain abscess.
In the case of the disease in infants, mortality rates reach 30% and 65% if an abscess has formed in the brain.
The prognosis for meningitis of all types depends on the cause of the disease and the form of its course. Bacterial meningitis occurs in an acute form and can result in the death of the baby. Even if the baby survives, he will still have complications that last a long time.
Such a child remains registered with pediatricians and infectious disease specialists for a long time and undergoes regular examinations. If the disease is mild, the child recovers within a few weeks without consequences.
Viral meningitis occurs in a milder form and goes away within 2 weeks if treatment is started in a timely manner.
At a younger age
In children over the age of two, meningitis can be caused by:
- viruses of “childhood” diseases (rubella, measles, chicken pox);
- simple microorganisms;
- fungal infections;
- bacterial infection.
Often, meningitis in children develops as a result of infection with meningococcal infection due to contact with a carrier of the virus, which can be stray animals or a sick person.
The risk group consists of children who suffered the following diseases and injuries at an early age:
- purulent inflammation of the middle ear (otitis);
- sinusitis;
- sinusitis;
- spinal injury;
- head injury;
- hydrocephalus;
- infections of the central nervous system;
- flu.
And children who underwent brain surgery before the age of three.
Symptoms of the disease from 2 years
In young children over the age of two years, the symptoms of this disease are exactly the same as in adults:
- fever with high temperature;
- nausea and profuse vomiting;
- severe splitting headache;
- weakening of the neck muscles, due to which the head is always in a lowered position;
- irritability;
- drowsiness.
The onset of the disease is accompanied by a headache, which is later joined by a high fever. At this time, the child may experience blurred consciousness, problems with speech and loss of strength, which provokes drowsiness and apathy.
Having discovered the first alarming symptoms, you must immediately call a doctor and send the child to the hospital, since progressive inflammation of the meninges can lead to serious complications, including death.
What can be done for prevention?
For prevention purposes, babies born severely weakened need to be vaccinated. Since the disease has many different forms, even vaccination cannot guarantee protection against meningitis.
Viral meningitis is spread by airborne droplets and in order to avoid becoming infected, it is necessary to maintain personal hygiene and heat treat food and objects that are used by all family members.
When there are patients with acute respiratory infections or acute respiratory viral infections in the family, the small child must be isolated from the patient. All family members should use Interferon three times a day for a week - this will also reduce the risk of infection.
Also, for prevention, you should drink a complex of vitamins and minerals, eat fortified foods, do not get too cold and do not walk in crowded places. This will help protect the family from contracting meningitis, including the newborn baby.
In the case of meningitis, the main thing is to quickly begin treatment, this is what will help avoid the death of a newborn child and help him recover and increase his chances of survival. Experts say that proper nutrition and good immunity will help the child avoid the disease.