Introductory part
Exam questions:
1.7. Segmental apparatus of the spinal cord: anatomy, physiology, symptoms of damage.
1.8. Spinal cord pathways: symptoms of damage.
1.9. Cervical thickening of the spinal cord: anatomy, physiology, symptoms of damage.
1.10. Syndromes of damage to the diameter of the spinal cord (transverse myelitis syndrome, Brown-Séquard).
1.11. Lumbar enlargement, conus spinal cord, cauda equina: anatomy, physiology, symptoms of damage.
1.12. Medulla oblongata: anatomy, physiology, symptoms of damage to the caudal group (IX, X, XII pairs of cranial nerves). Bulbar and pseudobulbar palsy.
1.15. Cortical innervation of the motor nuclei of cranial nerves. Symptoms of damage.
Practical skills:
1. Taking anamnesis in patients with diseases of the nervous system.
4. Study of cranial nerve function
Anatomical and physiological features of the spinal cord
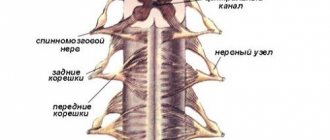
The spinal cord is anatomically a cylindrical cord located in the spinal canal, 42-46 cm long (in an adult).
1. Structure of the spinal cord (at different levels)
– The structure of the spinal cord is based on the segmental principle (31-32 segments): cervical (C1-C8), thoracic (Th1-Th12), lumbar (L1-L5), sacral (S1-S5) and coccygeal (Co1-Co2) . Thickenings of the spinal cord : cervical (C5-Th2, provides innervation to the upper extremities) and lumbar (L1(2)-S1(2), provides innervation to the lower extremities). Due to its special functional role (location of the segmental center for regulating the function of the pelvic organs - see lesson No. 2.), a cone (S3-Co2) is distinguished.
– Due to the peculiarities of ontogenesis, the spinal cord of an adult ends at the level of the LII vertebra; below this level, the roots form the cauda equina (roots of segments L2-S5) .
– Correlation of spinal cord segments and vertebrae ( skeletotopy ): C1-C8 = C I -C VII , Th1-Th12 = ThI-ThX, L1-L5 = ThXI-ThXII, S5-Co2 = LI-LII.
– Places where the roots emerge : C1-C7 – above the vertebra of the same name, C8 – under C VII, Th1-Co1 – under the vertebra of the same name.
– Each segment of the spinal cord has two pairs of anterior (motor) and posterior (sensitive) roots. Each dorsal root of the spinal cord contains a spinal ganglion. The anterior and posterior roots of each side fuse to form the spinal nerve.
2. Structure of the spinal cord (cross section)
– Gray matter of the spinal cord: located in the center of the spinal cord and resembles a butterfly in shape. The right and left halves of the gray matter of the spinal cord are connected to each other by a thin isthmus (median intermediate substance), in the center of which the opening of the central canal of the spinal cord passes. Histologically, the following layers are distinguished: 1 - marginal; 2-3 - gelatinous substance; 4-6 - proper nuclei of the posterior horns; 7-8 - nucleus intermedius; 9 - motor neurons of the anterior horns.
1) dorsal horns (columns) of the SC: bodies of II neurons of the superficial sensitivity pathways and the cerebellar proprioception system
2) lateral horns (columns) of the SC: segmental autonomic efferent neurons - sympathetic (C8-L3) and parasympathetic (S2-S4) nervous system.
3) anterior horns (columns) of the SC: cells of the motor (alpha large motor neurons, Renshaw inhibitory cells) and extrapyramidal (alpha small motor neurons, gamma neurons) system.
– White matter of the spinal cord: located on the periphery of the spinal cord, myelinated fibers pass here, connecting the segments of the spinal cord with each other and with the centers of the brain. The white matter of the spinal cord is divided into posterior, anterior and lateral cords.
1) posterior cords of the SC: contain ascending conductors of deep sensitivity - medial (fasc.gracilis, thin, Gaulle, from the lower extremities) and lateral (fasc.cuneatus, wedge-shaped, Burdacha, from the upper extremities).
2) lateral cords of the SC: contain descending : 1) pyramidal (lateral corticospinal tract), 2) red nucleus-spinal cord (dorsolateral extrapyramidal system); and ascending pathways : 1) spinocerebellar (along the lateral edge of the lateral cords) - anterior (Goversa) and posterior (Flexiga), 2) lateral spinothalamic (laterally - temperature, medially - pain).
3) anterior cords of the SC: contain descending: 1) anterior pyramidal (Turk's bundle, uncrossed), 2) vestibulospinal (ventromedial extrapyramidal system), 3) reticulospinal (ventromedial extrapyramidal system) ; 4) olivospinal , 5) tectospinal ; and ascending pathways : 1) anterior spinothalamic (laterally - touch, medially - pressure), 2) dorso-olivary (proprioceptive, to the inferior olive), 3) dorso-tegmental (proprioceptive, to the quadrigeminal).
Brain compression
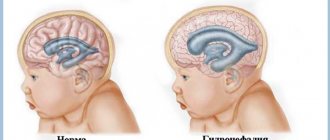
The clinical picture of brain compression depends on the etiology, localization of the compressive formation, its size and rate of increase, as well as on the compensatory abilities of the brain. Pathognomonic for most post-traumatic hematomas and hygromas is the presence of the so-called. “bright interval”, when the victim is conscious without showing signs of severe brain damage. The duration of the light interval can vary from minutes to 36-48 hours. Subarachnoid hemorrhage and the formation of a subdural hematoma can be accompanied by a clear interval lasting up to 6-7 days. In cases of severe brain damage (severe brain contusion, axonal damage), the lucid interval is usually absent.
Acute compression of the brain usually manifests itself with repeated vomiting, persistent intense headache and psychomotor agitation with sleep disturbance, sometimes delusional and/or hallucinatory syndromes. Later, the excitement turns into general inhibition, manifested by apathy, lethargy, and lethargy. There is a disturbance of consciousness that progresses from stupor to coma. Diffuse inhibition in the central nervous system is accompanied by respiratory and cardiovascular disorders, which are also caused by the resulting mass effect. The latter is a displacement of cerebral structures towards the foramen magnum, occurring due to increased intracranial pressure. The result is prolapse and infringement of the medulla oblongata in the foramen magnum with disruption of the centers located in it that regulate respiratory and cardiac activity.
There is a disorder in the breathing rhythm. Tachypnea (increased breathing) reaches 60 per minute, accompanied by noisy inhalation and exhalation, Cheyne-Stokes respiration is observed. Heart rate gradually decreases, bradycardia reaches 40 beats/min. and below, the blood flow rate drops significantly, and arterial hypertension is observed. Congestive pneumonia and pulmonary edema develop in the lungs. On auscultation, multiple moist rales are heard. The skin of the limbs and face becomes cyanotic. Body temperature rises to 40-41°C. Meningeal symptoms are detected. In the terminal stage, tachycardia and arterial hypotension appear. The pulse becomes thread-like, episodes of apnea (breath holding) appear, the duration of which increases.
In parallel, against the background of general cerebral symptoms, focal symptoms arise and worsen. They entirely depend on the topic of the pathological process. On the side of the lesion, drooping of the upper eyelid, diplopia, strabismus, mydriasis, central facial paresis (facial asymmetry, lagophthalmos, “sailing” cheek) are possible; on the opposite side (heterolateral) - paresis, paralysis, tendon hypo- or areflexia, hypoesthesia. Epileptic seizures, hormetonic convulsions (paroxysms of muscular hypertension), tetraparesis, coordination disorders, bulbar syndrome (dysarthria, swallowing disorders, dysphonia) may occur.
Spinal cord syndromes
1. Syndromes of SM lesions (across the diameter):
– anterior horn – 1) peripheral paralysis in the muscles of this segment (decreased strength, and reflexion (interruption of the efferent link), and tone (rupture of the gamma loop), and muscle trophy) + 2) fascicular twitching;
– posterior horn – 1) dissociated sensitivity disorder (loss of the superficial while maintaining the deep) on the affected side in the segment zone (“half-jacket”) + 2) areflexia (interruption of the afferent link);
– lateral horn – 1) impaired sweating, pilomotor, vasomotor and trophic disorders in the segment area;
– anterior gray commissure – 1) dissociated sensitivity disorder (loss of superficial while maintaining deep) on both sides in the segment area (“jacket”);
– posterior funiculi – 1) loss of deep sensitivity (posture, locomotion, vibration) ipsilateral + 2) sensory ataxia ipsilateral;
– lateral cords – 1) central paresis ipsilaterally (with bilateral lesions - dysfunction of the pelvic organs according to the central type) + 2) disturbance of temperature and pain sensitivity according to the conduction type contralaterally (2 segments below the upper border of the lesion - precrossing is carried out at the level of 2 segments) ;
– anterior spinal artery (Preobrazhensky) – damage to the anterior 2/3 of the spinal cord;
– half lesion of the SC (Brown-Séquard) – 1) loss of superficial sensitivity ipsilaterally at the level of the segment, contralaterally - 2-3 segments lower according to the conductor type, 2) loss of deep sensitivity ipsilaterally from the level of the lesion, 3) peripheral paresis ipsilaterally at the level of the segment , central paresis ipsilaterally below the level of the lesion, 4) trophic disorders ipsilaterally at the level of the segment.
– complete transverse lesion of the SM : 1) loss of superficial sensitivity from the level of the lesion, 2) loss of deep sensitivity from the level of the lesion, 3) peripheral paresis at the level of the segment, central paresis below the level of the lesion, 4) autonomic disorders
2. Syndromes of complete transverse lesion of the SM at different levels (Geda-Riddoha, along the length):
– craniospinal:
1) sensitive area: a) conduction type anesthesia of the spinal version on both sides in the caudal zones of Zelder, on the back of the head, arms, body and legs, b) pain and paresthesia in the back of the head;
2) motor sphere: a) central tetraparesis, b) breathing disorders (diaphragm);
3) central pelvic disorders;
4) vegetative sphere: Bernard-Horner syndrome (damage to the descending sympathetic pathway from the hypothalamus (body I)) - vegetative ptosis (narrowing of the palpebral fissure), miosis, enophthalmos;
5) damage to the caudal group of cranial nerves;
6) intracranial hypertension.
– upper cervical segments ( C2- C4) :
1) sensitive area: conduction type anesthesia in the spinal version on both sides on the back of the head, arms, body and legs;
2) motor sphere: a) tetraparesis (VC-mixed, NC-central), b) breathing disorders (diaphragm paralysis) or hiccups (C4);
3) central pelvic disorders;
4) vegetative sphere: Bernard-Horner syndrome (damage to the path from the hypothalamus);
– cervical thickening ( C5- Th1) :
1) sensitive sphere: according to the conductive type in the spinal version on both sides on the arms, body and legs;
2) motor sphere: tetraparesis (VC-peripheral, NC-central);
3) central pelvic disorders;
4) vegetative sphere: a) Bernard-Horner syndrome (damage to the ciliospinal center - lateral horns C8-Th1, body of the II sympathetic tract); b) vegetative disorders on the VC,
– thoracic region ( Th2- Th12):
1) sensitive sphere: conductive type, spinal version on both sides on the body and legs;
2) motor sphere: central lower paraparesis;
3) central pelvic disorders;
4) vegetative sphere: a) autonomic disorders on the VC, b) cardialgia (Th5).
– lumbar thickening ( L1- S2):
1) sensitive sphere: conductive type, spinal version on both sides on the legs (paraesthesia) and in the perianal area;
2) motor sphere: peripheral lower paraparesis;
3) central pelvic disorders;
4) vegetative sphere: autonomic disorders in the NK.
– epicone ( L4- S2) :
1) sensitive sphere: according to the conductive type, spinal version on both sides in the perianal region and along the back surface of the thigh, legs;
2) motor sphere: peripheral paresis of the feet (loss of the Achilles reflex);
3) central pelvic disorders;
4) vegetative sphere: autonomic disorders in the NK.
– cone ( S3- Co2) :
1) sensitive area: anesthesia in the perianal area on both sides;
2) motor sphere: peripheral paresis of the perineal muscles;
3) peripheral pelvic disorders (incontinence, paradoxical ischuria);
4) vegetative sphere: autonomic dysfunction of the pelvic organs.
– cauda equina (roots L2- S5):
1) sensitive area: a) PAIN SYNDROME IN THE AREA OF THE SADDLE and LEGS, b) asymmetrical anesthesia in the area of the saddle and legs on both sides;
2) motor sphere: peripheral paresis of the muscles of the NK and perineum (L2-S5);
3) peripheral pelvic disorders (incontinence).
3. Syndromes of compression lesions of the SM:
– intramedullary: 1) more often in the area of thickenings, 2) rapidly progresses, 3) descending type of flow.
– extramedullary: 1) more often in the thoracic region or cauda equina, 2) slowly progresses, 3) ascending type of flow, 4) block of cerebrospinal fluid flow, 5) changes in the cerebrospinal fluid (xanthochromia, protein-cell dissociation), 6) changes in the spine (destruction, positive bell symptom).
Diseases of the medulla oblongata
Since the volume of the medulla oblongata is small, the anatomical structure and the numerous functions it performs are very complex, even small foci of its damage cause various clinical symptoms, most often bilateral. In diseases of the medulla oblongata, dysfunctions of the IX-XII pairs of cranial nerves, pyramidal motor disorders, sensitivity disorders on the face, trunk and limbs, disorders of cerebellar functions, breathing, vasomotor apparatus, cardiac activity and some other disorders of autonomic functions are observed. The most typical is bulbar syndrome, in which paralysis of the cranial nerves, the nuclei of which are located in the medulla oblongata, comes to the fore (see Bulbar palsy).
Lesions of the pyramidal tract at the level of the medulla oblongata cause hemiplegia or quadriplegia. Crossover paralysis rarely occurs as a result of damage to the pyramidal tract at the level of its decussation; in this case, paralysis of the arm on one side is combined with paralysis of the leg on the opposite side. Paralysis is spastic in nature. Often, lesions of the pyramidal tract involve the nuclei and roots of the IX-XII pairs of cranial nerves. In this case, paralysis of one or more cranial nerves occurs on the side of the lesion, and hemiplegia occurs on the opposite side, for example, peripheral paralysis of the hypoglossal nerve on the affected side and hemiplegia of the opposite limbs [Jackson syndrome (see Alternating syndromes)]. Cerebellar disorders in lesions of the medulla oblongata are expressed in the form of hemiataxia, hemiasynergia and other cerebellar symptoms on the side of the lesion (see Cerebellum). Pain and thermal sensitivity of the trunk and limbs on the side opposite to the lesion is usually impaired; at the same time, tactile sensitivity and deep muscle feeling remain intact. If the fibers coming from the nuclei of the posterior columns are affected, then a disorder of deep sensitivity occurs. Sensory disorders of the face depend on damage to the descending root of the trigeminal nerve and are usually found on the affected side.
The medulla oblongata is often affected by vascular, infectious and tumor diseases of the nervous system. Hemorrhages in the medulla oblongata, leading to the rapid death of the patient, are rarely observed. Softening of the medulla oblongata is more common. Zakharchenko-Wallenberg syndrome, which belongs to the group of alternating syndromes, is characteristic. The medulla oblongata is affected by polio more often than by other infectious diseases. Often, lesions of the IX-XII pair of cranial nerves are combined with nystagmus and, even more often, with lesions of the spinal cord. Poliomyelitis affecting the medulla oblongata is especially dangerous, as it can lead to the death of the patient due to respiratory paralysis.
Syphilitic endarteritis of small vessels of the medulla oblongata can also cause its damage. Often the pyramidal tract is predominantly affected, and hemi- and tetraparesis of a spastic nature often occurs. Sometimes damage to the caudal group of cranial nerves at the base of the brain simulates bulbar palsy. With botulism, speech and swallowing disorders are observed. The symptom of delayed saliva secretion is especially important.
Syringobulbia usually occurs when the process of cavity formation and clay proliferation spreads from the cervical spinal cord (see Syringomyelia). Very rarely the process is limited only to the medulla oblongata. With syringobulbia, first of all, signs of damage to the spinal root of the trigeminal nerve appear - disturbances in pain and thermal sensitivity on the face in the form of concentric circles (Zelder zones). These disorders first appear in the lower jaw area, the last areas to be affected are the lips and the tip of the nose. In advanced cases, along with symptoms of dysfunction of the IX-XII pairs of cranial nerves, ataxia, nystagmus, vestibular and cerebellar disorders, and sometimes autonomic crises in the form of attacks of vomiting, tachycardia, and breathing disorders are observed.
Amyotrophic lateral sclerosis (see) often ends in bulbar palsy. Less commonly, the disease begins with bulbar symptoms and proceeds as isolated bulbar palsy. The process progressively increases, affects only the motor nuclei of the bulbar nerves and can spread to the nuclei of the facial nerves and the motor nuclei of the trigeminal nerve.
Tumors of the medulla oblongata - most often astrocytomas, spongioblastomas, rarely gangliocytomas, arachnoendotheliomas, tuberculomas (see Brain, tumors). They are characterized by pain in the back of the head, attacks of vomiting and hiccups. Isolated lesions of the cranial nerves due to their close proximity are rare. Sooner or later, paralysis of the limbs occurs, which are usually bilateral. Signs of increased intracranial pressure appear late or are not observed at all, so the tumor is often mistaken for brainstem encephalitis. Sudden death may occur before the tumor reaches significant size. When the tumor penetrates into the fourth ventricle, congestive papillae of the optic nerves and other signs of increased intracranial pressure appear early.
Syndrome of damage to the medulla oblongata can occur due to its compression by a space-limiting process in the posterior cranial fossa. These include tuberculosis (caries) of the I and II cervical vertebrae or occipital bone, aneurysms of the vertebral and basilar arteries, gummous meningitis, and tumors.
Understanding the Brain Stem
1. Structural division of the brain stem:
— vertically:
1) medulla oblongata;
2) pons;
3) midbrain.
— horizontally:
1) base : descending tracts (corticospinal, corticobulbar, corticopontine)
2) tire ( tegmentum) :
1) ascending pathways (spino- and bulbothalamic, deep sensory pathways, medial lemniscus, lateral lemniscus),
2) nuclei of cranial nerves,
3) reticular formation,
4) specific formations.
3) roof ( tectum) : specific formations.
2. Features of the structure of cranial nerve systems (source in ontogenesis):
— Pre-auricular somites:
1) afferent part – optic nerve (II),
2) efferent part - oculomotor nerve (III),
3) vegetative (parasympathetic) part – Yakubovich nuclei + ciliary ganglion.
— Gill somites (1 – maxillary, 2 – facial, 3 – glossopharyngeal, 4 – vagus):
1) afferent part – upper and lower jaw nerve, ophthalmic nerve (branches V),
2) efferent part – lower jaw nerve (branch V), facial nerve (VII), glossopharyngeal nerve (IX),
3) autonomic (parasympathetic) part - salivary and dorsal nucleus + pterygopalatine, submandibular, auricular ganglion, vagus ganglion.
3. Diagram of the motor pathway of cranial nerves
- lower part of the anterior central gyrus of the cerebral cortex (body I) - tractus corticonuclearis - decussation directly above the motor nuclei ( 1.5 nuclei rule ):
1) to the nuclei of 3,4,5,6,9,10,11 pairs of cranial nerves, the corticonuclear pathway makes an incomplete crossover (bilateral innervation)
2) to the nuclei 7 (lower part) and 12 pairs of cranial nerves, the corticonuclear pathway makes a complete decussation (rule of 1.5 nuclei)
- nuclei of the brain stem (body II) - motor portion of the cranial nerve - striated muscles.
4. Diagram of the sensory pathway of the cranial nerves
- extero- or proprioceptor - cranial nerve;
- cranial ganglion (body I) - sensitive portion of the cranial nerve;
- sensory nucleus of the brain stem homolaterally (body II) - chiasm contralaterally (directly above the nucleus) - sensory tract as part of the medial lemniscus;
- ventrolateral nucleus of the thalamus (body III) - thalamocortical pathway - through the posterior third of the posterior limb of the internal capsule - corona radiata;
— the lower parts of the posterior central gyrus and the superior parietal region.
Brain stem: etiological factors of damage
1. Diseases that occur with selective damage to the gray matter of the trunk (nuclei of the cranial nerves):
- polioencephalitis (VII, IX, X, XI, XII): poliomyelitis, poliomyelitis-like diseases (Coxsackie, Eckho), West Nile fever,
- neurodegenerative diseases: motor neuron disease (progressive bulbar palsy)
- hereditary diseases and syndromes: Fazio-Londe syndrome (VII, VI, IV, III), Kennedy spinal amyotrophy
2. Diseases that occur with selective damage to the white matter of the trunk:
- autoimmune diseases: multiple sclerosis,
— dysmetabolic diseases: central pontine myelinolysis
— hereditary diseases and syndromes: hereditary spastic paraplegia, spinocerebellar atrophy
3. Diseases that occur with damage to the white and gray matter of the trunk:
- cerebrovascular accidents
— inflammatory diseases: ADEM
- injuries
- tumors
Anatomical and physiological features of the medulla oblongata
The medulla oblongata in the oral section borders on the pons of the brain (cerebellopontine angle), and in the caudal section on the spinal cord (the conventional lower edge of the medulla oblongata - the decussation of the pyramids, the exit point of the C1 root, the upper edge of the first segment of the spinal cord). In the middle of the ventral part there is the main groove, where the a.basilaris passes, the dorsal part makes up the bottom of the IV ventricle (the lower part of the rhomboid fossa).
1. Components:
- base ( basis) - pyramidal path (pyramids) and lower olives;
- tire ( tegmentum) :
1) ascending pathways: spinothalamic tracts; paths of deep sensitivity -> nuclei of Gaul (nucl.gracilis) and Burdach (nucl.cuneatus) -> medial loop,
2) nuclei of cranial nerves (IX-XII),
3) reticular formation (vasomotor, respiratory, swallowing center, center for regulating muscle tone, sleep center [synchronization of brain activity - hypnogenic effect]);
- roof ( tectum) - not prominent (posterior medullary velum).
2. Cranial nerves
— XII pair — N. Hypoglossus
1) Nuclei XII pair and function:
- motor - nucl.nn.hypoglossi (body II - muscles of the tongue)
2) The exit from the brain is the ventromedial sulcus (between the olive and the pyramid),
3) Exit from the skull – canalis nn.hypoglossi
4) Prolapse syndromes:
- supranuclear type (body and axon of the first neuron) - deviation in the opposite direction from the focus, dysarthria (central paralysis);
- nuclear type (body of the second neuron) - deviation towards the focus, dysarthria, tongue atrophy, fasciculations (peripheral paralysis);
- radicular type (axon of the II neuron) - deviation towards the focus, dysarthria, tongue atrophy (peripheral paralysis);
6) Research methods:
- complaints: dysarthria,
- status: 1) position of the tongue in the oral cavity and 2) when protruding, 3) the presence of atrophy (hypotrophy) and fibrillar twitching in the muscles of the tongue
— XI pair — N. Accessorius
1) Cores XI pairs and function:
- motor - nucl.nn.accessorii (body II - trapezius and sternocleidomastoid muscles)
2) Exit from the brain - ventrolateral sulcus (dorsal to the olive),
3) Exit from the skull – from the skull – for.jugulare.
4) Prolapse syndromes:
- nuclear (body of the second neuron) - inability to raise the arm above the horizontal, difficulty turning the head in the direction opposite to the lesion, lowering of the shoulder (with bilateral damage - “dropping” head), fasciculations in these muscles (peripheral paralysis);
- radicular type (axon of the II neuron) - inability to raise the arm above the horizontal, difficulty turning the head in the direction opposite to the lesion, lowering the shoulder (peripheral paralysis);
5) Irritation syndromes:
- motor portion - attacks of clonic and nodule spasms (Salaam's spasm), spastic torticollis
6) Research methods:
- complaints: impaired movement of the head and arms,
- status: 1) position of the shoulders, shoulder blades and head at rest and 2) movement, 3) tension of the sternocleidomastoid and trapezius muscles.
— X pair — N. Vagus
1) X pair cores and function:
- motor - nucl.ambiguus (body II - muscles of the pharynx and larynx)
- sensitive - nucl.solitarius (body II for taste sensitivity - epiglottis), nucl. alae cinerea (body II for interoceptive sensitivity - from chemo- and baroreceptors)
- vegetative - nucl.salivatorius inferior (parotid salivary gland), nucl.dorsalis nn.vagi (internal organs)
2) Exit from the brain - ventrolateral sulcus (dorsal to the olive),
3) Exit from the skull – for.jugulare (forms 2 ganglia - upper (special sensitivity) and lower (taste, peritoneum)).
4) Prolapse syndromes:
- nuclear (body of the II neuron) and radicular type (axon of the II neuron) - dysphagia, dysphonia, decreased pharyngeal reflex, anesthesia of the pharynx, trachea, dry mouth, tachycardia, gastrointestinal dysfunction
- neuropathy of the recurrent laryngeal nerve (dysphonia)
5) Irritation syndromes:
- vegetative portion - attacks of cardiac arrhythmia, bronchospasm, laryngospasm, pylorospasm, etc.
— neuralgia of the superior laryngeal nerve: 1) attacks of intense, short-term pain in the larynx and cough + 2) trigger zone under the thyroid cartilage (hyperesthesia zone, touching which provokes an attack of pain)
— IX pair - N. Glossopharyngeus
1) Cores IX pairs and function:
- motor - nucl.ambiguus (body II - muscles of the pharynx and larynx)
- sensitive - nucl.solitarius (body II for taste sensitivity - posterior 1/3 of the tongue), nucl. alae cinerea (body II for interoceptive sensitivity - from chemo and baroreceptors)
- vegetative - nucl.salivatorius inferior (parotid salivary gland)
2) Exit from the brain - ventrolateral sulcus (dorsal to the olive),
3) Exit from the skull - for.jugulare (forms 2 ganglia - upper - (special sensitivity) and lower (taste).
4) Prolapse syndromes:
- nuclear (damage to the body of the II neuron) and radicular type (damage to the axons of the II neuron) - dysphagia, dysphonia, decreased pharyngeal reflex, anesthesia of the pharynx, ageusia of the posterior 1/3 of the tongue, dry mouth
5) Irritation syndromes:
- sensitive portion - neuralgia of the glossopharyngeal nerve - 1) attacks of intense, short-term pain in the pharynx, tongue, tonsil, external auditory canal + 2) trigger zones (areas of hyperesthesia, touching which provokes an attack of pain)
6) Research methods:
- complaints: 1) pain and paresthesia in the pharynx, 2) loss of taste, 3) impaired phonation, articulation, swallowing,
- status: 1) Position and mobility of the soft palate and uvula at rest and 2) when pronouncing sounds, 3) swallowing, 4) articulation, 5) salivation, 6) taste sensitivity, 7) pharyngeal reflex.
Syndromes of damage to the medulla oblongata.
The medulla oblongata is a continuation of the spinal cord and has structural features similar to it - it consists of pathways and nuclei. In front it borders with the pons of the brain, and behind it, without a clear boundary, it passes into the spinal cord (conventionally, the lower edge of the medulla oblongata is considered to be the decussation of the pyramids or the upper border of the first cervical spinal roots).
On the ventral surface of the medulla oblongata there is an anterior median fissure, on its sides there are pyramids. Outside the pyramids are the inferior olives, separated from them by a lateral anterior groove. On the dorsal surface of the medulla oblongata, below the rhomboid fossa, the posterior funiculi (gracilis and wedge-shaped fascicles) are distinguishable, separated by an unpaired posterior medial sulcus and paired posterolateral sulci. The dorsal surface of the anterior medulla oblongata forms the floor of the ventricle (posterior corner of the rhomboid fossa). Outward from these edges, the lower cerebellar peduncles can be traced on the lateral surface of the medulla oblongata.
On a cross section of the medulla oblongata, the pyramidal tract passes through its ventral section; in the central part, the fibers of the decussation of the medial lemniscus are located (conduct deep sensitivity impulses from the nuclei of the thin and cuneate fasciculi to the thalamus). The ventrolateral sections of the medulla oblongata are occupied by the inferior olives. Dorsal to them are ascending conductors that form the inferior cerebellar peduncles, as well as the spinothalamic fascicle. In the dorsal part of the medulla oblongata there are nuclei of the posterior group of cranial nerves (XX pair), as well as a layer of the reticular formation.
The nuclei of many cranial nerves are located in the floor of the fifth ventricle (the rhomboid fossa). At the level of the lower (posterior) angle there are the nuclei of the hypoglossal (medial) and vagus nerves (lateral). At the level of the outer corner of the rhomboid fossa, parallel to the median sulcus, lies the sensory nucleus of the trigeminal nerve, lateral to it are the vestibular and auditory nuclei, and medial is the nucleus of the solitary tract (taste nucleus of the glossopharyngeal and vagus nerves). Paramedian anterior to the nucleus of the hypoglossal nerve is the motor nucleus of the glossopharyngeal and vagus nerves and the salivary nuclei.
Syndromes of damage to the medulla oblongata : symptoms of dysfunction of the nuclei and roots of the X, X, X and X pairs of cranial nerves, inferior olive, spinothalamic tract, nuclei of the thin and cuneate fasciculi, pyramidal and descending extrapyramidal systems, descending sympathetic fibers to the ciliospinal center , posterior and anterior spinocerebellar tracts.
The main alternating syndromes are the following.
Avellis syndrome: peripheral paralysis of half the tongue, soft palate and vocal cord (X, X, X pairs of cranial nerves) on the side of the lesion and hemiplegia on the opposite side; develops with a focus in one half of the medulla oblongata.
Jackson syndrome: peripheral paralysis of the tongue on the side of the lesion and central paralysis of the opposite limbs occurs when one pyramid of the medulla oblongata and the root of the X pair of cranial nerves are affected.
Wallenberg-Zakharchenko syndrome: damage to the vagus nerve on the side of the lesion (unilateral paralysis of the soft palate, vocal cord, swallowing disorder; on the same side the Bernard-Horner symptom, cerebellar ataxia, facial anesthesia, dissociated anesthesia on the opposite side (alternating hemianesthesia); occurs in case of circulatory disorders in the vertebral or the inferior posterior cerebellar artery extending from it; the ischemic focus is located in the dorsolateral part of the medulla oblongata.
Schmidt's syndrome: on the side of the lesion, paresis of the vocal cord, soft palate, trapezius and sternocleidomastoid muscles; on the opposite side - spastic hemiparesis, i.e. the nuclei and fibers of the IX, X, XI, XII pairs of cranial nerves and the pyramidal system are affected.
Tapia syndrome: on the side of the lesion, paralysis of the trapezius, sternocleidomastoid muscles (accessory nerve) and half of the tongue (hypoglossal nerve), contralateral spastic hemiparesis.
Voplestein's syndrome; on the side of the lesion, paresis of the vocal cord due to damage to nucl. ambiguus, contralaterally - hemianesthesia of superficial sensitivity (spino-thalamic tract).
Babinsky-Nageotte syndrome: on the side of the lesion - cerebellar symptoms (ataxia, nystagmus, asynergia), Claude Bernard-Horner syndrome, hyperthermia; contralateral spastic hemiparesis, dissociated hemianesthesia (loss of pain and temperature sensitivity); the syndrome is caused by damage to the posterolateral part of the medulla oblongata and the pons.
Glick syndrome: characterized by combined damage to the V, V, X nerves and pyramidal system; on the side of the lesion - blurred vision (or amaurosis), pain in the supraorbital region, paresis of facial muscles, difficulty swallowing; contralaterally - spastic hemiparesis.
With bilateral damage to the nuclei and roots of the X, X and X pairs of cranial nerves, bulbar palsy develops. It is characterized by impaired swallowing (choking, liquid food getting into the nose), changes in the sonority of the voice (hoarseness, aphonia), the appearance of a nasal tone of speech (nasolalia), and dysarthria. Atrophy and fascicular twitching of the tongue muscles are observed. The pharyngeal reflex disappears. This syndrome most often occurs with vascular and some degenerative diseases (amyotrophic lateral sclerosis, syringobulbia).
Pseudobulbar palsy is a central paralysis of the muscles innervated by the X, X, X pairs of cranial nerves. Develops with bilateral damage to the corticonuclear pathways. The lesions are located at different levels above the medulla oblongata, including the brain stem. Clinical manifestations are similar to those of palpebral palsy (impaired swallowing, nasal tone of voice, dysarthria). With pseudobulbar paralysis, reflexes of oral automatism (proboscis, palmar-mental, tongue-labial, etc.), violent laughter and crying appear. There are no signs of peripheral neuron damage (atrophy, fascicular twitching, etc.). The syndrome is most often associated with vascular lesions of the brain.
Thus, pathological lesions in the brain stem may involve the pyramidal system and the motor nuclei of the cranial nerves. In addition, this may damage sensory conductors, as well as the nuclei and roots of sensory cranial nerves. At the same time, the brain stem contains nerve formations that have activating and inhibitory effects on large areas of the brain and spinal cord. This refers to the function of the reticular formation of the brain stem. It has extensive connections with the lower and higher parts of the brain. Numerous collaterals from specific sensory pathways approach the reticular formation. Impulses pass through it, which tone the cortex and subcortical formations and ensure their activity and the awake state of the brain. Inhibition of ascending activating influences leads to a decrease in cortical tone and the onset of drowsiness or true sleep. Along descending pathways, the network-like formation sends impulses that regulate muscle tone (increases or decreases).
The reticular formation contains separate areas that have a certain specialization of functions (respiratory, vasomotor and other centers). The reticular formation is involved in maintaining a number of vital reflex acts (breathing, cardiovascular activity, metabolism, etc.). When the brain stem is damaged, especially the medulla oblongata, in addition to those described above, one also encounters such severe symptoms as respiratory and cardiovascular disorders.
When the function of the reticular formation is impaired, sleep and wakefulness disorders develop.
Narcolepsy syndrome: attacks of the patient’s uncontrollable desire to fall asleep in a completely inappropriate environment (during a conversation, eating, while walking, etc.); paroxysms of narcolepsy are often combined with paroxysmal loss of muscle tone (cataplexy), which occurs during emotions, which leads to immobility of the patient for several seconds or minutes; sometimes there is an inability to actively move for a short period of time immediately after awakening from sleep (awakening cataplexy, or “night paralysis”).
There is another type of sleep disorder - “periodic hibernation” syndrome: sleep attacks lasting from 10-20 hours to several days, Kleine-Levin syndrome: attacks are accompanied by bulimia. Thus, the reticular formation may participate in the formation of syndromes that occur when the lesion is localized not only in the brainstem, but also in other parts of the brain. This emphasizes the existence of close functional connections based on the principle of neuronal circles, including cortical, subcortical and brainstem structures.
With pathological foci outside the brain stem (extratruncally), several closely located nerves may suffer, and characteristic syndromes arise. Among them, it is important to note the cerebellar-pontine angle syndrome - damage to the auditory, facial and trigeminal nerves. It is characteristic of neuroma of the fifth pair of cranial nerves and basal arachnoiditis.
Internal auditory canal syndrome (Lanitz syndrome): damage to the auditory nerve, noise in the ear, decreased hearing of the sound-perceiving type), facial nerve (peripheral paralysis of facial muscles, dry eyes, decreased taste in the anterior third of the tongue) on the side of the lesion; also occurs with neuroma of the fifth pair of cranial nerves.
Gradenigo-Lannois syndrome (syndrome of the apex of the temporal bone): pain in the zone of innervation of the trigeminal nerve (irritation of the trigeminal ganglion), paralysis of the external rectus muscle of the eye on the side of the lesion; appears with inflammation of the middle ear and with a tumor localized in the middle cranial fossa.
With the tumor nature of extratruncal lesions in subsequent stages of disease development, conduction disorders also occur due to compression of the brain stem.