When several or all eye muscles are paralyzed, ophthalmoplegia occurs. This condition may occur due to damage to the optic nerves. In this case, one or both eyeballs may be damaged. Their motor ability is limited or lost in some types of disease. Let's look at the causes of ophthalmoplegia and methods of treatment.
In this article
- Causes of ophthalmoplegia
- Types and symptoms of ophthalmoplegia
- Diagnosis of the disease
- Treatment methods for ophthalmoplegia
- Complications of ophthalmoplegia
- Prevention
Causes of ophthalmoplegia
Various factors can serve as prerequisites for the development of this pathology. It can be either congenital or acquired as a result of certain diseases. At the same time, ophthalmoplegia occurs with equal frequency in men and women. Here are the most common causes of optic nerve palsy:
- severe infectious diseases, for example, tetanus, diphtheria, botulism;
- eye tumors and neoplasms;
- muscle dysfunction (myasthenia gravis, etc.);
- traumatic brain injuries;
- pathologies of the endocrine system - diabetes, problems with the thyroid gland;
- encephalitis;
- severe intoxication of the body;
- food or alcohol poisoning;
- chronic sinusitis;
- multiple sclerosis;
- brain diseases;
- trigeminal neuralgia;
- CNS diseases and other factors.
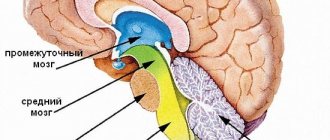
If any of these cases occurs, disruption of the activity of the nerves responsible for muscle contraction may occur. There are three in total:
- oculomotor, with the help of which we are able to turn the eyeball in different directions: up, down, towards the nose;
- block-shaped, providing the ability to rotate to the lower temporal angle;
- abducens - this nerve is responsible for turning the eyeball towards the temple.
Violation of the innervation of the muscles leads to a loss of their tone and the inability to move the eyes - paralysis occurs. Ophthalmoplegia has different forms.
Symptoms of internuclear ophthalmoplegia
The first and main sign that you should pay attention to is difficulty when trying to move your eyes. One (the healthy eye) moves normally, while the affected neighboring eyeball does not turn with it. An additional symptom is uncontrollable twitching that periodically occurs in the healthy eye. The general picture of the pathology is crowned by the deviation of the eyes from a single horizontal axis (that is, one is higher than the other).
A similar situation is observed with damage to the lower part of the bundle of nerve fibers in the region of the brain (medial longitudinal fasciculus), on which the implementation of motor, sensory, integrative and conduction functions—the pons—depends.
If there is a violation of the integrity of the fibers of the upper part, then the pathology spreads to the medial rectus muscles of each eye. A typical symptom in this case is convergence disorder, where the muscles lose the ability to converge on the observed object. The eyeballs diverge in opposite directions; this process can occur both horizontally and vertically. Additionally, an involuntary and uncontrollable oscillation is felt in each eyelid with periodic changes in direction.
Internuclear ophthalmoplegia affecting one eye may be aggravated by horizontal paresis of the neighboring eye, making it impossible to move the gaze in the horizontal direction. In this case, they speak of the onset of one and a half syndrome.
Types and symptoms of ophthalmoplegia
In modern medicine, the disease is divided into several main types:
- Internal ophthalmoplegia. It is characterized by weakening or paralysis of the muscles of the iris and ciliary body. In this case, the mobility of the eye is not impaired, but the pupil is permanently dilated, and a spasm of accommodation may also be observed.
- External ophthalmoplegia. With this type of pathology, the muscles on the outside of the eyeball are affected. At the same time, it can hardly move or is completely paralyzed. The external type of ophthalmoplegia is characterized by diplopia - double vision, but the pupil's reaction to light is preserved. Due to the uneven distribution of the tear film, the dryness of the mucous membrane of the eyes increases. Patients also complain of increased lacrimation. Internal and external ophthalmoplegia can also be partial or complete. In complete ophthalmoplegia, both the external and internal muscles of the visual organs are affected.
Total ophthalmoplegia is also characterized by immobility of the eyeballs and drooping (ptosis) of the upper eyelids - this condition is called Hutchinson's face. The patient has to tilt his head back to be able to see normally from under drooping eyelids. Partial ophthalmoplegia is a condition during which paresis of only the external or only the internal muscles of the eye develops.
- Internuclear ophthalmoplegia. This type of disease is characterized by damage to the muscles that are responsible for the simultaneous movement of the eyeballs. With unilateral internuclear ophthalmoplegia, one of them can be fixed in some position, and on the second, nystagmus occurs - frequent involuntary twitching. Most often, internuclear ophthalmoplegia is a consequence of multiple sclerosis, as well as stroke, head injuries, drug intoxication and some other risk factors. Patients complain that they cannot look in the same direction with both eyes at the same time.
- Supranuclear ophthalmoplegia. Its other name is Steele-Richardson-Olszewski syndrome. This is a rare brain disorder that causes problems with motor function and eye movements. It is also characterized by gaze paralysis - there is no simultaneous eye movement up and down or left and right. Many people complain that they are not able to direct their gaze in the right direction at will.
Symptoms
The characteristic symptoms of ophthalmoplegia are the following clinical manifestations:
- disorder of the motor functions of the eyeball (its mobility is reduced and limited, or absent altogether);
- the presence of mydriasis is noted (a condition of the eye when the pupils are unnaturally dilated);
- swelling of the tissue around the eyeball appears;
- protrusion of the eyeball is observed;
- there is diplopia (doubling of the perceived object or object);
- ptosis (abnormal drooping) of the upper eyelid;
- the pupils do not react to the light beam entering the eye;
- the quality of vision is reduced;
- there is pain (both in the eye itself and in the tissues around it - forehead, upper jaw).
Diagnosis of the disease
Ophthalmoplegia has characteristic external signs. But in order to distinguish it, for example, from paralytic strabismus, and also to identify the exact type, a number of diagnostic hardware tests are carried out:
- Ultrasound of the eye allows you to detect the features of the eyeballs and study the condition of the orbital cavity;
- X-ray of the skull - the image will show internal damage, if this is the cause, as well as the condition of the sinuses;
- computed tomography of the head and neck makes it possible to detect neoplasms, which are one of the causes of ophthalmoplegia;
- proserine test for the diagnosis of myasthenia gravis;
- angiographic examination of cerebral vessels;
- perimetry to determine the boundaries of the field of view.
Depending on what is the cause of the disease, consultation and examination by highly specialized specialists is also required: in case of a neoplasm - an oncologist, in case of suspected pathology of the central nervous system - a neurologist.
How does the disease manifest itself?
Internuclear ophthalmoplegia is a disorder of synchronous movement of the eyeballs. Muscles and nerves control movement and normally perform their work in harmony.
In this article
- How does the disease manifest itself?
- Etiology of the disease
- Symptoms of internuclear ophthalmoplegia
- Diagnostics
- Treatment
- Forecast
Several external eye muscles are involved in the process. In practice, it looks like this: when you turn your gaze to the right, the right rectus lateral muscle and the left rectus medialis muscle contract. Control is exercised by the oculomotor nerve, which contains motor and autonomic fibers, and the overall control of the entire mechanism is performed by the pontine center.
Treatment methods for ophthalmoplegia
Treatment consists of eliminating the disease that caused the paralysis, as well as restoring the functionality of the muscles and nerves. Therapeutic interventions include several aspects.
Drug treatment. The patient may be prescribed various medications depending on the etiology:
- anti-inflammatory drugs;
- topical corticosteroids;
- vitamins B and C;
- nootropics to improve nervous activity;
- drugs that eliminate muscle weakness.
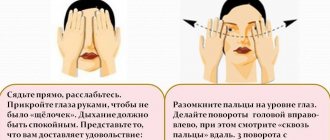
Hardware therapy. Along with taking medications, treatment using hardware procedures - electrophoresis, phonophoresis, acupuncture - also produces effective results. This helps strengthen the eye muscles and eliminate spasm.
Surgical intervention. It is prescribed if it is necessary to eliminate the tumor that is the cause of paralysis, as well as restore muscle activity of the eyes, and raise the upper eyelid with ptosis.
Three methods are used to influence muscles:
- myotomy (dissection);
- recession (pushing back);
- tenomyoplasty (lengthening).
Surgeries for ophthalmoplegia are aimed at restoring the correct balance between the eye muscles. The doctor decides what type of intervention is necessary, taking into account the existing form of pathology and its severity, the patient’s age and other characteristics. As a rule, several muscles are operated on at once. There are cases when a strengthening operation is performed on one eye and a weakening operation on the other.
The success of treating ophthalmoplegia depends on timely contact with specialists, as with many other diseases, and not only eye ones.
Treatment
In cases of mild, newly diagnosed myasthenia and the ocular form, only kalimin and potassium preparations are used in treatment.
Kalimin 60N, 1 tablet 3 times a day with an interval of at least 6 hours. Potassium chloride 1 g 3 times a day or potassium-normine 1 tablet 3 times a day.
In cases of severe muscle weakness or the presence of bulbar disorders, glucocorticoid therapy is used: prednisolone at a dose of 1 mg/kg body weight strictly every other day in the morning (usual doses are 60-80 mg per day, the minimum effective dose is 50 mg per day, every other day).
One tablet of prednisolone contains 5 mg, respectively, the daily dose of prednisolone is 12-16 tablets. A Metypred tablet (one of the commercial names of methylprednisolone) contains 4 mg, but its effectiveness is equal to 1 tablet of prednisolone 5 mg, therefore, in terms of Metypred, the number of tablets is the same 12-16 tablets, and the total dose will be less [ source not specified 152 days
].
Prednisolone 60 mg in the morning every other day.
Taking prednisolone is long-term, remission can occur after 1-2 months, then the dose of prednisolone 0.5 tablets is reduced to a maintenance dose of 10-40 mg every other day. And then slowly, with caution, 0.25 tablets until the drug is completely eliminated.
Taking prednisolone requires monitoring blood sugar and monitoring by a local physician (blood pressure, prevention of steroid ulcers, osteoporosis).
In the first 1-2 years from the onset of the disease, in the generalized form of myasthenia gravis, surgical intervention is performed to remove the thymus gland (thymectomy). The effect of thymectomy develops in the interval of 1-12 months from the moment of thymectomy; the effectiveness of thymectomy is assessed after 1 year.
In old age, when prednisolone therapy is insufficiently effective, when it is impossible to prescribe prednisolone, and when prednisolone is discontinued, cytostatic therapy is prescribed. In mild cases - azathioprine 50 mg (1 tablet) 3 times a day. In more serious cases - cyclosporine (Sandimmune) 200-300 mg per day or Cellcept 1000-2000 mg per day.
In case of exacerbation of myasthenia gravis, plasmapheresis and administration of intravenous immunoglobulin are acceptable and justified. It is advisable to carry out plasmapheresis 500 ml every other day N5-7 with replacement with plasma or albumin.
Immunoglobulin is administered intravenously at a dose of 5-10 g per day up to a total dose of 10-30 g, on average 20 g. Immunoglobulin is administered slowly, 15 drops per minute.
In 2021, health regulators in the US (FDA), EU (EMA) and Japan (MHLW) approved Soliris (eculizumab) as a treatment for patients with generalized myasthenia gravis (gMG).
Complications of ophthalmoplegia
The consequences of advanced ophthalmoplegia can have a very negative impact on the condition of the visual organs. Paralysis of the internal muscles leads to impaired accommodation and decreased visual acuity. Internuclear ophthalmoplegia can cause the development of persistent nystagmus.
Inflammatory diseases such as conjunctivitis, keratitis, blepharitis are often present; the patient’s normal functioning of the lacrimal and meibomian glands is disrupted. Paralysis of the eye muscles is accompanied by facial asymmetry. With supranuclear ophthalmoplegia, difficulties with orientation in space and imbalance also arise. Another common complication of ophthalmoplegia is xerophthalmia, drying of the conjunctiva and cornea.
Ophthalmoplegia - causes and treatment
Ophthalmoplegia is a pathological condition of the organ of vision caused by damage to the oculomotor nerves. It develops against the background of complications of brain diseases, severe infectious lesions, and intoxications of the body. Ophthalmoplegia is manifested by paralysis of all or individual groups of the eye muscles, which leads to decreased mobility of the eyeball or its complete immobility. The disease can be detected in one eye or in both eyes at once.
Prevention
There are no special preventive measures in this case. To reduce the risk of pathology, you need to adhere to general recommendations:
- after eye injuries, head bruises, you should monitor the condition of the visual organs; if discomfort occurs, you should visit an ophthalmologist for diagnostic purposes;
- engage in timely treatment of infections, preventing transition to the chronic stage;
- Observe precautions when frequently working with toxic substances;
- If there are factors that can lead to ophthalmoplegia, such as diseases of the nervous and endocrine systems, you should also undergo regular examinations by a specialist so as not to miss the development of pathology.
A careful and careful attitude to eye health will help to detect negative symptoms in time and begin appropriate therapy.
Causes
CPEO is caused by mutations in mitochondrial DNA (inherited or sporadic). The disease can be inherited in an autosomal recessive, autosomal dominant, or mitochondrial manner. The TWNK and SLC25A4 genes are involved in the autosomal dominant type of inheritance, POLG and RRM2B are involved in the autosomal dominant and autosomal recessive type of inheritance, the MTTL1 gene is most often associated with the mitochondrial type of inheritance, along with other mtRNA and mtDNA genes.
CPEO can occur against the background of other diseases: neuromuscular (POLG-associated ataxias), mitochondrial myopathies (Cairns-Sayre syndrome).
The prevalence of chronic progressive external ophthalmoplegia is unknown.
Classification
Ophthalmoplegia can be congenital or acquired, affecting one eye or both.
A congenital disease is most often accompanied by concomitant abnormalities in the visual organs, and an acquired one can occur in acute and chronic forms.
The disease has the following varieties:
- External ophthalmoplegia is associated with damage to the muscles that are located on the outside of the eye, while the eyeball turns towards the healthy muscle, causing duality of objects, it is partially or completely immobilized.
- Internal - when the internal muscles are affected, the pupil dilates in bright light.
- The partial form affects both muscle groups, but they are affected differently.
- Complete ophthalmoplegia - all types of muscles are affected equally, paralysis of the eyeball appears.
- The supranuclear form is accompanied by complete paralysis of the eye, when it cannot perform horizontal or vertical movements. More often diagnosed in older people.
- Internuclear form. Characterized by pathological disruption of nerve connections. The eyeballs deviate in different directions, one eye is limited to internal movement, and the other has involuntary vibrations (nystagmus). This type of disease often appears in multiple sclerosis at a young age.
In severe cases of the disease, total ophthalmoplegia is observed, when the gaze is completely paralyzed, and the ability to move the gaze is absent. Along with it, diabetic ophthalmoplegia is distinguished, which is characterized by an acute course with severe headaches and paresis. In this case, diabetes occurs in a latent form.
With Tolosa-Hunt syndrome, painful ophthalmoplegia is diagnosed, which causes inflammatory processes in the vessel wall.
Diagnostics
The initial diagnosis is made during an external visual examination of the visual organ by a specialist. In this case, a dilated pupil, asymmetrical eye movement, redness or swelling are detected.
After this, additional studies are carried out to confirm the disease:
- perimetry - with its help the boundary of the field of view is determined (in the external form of the disease it is narrowed);
- visometry – it is used to measure visual acuity (internal ophthalmoplegia causes visual dysfunction);
- computed tomography – helps examine the brain and orbital cavity for abnormalities;
- ultrasound diagnostics - allows you to examine the orbital cavity and detect abnormalities in the eyeball;
- angiography of the head - reveals aneurysm in the vessels, thrombosis and other pathological disorders in the brain;
- proserine test - if the result is negative, ophthalmoplegia is diagnosed;
- X-ray examinations of the skull for hidden traumatic brain injuries, checking the condition of the bones.
If, as a result of the research, the presence of neoplasms is detected, the patient is referred to an oncologist, who will prescribe the following tests: blood donation for biochemistry, general analysis, analysis of hormones, sugar and tumor markers.
After this, the patient is prescribed treatment in accordance with the type and causes of the disease.