Neuropathic pain that persists for a long period after an episode of herpetic infection with localization of rashes on the torso, head or limbs of a person negatively affects his general condition. With a favorable course, neuralgia caused by herpes zoster goes away on its own. Patients with severe pain that does not go away for a long time after the skin heals need specific therapy.
Neuropathic pain that persists for a long period after an episode of herpetic infection with localization of rashes on the torso, head or limbs of a person negatively affects his general condition.
Postherpetic neuralgia - what is it?
The development of herpes zoster occurs due to the restoration of the vital activity of the herpes zoster virus. Why recovery? Because our body has already encountered it. It is the herpes virus type 3 that causes the development of chickenpox, which most often affects children.
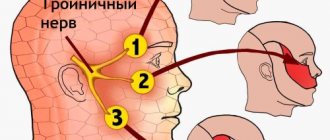
After contracting the disease, the chickenpox virus remains inside the body. It is contained in nerve ganglia, which are formed from nerve cells. As soon as the protective functions of our body weaken, the virus immediately reactivates and begins to reproduce. Nerve fibers and the surface of the epidermis are affected. Herpes zoster develops.
The average duration of the disease is 3-4 weeks. Symptoms are presented in the form of the formation of bubbles on the skin with liquid contents inside, their subsequent drying and hardening. After the crusts come off, pigment spots remain on the surface of the skin for some time. This whole process is accompanied by redness, itching, pain (to the point that it is impossible to touch the skin), burning, and intoxication.
Herpes zoster often disappears completely, but sometimes becomes a source of development of postherpetic neuralgia.
The essence of the disease is that herpes zoster (more precisely, its symptoms) has gone away, but the pain and burning sensation remain, moreover, in those places where signs of herpes were previously absent. Doctors associate the pathology with inflammation occurring in the nerve ganglia due to the rapid spread of the virus.
In this case, an imbalance occurs between the anti-pain systems in the body and the pain systems. As a result, disturbances occur in the nervous system. The mechanism responsible for the sensitivity of neurons that perceive pain impulses “breaks down.” In other words, the nerve fibers become overactive. The pain syndrome bothers me for no reason. A neurologist deals with the treatment and diagnosis of postherpetic neuralgia.
Herpes zoster - what is it?
Shingles (herpes) is the result of reactivation of the herpes virus type 3 (Varicella zoster). Reactivation, because the first encounter with this virus ends in the development of chickenpox for a person. After chickenpox, the virus hides in the nerve ganglia for life. When immunity decreases, it leaves the “shelter”, multiplies and causes damage to nerve conductors and skin, which is called herpes zoster.
Herpes zoster lasts about 3-4 weeks. The disease is characterized by the appearance of blisters on the skin, which then dry out and form crusts. When the crusts fall off, pigmentation remains for some time. The rashes are located in the area of the affected nerve ganglion: in the form of transverse stripes on the torso, longitudinal stripes on the limbs and in the zone of innervation of the cranial nerves on the face and head. Moreover, the very appearance of the rash and all stages of its development are accompanied by itching, burning, pain of varying intensity and nature (shooting, boring, dull and aching, burning, and so on), as well as increased temperature and intoxication. With a favorable outcome, shingles goes away without a trace. In some cases, it leaves behind postherpetic neuralgia. When does it occur and why? Let's find out.
Causes
The risk of postherpetic neuralgia increases mainly in older people over 60 years of age. After 70, the probability of developing the disease increases to 75%. In adolescents and middle-aged people, neuralgia is observed in only 10% of cases. This is due to the fact that in younger people, tissue regeneration occurs much faster than in older people.
The main provoking factors for the development of pathology include:
- weakened immunity, immunodeficiency states, diabetes mellitus, AIDS;
- location of the rash on the body;
- large size of the lesion increases the risk of postherpetic neuralgia;
- the intensity of the pain syndrome also leads to complications of herpes zoster;
- late intake of antiviral drugs.
The disease affects women more often than men. This fact has not yet been explained.
Symptoms
Postherpetic neuralgia is the same pain as with shingles that remains after the rash disappears. Pain syndrome manifests itself in different ways:
- Constantly – the pain is dull, pressing, sometimes combined with a burning sensation;
- periodically - the sensations have a shooting character;
- suddenly - usually this is allodynic pain, it can manifest itself even with a light touch of the skin, wearing clothes, and is accompanied by a strong burning sensation.
In addition to pain, other symptoms of postherpetic neuralgia are noted;
- itching;
- decreased physical activity;
- numbness;
- constant muscle weakness;
- tingling, sensation of “pins and needles”, presence of a foreign body on the body.
The disease is accompanied not only by pain, but also by signs of mental disorder:
- sleep problems;
- loss of appetite;
- fatigue, fatigue;
- feeling of anxiety, fear for your life;
- irritability;
- depression.
Painful sensations greatly harm the body and often lead to a decrease in social adaptation and disruption of the usual way of life (a person is not able to carry out usual activities and his or her job).
Clinical picture
Symptoms of the disease appear acutely. The pain is constant or paroxysmal along the intercostal spaces, intensifying with sudden movements of the body, coughing, sneezing. The pain is accompanied by burning, tingling, and numbness in the affected area. Unpleasant sensations can radiate to the heart, back, under the shoulder blade, or in the lower back. An objective examination of the patient reveals pain on palpation in the affected area, hyperesthesia, and local paresthesia. Characteristic is an increase in pain in the chest area with active movements of the body (bending, movement in the shoulder/acromial clavicular joints).
Treatment
To avoid having to treat postherpetic neuralgia later, treatment for herpes zoster should be started on time. If a rash appears, antiviral drugs containing acyclovir are prescribed. You need to take the medicine in the first 72 hours after the onset of symptoms of the disease. Antiviral drugs prevent further spread of the virus throughout the body and reduce the lesion. As a result, the development of complications is reduced to zero.
A thorough medical examination is required to make a correct diagnosis. The main diagnostic methods are laboratory tests. CT, MRI, ultrasound, and EMG are prescribed as differential diagnostics.
For the treatment of postherpetic neuralgia, medications and folk remedies are used.
What groups of drugs are prescribed to eliminate signs of the disease?
Anticonvulsants (Pregabalin, Gebalentin). "Gebalentin" is taken according to a certain scheme. This is necessary to determine the optimal dosage. On the first day, 300 mg of the drug is prescribed once a day. Then the dosage is doubled and divided into 2 doses - morning and evening. On the third day, the optimal amount is 900 mg (taken in the morning, at lunch and in the evening, 300 mg). Next, on days 4, 5, 6, you should drink 300 mg in the morning and afternoon, and 600 mg in the evening. On days 7, 8, 9, 10, the patient takes 300 mg in the morning and 600 mg in the afternoon and evening. And so on until the dosage increases to 3600 mg per day. When the symptoms go away, the patient should take the drug in maintenance dosages for some time - 600-1200 mg per day. Pregabalin is used in the treatment of neuralgia 2-3 times a day. The daily dosage is 150-300 mg. The downside of the drugs is their high price.
Citracyclic antidepressants. The most commonly prescribed drugs are Amitriptyline, Melipramine, Doxepin and Nortriptyline. Treatment of postherpetic neuralgia in older people is carried out with the help of "Nortriptyline", since it has a gentler effect on the body and is better tolerated. These drugs are prescribed to people in cases where the disease is combined with nervous excitability, anxiety, fears, phobias, and depression. Amitriptyline is prescribed in a dosage of 125 to 150 mg per day, Nortriptyline - from 25 to 100 mg.
Patches containing lidocaine (Versatic). Apply a lidocaine patch to the painful area for the whole day. It relieves pain and protects the skin from external influences, touching clothes and linen. Another plus is the complete absence of prohibitions on use (except for allergies to substances in the patch) and unwanted reactions.
Capsaicin. This is a component that is added to pain-relieving ointments (Nicoflex, capsaicin). Medical plasters are also impregnated with it. The substance is obtained from hot red pepper. It is not suitable for use by everyone, as severe burning and irritation of the skin may be felt after application. The effective mechanism of the component is to gradually block pain impulses. Capsaicin-based products are applied three times a day (more is possible), depending on the severity of the pain.
Opioid analgesics (Tramadol, Methadone, Morphine). Such drugs are prescribed only by a doctor and are indicated in cases of unbearable pain. Used for a short time to alleviate the patient's condition.
It is worth noting that conventional analgesics, such as Ibuprofen, do not relieve pain and do not help in the treatment of neuralgia.
The most effective non-traditional method is acupuncture. The procedure will help relieve even the most excruciating pain.
Traditional medicine for postherpetic neuralgia
There are also effective treatment methods with folk remedies. Here are the most commonly used ones:
- Juice is extracted from black radish. Rubbing is made on its basis. The same goes for oil made from garlic.
- Compresses from herbal decoctions - geranium, wormwood.
- Rubbing with ointments prepared from bee products.
- Treatment of the painful area with infusion of sleep herbs.
- Infusions of willow bark and moss are recommended for internal use.
PHN can also be treated at home by taking pine and salt baths.
Kinds
Types of pain with postherpetic neuralgia are divided into groups:
- periodic – pulsating, sharp, like an electric shock;
- persistent – with a burning sensation, pressing, accompanied by numbness of areas of the skin;
- allodynic – sudden, which appears in response to the touch of clothing or some other “frivolous” irritant and disappears quite quickly.
There are also several phases in the development of neuralgia:
- acute (when there were rashes on the skin);
- subacute (when the skin is cleared of sores), lasting an average of 3 months;
- postherpetic neuralgia itself lasts more than 4 months.
Prevention
To prevent the development of postherpetic neuralgia, herpes zoster should be treated as quickly as possible. This is the main preventive measure. In addition, today vaccination against chickenpox is actively practiced in all cities. It will not be able to completely eliminate the development of infection, but it will significantly reduce the severity of symptoms, yes.
Postherpetic neuralgia is difficult to treat. It’s better to warn her and neutralize her. To do this, you need to start treatment for herpes zoster on time. This will help reduce the likelihood of developing the disease. If it cannot be avoided, then you need to urgently contact a neurologist for diagnosis and treatment.
Recommendations for caring for rashes
Prodromal, characterized by general malaise, neuralgic pain of varying intensity, this lasts on average 2-4 days:
- Headache
- Low-grade body temperature, less often fever up to 39C
- Chills, weakness
- Dyspeptic disorders, gastrointestinal dysfunction
- Pain, itching, burning, tingling in the area of the peripheral nerves in the area where the rash will later appear.
- Most often, during an acute process, regional lymph nodes become painful and enlarged.
- In severe cases of the disease, urinary retention and other disorders of certain systems and organs may occur.
After the temperature decreases, other general intoxication disorders also weaken.
The time when rashes characteristic of shingles appear. The symptoms and nature of the rash depend on the severity of the inflammatory process. At first, the rashes look like pockets of pink spots 2-5 mm in size, between which there are areas of healthy skin.
- In the typical form of the disease, the next day, small, closely grouped vesicles and vesicles with transparent serous contents form in their place, which becomes cloudy after 3-4 days.
- In severe gangrenous form of herpes, the contents of the vesicles may be mixed with blood and black in color. Herpetic rashes have a wave-like course, as with chickenpox, that is, fresh rashes with vesicular elements appear at intervals of several days. The bubbles seem to crawl from one place to another, encircling the body, hence the name of this disease.
In mild forms of the inflammatory process, the transformation of skin nodules into pustules does not form and their ulceration does not occur, and the manifestation of herpes is also possible only of a neurological nature - pain without a rash, otherwise it is also called herpetic neuralgia and is often mistaken for manifestations of intercostal neuralgia, osteochondrosis or heart pain. And therefore, inadequate treatment may be prescribed.
While taking a shower (and doing this if you have herpes zoster is not prohibited), do not rub the rash. If possible, avoid taking baths with aromatic oils and salts.
Development of herpes zoster.
To reduce the severity of pain, you can apply cold to the affected areas, for example, a heating pad with ice. To relieve itching, it is recommended to make lotions with menthol or calamine.
If possible, keep the affected skin areas as unclothed as possible. It is better that contact with clothing is minimized, and contact with air, on the contrary, is maximized.
There is no need to lubricate the rash with brilliant green, iodine and other similar substances - you will recover longer. There will be no effect from topical use of antiviral ointments.
Remember 3 main rules:
- do not panic;
- do not self-medicate;
- consult a doctor promptly.
To reduce the severity of pain, you can apply cold to the affected areas, for example, a heating pad with ice.
Starting the fight against the virus in a timely manner allows you to quickly achieve positive results and prevent the development of complications. It is important that the treatment is carried out under the supervision of an experienced specialist. Otherwise, there is a high probability of developing complications.