Meningitis is a dangerous infectious disease that affects the meninges. It can be bacterial, fungal or viral in nature. Viral meningitis is also called serous meningitis and causes inflammation of the brain and spinal cord. Serous meningitis occurs most often in the summer, which is associated with the seasonality of some viral diseases. However, the risk of infection at other times of the year cannot be excluded. When the first signs of meningitis appear, it is important to consult a doctor as soon as possible.
At the Yusupov Hospital, the patient will be provided with all the necessary medical care: they will conduct an examination and prescribe adequate treatment. Experienced doctors at the Yusupov Hospital can quickly determine the type of disease and, without wasting time, begin therapy, which will reduce the risk of complications.
Treatment of viral meningitis
There are no special medications that help effectively fight the viruses that cause meningitis. Antibiotics are ineffective in this case. For inflammation of the meninges caused by herpetic infection, acyclovir and other antiherpetic drugs are used.
In most cases, treatment of meningitis is limited to measures aimed at combating the symptoms of the disease. For example, a doctor may prescribe painkillers, antipyretics, and antiemetics.
In most adult patients, viral meningitis goes away without any treatment within 5-10 days. Some people take longer to recover. If encephalitis (an inflammatory process in brain tissue), pericarditis (inflammation of the pericardial sac), or hepatitis develops, the prognosis worsens.
Prevention: what to do to avoid catching the disease during an epidemic?
To date, several types of vaccines have been developed that can prevent infection by certain viruses and bacteria. First of all, such vaccination is recommended for children and those who travel to areas where outbreaks of the disease have been recorded.
It is always necessary to observe basic hygiene rules - use a separate towel, toothbrush, and wash your hands frequently. If there is a person with meningitis in the house, he should be isolated as much as possible from healthy family members. Close contact with the patient should be limited.
Advice! To prevent the spread of epidemics, it is necessary to frequently ventilate rooms where large numbers of people gather (schools, barracks, large offices) and carry out systematic wet cleaning there.
How to prevent viral meningitis?
There are vaccines against some viral infections that can cause inflammation of the meninges, such as influenza, measles, and mumps. However, there are no vaccinations against enteroviruses, the most common causative agents of the disease. In order to avoid getting an infection, you need to follow some general recommendations:
- Wash your hands often with soap, especially if you have touched objects in public places.
- Avoid touching your face with unwashed hands.
- Avoid close contact with a sick person. Don't hug, don't kiss, don't share utensils.
- When coughing or sneezing, do not cover your mouth and nose with your hands - use a handkerchief for this.
- Thoroughly wash and disinfect items that are frequently touched by a large number of people (such as door handles), especially if there are sick people among them.
If you notice the first signs of the disease, you should immediately consult a doctor. Despite the fact that viral meningitis is a relatively “harmless” form of the disease, it can be severe and cause life-threatening complications. Don’t delay, seek help in Moscow: +7 (495) 230-00-01
Viral meningitis is usually milder than bacterial meningitis, less often leads to serious complications, and most often does not pose a threat to life. The infection caused by the virus goes away on its own within 5-10 days, and as a rule, it is not even necessary to take special antiviral drugs; symptomatic therapy is sufficient.
However, all this does not give reason to take your condition lightly and ignore the first symptoms of the disease.
Take care of yourself, book a consultation now
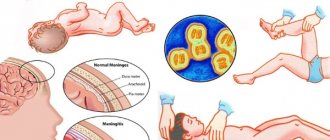
Symptoms of the disease
The danger of the disease is that its first stages may be asymptomatic or accompanied by a slight increase in temperature, chills, and weakness. Sometimes a headache appears, which is accompanied by nausea, rarely vomiting.
Viral meningitis at the peak of its development has more pronounced symptoms. This usually occurs on the 4th day after infection. The pathology is accompanied by the following symptoms:
- headache;
- malaise;
- muscle pain;
- nausea, vomiting;
- diarrhea;
- cutting pain in the abdomen;
- runny nose;
- coughing;
- Brudzinski's symptom (severe pain when tilting the head).
Parents should closely monitor their child's condition to exclude or promptly diagnose viral meningitis in children. In infected infants, swelling and strong pulsation of the fontanel are observed. Loss of consciousness, excessive restlessness, and unintentional irritability may often occur. A severe form of the disease is accompanied by loss of consciousness and coma. With timely diagnosis and treatment, the disease lasts about two weeks.
Common signs of viral meningitis in adults
Typically, viral meningitis is manifested by the following general symptoms:
- headache;
- increased body temperature, fever;
- tension in the neck muscles, resulting in torticollis;
- constant drowsiness;
- it is difficult for the patient to wake up from sleep;
- increased sensitivity to bright light;
- decreased appetite;
- nausea and vomiting;
- lethargy, feeling of exhaustion.
The signs of viral meningitis at the onset of the disease are almost impossible to distinguish from the signs of bacterial meningitis. Until tests are carried out, it is impossible to say for sure which pathogens caused the infection. Even if you feel relatively well, your condition can get very worse at any given time.
If these symptoms begin to bother you, you should immediately seek medical help from a neurologist in Moscow. If the infection is caused by harmful bacteria, there is a risk that it will cause brain damage, hearing loss and other functions.
Enduring pain is life-threatening!
Take care of yourself, schedule a consultation today
In addition, signs characteristic of a particular infection may occur, for example, cough, runny nose, and skin rashes.
Until you know the cause of the disease, you don't know how much risk you have. Typically, inflammation of the meninges is more severe in children and people with reduced immunity, but even in a strong adult, the symptoms of viral meningitis should never be ignored. There is always a risk of serious complications.
See your doctor. A specialist will examine you, prescribe an examination, understand the cause of the disease, and select the best treatment. Our experienced neurologists will definitely help you, contact us by phone
We will call you back
Leave your phone number
Various viral infections can lead to the development of an inflammatory process in the membranes of the brain. Almost every person encounters them during their life, but in most people this does not lead to the development of meningitis.
The most common pathogens of viral meningitis: enteroviruses, arboviruses, mumps virus, herpes, lymphocytic choreomeningitis, measles, adenoviruses, HIV. Let's talk about each of them in more detail.
Enteroviruses
Enterovirus infection is the most common cause of viral meningitis (more than 85% of all cases). Most often, inflammation of the meninges is caused by the Coxsackie virus and the ECHO virus.
Infection with enteroviruses occurs through the fecal-oral route (the pathogen enters the body through the mouth from the surface of unwashed hands, vegetables and fruits, and from contaminated water). The virus can also enter the body through the respiratory tract.
The risk of contracting enterovirus infection is highest in summer and early autumn.
Ways of spread of infection
The carrier of enteroviruses that can cause serous-lymphocytic meningitis is a person. In addition to patients with pronounced clinical forms, sources of infection spread can be patients with erased signs of the disease and healthy virus carriers. The entry point for infection is the gastrointestinal or respiratory tract.
Viral meningitis is transmitted both by airborne droplets (through direct interaction with a patient) and by contact household contact (through infected household items, dishes, toys, contaminated food and water).
The main risk group for morbidity includes children under 9 years of age, the elderly and people with weakened immune systems.
Arboviruses
Arboviruses are more than 500 viruses grouped into several families. According to North American statistics, they cause viral meningitis in 5% of cases. The pathogens are transmitted by arthropods, mainly mosquitoes and ticks.
The peak incidence occurs in summer and early autumn. In most cases, pathogens do not cause inflammation of the meninges in their pure form, but meningoencephalitis. In such patients, seizures occur more often than with other types of viral meningitis.
Regardless of what pathogen causes the infection, you should immediately contact an experienced neurologist. Lack of medical care, self-diagnosis and self-medication can lead to negative consequences.
Mumps virus (mumps)
The main target of the mumps virus is the parotid salivary glands (as they enlarge, the patient’s face acquires a characteristic appearance, for which the disease received its second name – “mumps”). But other organs can also be affected, in particular the membranes of the brain.
With the introduction of vaccination, the importance of mumps as a cause of viral meningitis has decreased dramatically. The disease has become extremely rare in developed countries. However, where vaccine shortages are severe, mumps accounts for 10-20% of meningitis cases. Most often, men aged 16-21 years are affected.
Herpes viruses
The most common pathogens of meningitis in this family include: herpes simplex virus types 2 and 6, chickenpox, Ebstein-Barr, cytomegalovirus. Collectively, they cause about 4% of cases.
You can become infected at any time of the year. If inflammation of the meninges is combined with encephalitis, the death of the patient is possible. The earliest possible initiation of treatment with acyclovir is of great importance.
Lymphocytic choreomeningitis virus
Currently, this pathogen causes viral meningitis quite rarely. Infection occurs during contact with rodents: mice, hamsters, etc., as well as their excrement. At high risk are workers in laboratories that use rodents, pet owners, and people who live in rural areas in unsanitary conditions.
Measles
With the introduction of vaccination, the disease has become extremely rare, but the pathogen poses a great danger due to its high infectiousness. The World Health Organization now considers eliminating measles worldwide as one of the most important tasks.
HIV
HIV infection can cause atypical viral meningitis, which is prone to chronicity and relapse. In addition, the pathogen can affect the nervous system and cause serious neurological disorders.
Although many viral infections that cause inflammation in the meninges do not require special antiviral treatment, medical supervision and symptomatic therapy are very important. When the first signs of meningitis appear, you should immediately seek medical help at a neurology center. Make an appointment with a neurologist in our clinic by phone: +7 (495) 230-00-01
Get a consultation with a doctor
Preventive actions
Treatment of any form of meningitis does not begin at the time of discharge from the hospital. A whole range of preventive measures will be recommended, some of which will have to be observed and carried out for 4 years. Prevention will not hurt those who have been in contact with the patient.
The best prevention is considered to be a strong immune system, which can be easily maintained with a healthy diet and vitamin supplements. Adults need to give up alcohol and smoking, children and their parents need to ensure a healthy lifestyle. Vaccination against tuberculosis may be recommended. This procedure should not be ignored. This guarantees no relapse.
In addition, it is recommended:- do not visit polluted water bodies;
- regularly do wet cleaning and ventilate the room;
- wash your hands after going outside and before eating;
- wash fruits and vegetables before eating;
- do not drink tap water;
- observe the rules of personal hygiene.
Principles of nutrition
Not only ready-made vitamin complexes, but also recommendations from alternative medicine will help strengthen the immune system. Children need to be taught from early childhood the dangers of eating unhealthy foods. Therefore, it is necessary to exclude carbonated sweet drinks, spicy, fried, fatty foods, reduce salt and sugar to a minimum, and avoid visiting fast foods. The menu of a person who has had meningitis should include:
- fresh vegetables and fruits;
- dairy products;
- hard cheeses;
- lean meats (boiled, steamed);
- sea fish and seafood;
- nuts;
- buckwheat, cheese;
- dried fruits.
Even in modern supermarket chains you can select products that provide balanced and healthy nutrition.
Often a relapse can be triggered by contact with street animals. With all the great love for cats and dogs, it is advisable to exclude this. After suffering a pathology, children become much smarter and will agree with their parents. Pets need to be dewormed and treated with flea prevention. Do this a few days before the former patient returns.
Long walks in the fresh air, swimming, and leisurely cycling will help not only strengthen the immune system, but also support the heart muscle.
Traditional medicine is a separate, huge world that helps maintain the normal immune system, increase resistance and saturate the body with vitamins. The source of vitamin C, which is important for a healthy immune system, is not only found in citrus fruits. They are rich in:
- dill;
- parsley;
- rose hips and rowan;
- ginger root;
- bell pepper;
- figs;
- kiwi;
- Brussels sprouts;
- beef liver;
- sea buckthorn oil;
- pollen;
- currant.
No less useful for maintaining and restoring immunity are herbal infusions or decoctions, which you can prepare yourself. For this, herbs that have an anti-inflammatory effect are used. You can safely use:
- mint;
- dandelion;
- chamomile;
- cornflower flowers;
- nettle;
- primrose;
- coltsfoot;
- St. John's wort.
Honey is a natural antibiotic and a rich source of vitamins. Therefore, it should be present on the menu throughout the entire recovery period, if there is no allergy to this product. It, like flower pollen, can be safely added to drinks and strengthening mixtures. One of these mixtures gives a powerful strengthening effect. To prepare you will need:
- prunes;
- dried apricots;
- raisin;
- nuts.
You need to take 200 grams of these components. Grind everything in a meat grinder or using a blender. Add a glass of honey and chopped lemons (3 pcs.) to the resulting mass. Pass the lemons through a meat grinder along with the peel.
Honey loses its healing properties in hot water. It is better to dissolve it in drinks whose temperature does not exceed 65 °C.
Don't forget about the benefits of cranberries. A fruit drink made from this healing berry will quickly help tidy up and strengthen the immune system. For cooking, you can use fresh and frozen berries. A glass of cranberries must be crushed and the juice squeezed out. Dilute the juice with water, bring to a boil, but do not boil. It is not advisable to add sugar. It kills many beneficial substances in the drink. It is better to add honey to warm fruit drink.
What can a doctor find during an examination?
Diagnosis of viral meningitis begins with an examination by a neurologist. The doctor can detect not only characteristic symptoms of the nervous system, but also general signs of infection caused by viruses: damage to the mucous membranes of the respiratory tract (as with a cold), skin rashes, etc.
At this stage, a preliminary diagnosis can be made. For a more accurate diagnosis, it is necessary to conduct some laboratory tests.
Only special diagnostics at a neurological center will help to understand the causes of meningitis and choose the optimal treatment. Sometimes the patient's life is at stake.
Take care of yourself, book a consultation now
Symptoms of bacterial and viral meningitis at the onset of the disease are usually approximately the same. Based on an external examination, it is not always possible to say which pathogen caused the infection.
But the further course of the disease can vary greatly. Most often, infections caused by viruses go away on their own within a few days, without special antiviral therapy. And if inflammation of the meninges is caused by pathogenic bacteria, there is always a risk of severe complications, even death.
For bacterial infections, symptomatic therapy alone is not enough - you need to start administering antibacterial drugs to the patient as early as possible.
Our expert in this field:
Vasinkina Inna Yurievna
Neurologist
Call the doctor
Modern laboratory methods for diagnosing viral meningitis
Viruses that cause inflammation of the meninges can be found in various biological materials:
- swabs from the nose or throat;
- chair;
- blood;
- cerebrospinal fluid.
With the help of special studies - complement fixation reaction (FFR), polymerase chain reaction (PCR) - you can detect viral antigens, DNA, or antibodies that the body produces in response to the introduction of pathogens.
To analyze cerebrospinal fluid, it is necessary to perform a lumbar puncture, a procedure during which a special needle is inserted between adjacent vertebrae into the space around the spinal cord. By analyzing the composition of the spinal fluid, the presence of a viral infection can be assumed.
Meningitis is a dangerous disease. Even if the patient’s health is relatively good at the moment, it is never possible to say how it may change in the near future. Only timely diagnosis in a clinical setting will help prescribe the correct treatment and minimize risks. Consult a doctor