The brain is one of the most important organs in the human body. It is often compared to the heart, but if the heart can be restored and restarted after clinical death, then the brain and its cells die once and for all. Nerve cells and endings are found in large numbers on the surface of the brain and they contact each other using synaptic connections. When cells die, new ones come to replace them and this is normal. Millions of cells die in the human body every day. With the development of an undesirable pathological process, the connection between them is lost, and a process occurs, which in medicine is called atrophy - this is a phenomenon associated with the death of many brain cells, leading to the development of a serious disease - dementia. There are quite a few reasons, but the World Health Organization has found that this phenomenon mainly affects people over 55 years of age, regardless of whether they are men or women.
Causes of neuron death
The death of brain cells is a process that occurs throughout a person’s life. Doctors say that at a young age it is not scary, since the body is young - the hereditary factor plays a role in this case. Elderly people, especially after 55 years, encounter this phenomenon much more often and are diagnosed several times more often. This may be due to the following reasons:
- A heart attack is a process of disruption of blood flow to the main heart muscle.
- Stroke is a process of disruption of blood flow to the brain (cerebrovascular accident).
- Industrial emissions, working conditions, ecology.
- Previous injuries.
- Heredity and genetic predisposition.
- Pregnancy period (mother's use of drugs, cigarettes, alcohol), lack of professionalism of doctors - gynecologists and obstetricians.
There are many reasons for the spread of this phenomenon. Currently, MRI and CT scans are increasingly detecting serious changes in the neurons of the brain.
Depression in cerebrovascular diseases
Table 1. Diagnostic criteria for depression according to ICD-10
Table 2. Antidepressants that do not have a negative effect on cognitive function
Introduction
Depression is one of the most common mental disorders in the population, which not only psychiatrists, but also doctors of other specialties have to deal with. According to epidemiological data, the risk of developing depression during life is up to 10% among men and up to 20% among women [1, 2]. Difficulties in diagnosing depression are due to the fact that many patients do not complain of an emotional nature, and often even deny the presence of depression or low mood when asked directly by the attending physician. In such cases, the reason for a patient to contact a clinician may be symptoms of a somatic nature: pain of various localizations or other unpleasant physical sensations, increased fatigue, and disturbed night sleep. Without assessing the patient's emotional state, these symptoms can cause significant diagnostic difficulties.
It is important for neurologists to understand that depression can be organic in nature, associated with local or diffuse brain damage. In such cases, emotional disorders are part of the general neurological deficit associated with brain damage. A classic example is Parkinson’s disease, in which emotional disorders are almost obligatory and often precede the development of motor symptoms [3]. At the same time, specific therapy for the disease affects the emotional sphere, and increased severity of depressive disorders can aggravate motor and cognitive symptoms. In this regard, when managing patients with extrapyramidal pathology, it is necessary to carefully analyze the emotional state of patients and, if appropriate, prescribe antidepressant therapy. Consultation with a psychiatrist for mild to moderate depression and the absence of suicidal thoughts is usually not required.
In recent years, more and more attention has been paid to another type of organic depression associated with vascular diseases of the brain. Stroke and chronic forms of cerebral circulatory failure are the most common neurological pathology [4]. This causes a significant prevalence of so-called vascular depression, which probably underlies some subjective neurological disorders characteristic of the initial stages of dyscirculatory encephalopathy [5]. A correct understanding of the nature of the patient’s complaints allows us to build a more justified strategy for helping these patients from a pathogenetic point of view and improve their quality of life.
Epidemiology of vascular depression
Depression is included in the spectrum of characteristic manifestations of vascular damage to the brain in both acute and chronic cerebrovascular accidents. According to epidemiological data, every third stroke patient develops a clinically significant decrease in mood. At the same time, two peaks in the incidence of depression stand out: the first weeks after a stroke and three months after it. According to some data, in the early onset of post-stroke depression, the factor of localization of brain damage plays a decisive role, while in delayed development, the degree of disability plays a decisive role. Thus, early post-stroke depression is likely to be predominantly organic in nature, while late post-stroke depression is reactive [6–12].
The prevalence of depression in chronic cerebrovascular insufficiency was studied by T.A. Yanakaeva. Based on a detailed analysis of the emotional and cognitive sphere of 30 patients diagnosed with dyscirculatory encephalopathy, it was shown that depression is observed in the majority of patients with chronic cerebrovascular insufficiency (63%). Moreover, in 60% of patients with depression, the severity of emotional disorders according to the International Classification of Diseases, 10th revision (ICD-10) was classified as mild to moderate, and in 40% - as severe [13].
T.G. Voznesenskaya analyzed the results of assessing the emotional status of 29 patients with initial and moderate stages of dyscirculatory encephalopathy. According to formalized scales, approximately 80% of patients suffered from depression. Moreover, in 50% it had significant clinical significance [14–16].
It should be noted that in the study by T.A. Yanakaeva, 15 out of 30 (50%) patients had stage III dyscirculatory encephalopathy, while in the study by T.G. Voznesenskaya stage I or II was determined in all patients. Comparing the prevalence rates of depression in the cited studies, it can be assumed that emotional disorders are more common in the initial stages of chronic cerebrovascular insufficiency, and as the underlying disease progresses, their severity decreases somewhat.
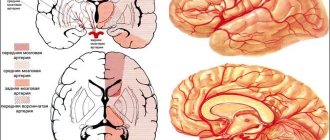
Depression and localization of vascular lesions of the brain
A connection is shown between the development of post-stroke depression and the location of vascular lesions in the brain. Thus, the greatest risk of developing emotional disorders is observed with damage to the left frontal lobe or subcortical gray ganglia of the left hemisphere [17–19]. It should be noted that the above-mentioned formations are in close functional connection with each other. According to one of the existing ideas, the circulation of excitation along closed frontostriatal neuronal circles is necessary for positive emotional reinforcement when achieving the desired result of an activity. The absence of such reinforcement may be a psychological mechanism for the development of depression in patients with vascular lesions of the brain of this location.
In addition to local brain damage, the development of vascular depression can be caused by diffuse changes in the white matter of the brain (leukoaraiosis). In the LADIS (LeucoAreosis and DISability) study, 639 patients aged 65 to 84 years were observed at 11 European neurological clinics for three years. The presence of more severe white matter changes at baseline was associated with a significantly higher risk of developing depression during follow-up [20, 21].
The connection between depression and leukoaraiosis makes it possible to classify depression in chronic vascular lesions of the brain as one of the manifestations of the phenomenon of dissociation. As is known, association fibers pass through the white matter of the brain, connecting various parts of the cerebral cortex, as well as cortical and subcortical structures. Thus, with diffuse brain damage, as with local damage, disruption of the functional interaction between the frontal cortex and the subcortical basal ganglia may be of decisive importance [22, 23].
A number of studies using volumetric neuroimaging have noted a statistical relationship between the volume of the anterior parts of the brain and subcortical basal ganglia and the risk of developing vascular depression [23, 24].
Clinical features of vascular depression
Depression of vascular etiology has a number of significant clinical features. According to GS Alexopoulos et al., who proposed the term “vascular depression,” these clinical features are the basis for diagnosing emotional disorders of vascular nature [25, 26].
Vascular depression develops in the second half of life (after 50 years), while ordinary depression often debuts at a young age. Thus, the first manifestation of emotional disorders in old age in the absence of episodes of depression in young years in a patient with cardiovascular diseases makes its vascular nature very likely [25–27].
According to the diagnostic criteria for depression according to ICD-10, to diagnose this mental disorder, the patient must have at least two (out of three) main clinical symptoms: depression or melancholy, anhedonia, decreased energy or fatigue (Table 1). Of the three indicated symptoms, depression of a vascular nature is not characterized by depression and melancholy [14, 15, 25, 26, 28]. In this regard, patients rarely complain of decreased mood and deny a depressed mood when questioned by their attending physician. Ideas of self-blame or feelings of guilt are also not characteristic of vascular depression.
On the contrary, the most characteristic symptom is anhedonia - the lack of a feeling of satisfaction from those activities that previously brought this feeling [14, 15, 25, 26, 28]. Patients lose interest in work, family, social life, their former interests and hobbies (“nothing makes me happy”). Due to loss of interest, patients become less active and devote most of their time to activities that do not require effort (for example, watching TV). Probably, the basis of anhedonia in vascular depression is a violation of positive emotional reinforcement associated with dysfunction of the “frontal cortex - subcortical basal ganglia” system, as discussed above.
No less characteristic is the feeling of decreased energy (anergy) [14, 15, 25, 26, 28]. For this reason, one of the most common complaints of patients with the initial stages of dyscirculatory encephalopathy is increased fatigue during mental and/or physical activity, as well as general weakness.
Features of vascular depression also include a high prevalence of so-called somatic symptoms (somatized depression) [29]:
- headaches of a compressive or vague nature, a feeling of heaviness, fog or other unpleasant sensations or discomfort in the head (the head is “somehow different”, “like cast iron”, “like being hit with a dust bag”), non-systemic dizziness (emptiness, discomfort in the head , feeling of slight intoxication or nausea), weather sensitivity;
- chronic pain of a different localization (pain in the spine, joints, muscles, internal organs), usually dull, poorly localized (“everything hurts”), aching in nature, not associated with movement or other external influences (“always hurts”);
- other unpleasant sensations that cannot be explained by the patient’s physical condition, especially if these sensations are poorly localized and are observed constantly or most of the time;
- sleep disorders: difficulty falling asleep or waking up at night or early in the morning - the patient wakes up before the right time and cannot fall asleep, despite the lack of satisfaction with sleep and the desire to sleep more, lies in bed for a long time without sleep.
From our point of view, it is the somatic symptoms of vascular depression that form the core of the so-called subjective neurological disorders [4], which are present at stage I of dyscirculatory encephalopathy [5]:
- headache;
- dizziness;
- noise in the ears or head;
- increased fatigue during mental work;
- sleep disorders;
- memory loss.
For making a diagnosis, a very important clinical feature of vascular depression is the significant severity of cognitive impairment [16, 23, 25, 26, 28, 30]. The cognitive status of patients is dominated by impairments of executive (frontal) functions in the form of insufficient planning and control. Most often, the pace of cognitive processes suffers: intellectual activity requires more time from patients than before (slowness of thinking, or bradyphrenia). At the same time, the ability to concentrate, concentrate and maintain an optimal level of attention for the required time is impaired. The greatest difficulties are caused by the need to quickly switch attention from one type of activity to another, so patients become intellectually inert, overly conservative, and wary of everything new [31–33].
Memory is impaired to a mild or moderate extent. Mainly operative memory suffers: patients cannot simultaneously retain significant amounts of information in their heads, which leads to difficulties in learning, carrying out professional or social activities. At the same time, memory for current and distant life events remains intact. The basis of memory disorders is the insufficiency of information reproduction with relative safety of memorization and storage. This can be judged by the effectiveness of the hints: the patient finds it difficult to remember this or that information on his own, but quickly remembers it if given a hint or given multiple choice. For example, a doctor, assessing memory, asks a patient: “What did you remember: this or that?” [31–33].
The significant severity of cognitive disorders in vascular depression raises a number of questions about the relationship between cognitive and emotional disorders in vascular pathology of the brain. When cognitive and emotional impairments are combined, cognitive disorders are often interpreted as a consequence of depression (pseudo-dementia or cognitive depressive syndrome). However, with vascular pathology of the brain, cognitive and emotional disorders can be independent consequences of vascular damage to the brain, united by a common substrate - dysfunction of the anterior parts of the brain and disruption of their connection with the subcortical basal ganglia. Depression can also be caused by cognitive disorders: as a result of insufficiency of frontal control functions, the patient may incorrectly assess the existing situation and behavior of both his own and those of loved ones. It is known that older people are touchy and vulnerable, and tend to make hasty, not always justified, conclusions. This is probably based on a lack of cognitive control, which is referred to in neuropsychology as frontal impulsivity. Incorrect cognitive assessment of the current situation can cause emotional suffering in elderly people with vascular pathology of the brain. When criticism is intact, depression may also be a patient's reaction to awareness of his cognitive failure.
Lack of cognitive control probably underlies emotional disorders characteristic of vascular pathology of the brain, such as affect lability and irritability, which often accompany vascular depression [31, 34]. Emotional lability implies a very rapid, insufficiently motivated change of mood: the patient sobs uncontrollably after seeing a sad scene in a movie, and immediately goes into a complacent state as soon as he is distracted from sad thoughts. At the same time, the patient cannot restrain external manifestations of emotionality, quickly becomes irritated, shouts at the people around him, etc.
Sometimes vascular depression is combined with symptoms of anxiety, which can also be somatized. Among the manifestations of anxiety, one should note a feeling of shortness of breath, stiffness, muscle tension, palpitations, pain in the heart area (cardialgia), numbness in the limbs, muscle twitching (for example, eyelid twitching), spasms (leg cramp), abdominal pain, alternating constipation and diarrhea, feeling hot, hot flashes, increased sweating and frequent urination [35].
Vascular depression is rarely severe and is usually not accompanied by suicidal thoughts or actions. The presence of such signs requires mandatory and urgent consultation with a psychiatrist.
As mentioned above, vascular depression is more characteristic of the initial rather than advanced stages of chronic cerebrovascular insufficiency. In the future, especially with the onset of vascular dementia, significant changes occur in the emotional state of patients. As criticism decreases, vascular depression regresses and is replaced by apathy. Apathy is usually understood as a decrease in motivation and initiative, a lack of interest in those types of activities that previously attracted people [36]. Moreover, unlike depression, the patient does not experience mental discomfort - his mood is normal or even elevated. Apathy is usually accompanied by the formation of emotional indifference to the environment: the patient is not touched by current events, the ability to empathize with others and emotional attachment to loved ones decreases.
Diagnosis of vascular depression
The vascular nature of emotional disorders can be assumed in the presence of a characteristic vascular lesion of the brain according to neuroimaging data (cerebral infarctions, leukoaraiosis) and the following clinical features [25, 26, 37]:
- onset after 50 years;
- the predominance in the clinical picture of anhedonia (lack of pleasure from life), decreased motivation and initiative, apathy, indifference;
- significantly pronounced cognitive symptoms: slowness of thinking (bradyphrenia), difficulty concentrating;
- absence of melancholy and guilt;
- tendency to protracted course;
- moderate pharmacoresistance.
Medical and social significance of vascular depression
Depression not only has a significant negative impact on the quality of life of the patient and his immediate environment, but also significantly complicates the treatment of the underlying vascular disease, increases the risk of stroke and mortality rates. It is known that depression is accompanied by activation of the hypothalamic-pituitary-adrenal system. An increase in the level of corticosteroid hormones as a result of such activation contributes to the progression of arterial hypertension and negatively affects the rheological properties of the blood. In addition, patients with depression are less adherent to any therapy, including therapy for underlying cardiovascular disease. Such patients are more likely to engage in behavior associated with increased vascular risk (smoking, drinking alcohol, overeating, etc.). In this regard, identification and correction of depression are of great importance for the overall prognosis [2, 14, 15].
Treatment of vascular depression
For vascular depression, as for depression of any other etiology, the prescription of antidepressants is indicated. According to a number of observations, the effectiveness of antidepressants in the vascular nature of emotional disorders is somewhat lower than in ordinary depression. Moreover, a greater severity of concomitant cognitive disorders is a predictor of an insufficient response to therapy [30]. Nevertheless, patients need to be helped, and there is no alternative to antidepressants at the current stage of development of neurology and psychiatry.
Clinical features of vascular depression, such as the elderly age of patients, the high prevalence and severity of cognitive impairment, require special care when choosing an antidepressant. It is known that non-selective antidepressants with an anticholinergic effect increase the severity of cognitive disorders. Such drugs are inappropriate in neurogeriatric practice in general and in the treatment of vascular depression in particular. At the same time, selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors, as well as melatonergic drugs do not have a negative effect on cognitive functions (Table 2).
Obviously, in the treatment of older people, priority is given to the safety and tolerability of prescribed medications. There is a certain relationship between the risk of adverse events and the selectivity of the effect on the serotonergic system. In this regard, SSRIs are less likely to cause side effects, such as exacerbation of concomitant anxiety, compared with non-selective drugs. However, even within the SSRI class, drugs have varying degrees of selectivity for the serotonergic system, and therefore have a different likelihood of side effects.
Escitalopram (Cipralex) has an almost exclusive effect on the serotonergic system. It is not surprising that this drug has established itself as an antidepressant, which extremely rarely causes any undesirable effects. Thus, according to the results of a meta-analysis of 117 randomized trials of SSRIs, in which a total of about 26 thousand patients with depression took part, Cipralex had the best safety and tolerability indicators in this pharmacological group. At the same time, in terms of the severity of the antidepressant effect, Cipralex is significantly superior to other SSRIs (fluoxetine, paroxetine and fluvoxamine) and is slightly inferior only to mirtazapine. It is important to note that the antidepressant effect of Cipralex develops when using minimal doses, which is of great importance in the treatment of elderly patients [38].
The effectiveness of Cipralex in the treatment of vascular depression has been shown in patients who have suffered a stroke. Thus, in the work of E.I. Guseva et al. Cipralex was taken by 99 patients with post-stroke depression. Inclusion criteria were a diagnosis of depression established within six months after an ischemic or hemorrhagic stroke, and the absence of dementia or significant disability due to other neurological disorders. Patients received the study drug at a standard dose (10 mg/day) for six months. During therapy, there was a significant regression in the severity of emotional disorders (according to the Beck scale) and sleep disturbances. In addition, the rate of patient adherence to concurrent therapy for the underlying vascular disease has improved, and the degree of social maladaptation in general has decreased [39].
Similar results were obtained in a study by M.A. Domashenko et al. Cipralex 10 mg/day was taken by 36 patients with post-stroke depression, which developed within three months after an ischemic stroke in the carotid system. The observation period was three months. During treatment, the severity of both depression and anxiety significantly decreased. These results are of great clinical significance due to the high comorbidity of depressive and anxiety disorders [12].
An important clinical feature of vascular depression, which has already been mentioned above, is the presence in its structure or in parallel as a comorbid condition of pronounced cognitive disorders. Anecdotal evidence suggests that SSRIs may have beneficial effects on cognitive function even in the absence of depression. RE Jorge et al. analyzed the effect of Cipralex on the cognitive functions of patients without depression during the recovery period of stroke. Over the course of one year, 129 patients received Cipralex, placebo, or psychotherapy. As a result, the use of Cipralex significantly improved cognitive functions, primarily memory, compared to placebo or psychotherapy [40]. It is likely that the positive cognitive effect of Cipralex is associated with the activation of the cerebral serotonergic system, which is involved in the regulation of not only emotions, but also cognitive processes. The positive cognitive effect of the drug may also be due to the normalization, against the background of its use, of the level of cerebral neurotrophic factor (brain-derived neurotrophic factor), which affects neurogenesis and reparative processes of the brain. The positive effect of Cipralex on the synthesis of this neurotrophic factor was also reported by A. Cattaneo et al. [41].
Conclusion
Vascular depression is a pressing clinical problem that requires a special approach to diagnosis and treatment. Timely detection of depressive disorders in patients with cerebrovascular accidents is of great importance for the selection of optimal therapeutic tactics and prognosis in general. At the same time, drugs that are highly selective to the cerebral serotonergic system are considered optimal for the correction of depression in such patients, since they have a beneficial effect on the cognitive sphere, and their use is accompanied by minimal side effects.
Diseases that cause death
Requests for help are becoming increasingly popular on TV screens, on the Internet and in newspapers. The following diseases are making headlines:
- Parkinson's disease is a disease in which neurons in the brain die and motor functions are impaired.
- Alzheimer's disease is a progressive disease associated with impaired neurodegenerative functions that leads to dementia.
- Epilepsy is a paroxysmal disease with the occurrence of seizures.
The above diseases are the main reasons for which nerve cells die in large quantities. In medicine, it is also found that damage to the brain and its functioning parts may be due to encephalitis. People can be immobilized for life, lose speech and many other important functions, which ultimately shortens their life and leads to death.
Literature
- Craig L Hyde, Michael W Nagle, Chao Tian, Xing Chen, Sara A Paciga, Jens R Wendland, et al.. (2016). Identification of 15 genetic loci associated with risk of major depression in individuals of European descent. Nat Genet
.
48 , 1031-1036; - Novel study method identifies 15 genomic regions associated with depression. (2016). Science Daily;
- Code of Life: Reading does not mean understanding;
- Genetics of psoriasis: immunity, skin barrier function and GWAS;
- GWAS and psychogenetics: consortia in search of associations;
- The mysterious genetics of the “mysterious skin disease” - vitiligo;
- Wei Cheng, Edmund T. Rolls, Jiang Qiu, Wei Liu, Yanqing Tang, Chu-Chung Huang, et al.. (2016). Medial reward and lateral non-reward orbitofrontal cortex circuits change in opposite directions in depression. Brain
.
139 , 3296-3309; - Depression's physical source discovered. (2016). Science Daily...
How to save neurons
Nerve cells are restored - myth or reality? During the process of embryogenesis, all cells, tissues and organs are laid down and formed inside the body, in exactly this order. A huge number of brain cells are formed even before the birth of a child - he loses some at birth, another part during the first years of life, and so on throughout his entire life. Restoring nerve cells is a myth that can be turned into reality with little effort. These efforts consist not only in training memory and attention through various exercises, reading books, watching films, intellectual games, but also proper nutrition - it is the key to the health of the whole body.
The following factors can preserve, prolong life and restore neurons:
- Sufficient amount of oxygen . It's no secret that the brain feeds on oxygen, which means that for its proper and normal functioning there must be a lot of this element. Pure water, foods that stimulate the production of hemoglobin and the brain will be fed in the right amount.
- Vascular balance . Cholesterol plaques that attach to blood vessels disrupt the flow of blood, and therefore oxygen, and therefore the nutrition of the brain
- Vitamin and mineral complexes . In addition to the vitamins and minerals that enter the body with food, it is necessary to consume potassium, calcium, magnesium, phosphorus and iodine in courses.
- Emotional comfort . Of course, a favorable psycho-emotional background for a person is an important aspect in this process.
Symptoms
Atrophic brain damage first manifests itself in barely noticeable changes: a person indulges in apathy and indifference, his aspirations disappear and lethargy appears, and his memory deteriorates. Previous skills are lost and new ones are difficult to acquire. Often there is a strong deviation from moral norms, irritability and conflict levels increase, sudden mood swings and depression occur.
The following symptoms are also observed:
- impoverishment of the vocabulary - a protracted selection of the necessary words to express ordinary realities;
- decreased brain activity;
- the disappearance of self-criticism and the ability to comprehend;
- sensitivity disorders, erectile dysfunction;
- deterioration of motor skills;
- parkinsonism.
Specific symptoms of cerebral atrophy of the head depend on the involvement of different areas. For example, dysfunction of the frontal lobes negatively affects behavior and intelligence, and damage to the cerebellum affects motor skills, gait, speech and handwriting. If the nerve pathways are damaged, autonomic disorders may occur.
What to do to stop dying
If cell death has already begun, then it should be slowed down and stopped. This can be done with the help of drug therapy. Groups of drugs used in medicine:
- Antioxidants.
- Neuropeptides.
- Neurometaloliths.
- Vitamins and minerals.
There are radicals inside every brain cell. When there are too many of them, they simply kill this cell. Antidepressants cope well with this process. Unfortunately, people quickly get used to them and have significant side effects.
Neuropeptides, in turn, slow down the death process and manage healthy cells, as well as build new ones.
Many feel the effect after starting to take these groups of drugs, because this is a kind of prevention from unwanted complications when the disease has progressed far and it is unlikely that anything can be done to save the situation.
Diagnosis and treatment
The disease is diagnosed comprehensively: an objective examination, a conversation with a doctor, instrumental examination and psychodiagnostics.
- An objective examination involves studying elementary nervous activity: the activity of tendon reflexes, coordination of the eyes and limb movements, performing simple actions (tying shoelaces).
- During the conversation, the doctor finds out the patient’s vocabulary and his criticism of his disease. The general condition is assessed: the presence of consciousness, satisfaction with health in general.
- The task of instrumental methods is to visualize atrophic disorders in the brain using MRI, CT or vasography. In the resulting drawings, organic changes in the telencephalon are studied.
- Using psychodiagnostics, a medical psychologist studies the degree of loss of intellectual functions. The doctor determines the patient’s ability to remember, consistency of thinking, attention span, IQ and emotional state.
Treatment of GM atrophy is symptomatic. To correct emotional disorders, mood stabilizers are prescribed - drugs that stabilize mood. Lost intellectual functions are not restored, so the patient requires constant care: hygiene, feeding, ensuring comfort and coziness.
Drug treatment acts only as an auxiliary method. The best thing that loved ones can give is caring for the sick. The patient should be provided with maximum comfort of life, ease of household chores, support, stimulation and praise. To prevent the progression of pathology, you should engage in light physical activity, walk in the fresh air, read, and, if possible, solve simple problems and puzzles such as Sudoku or crosswords.
Forecasts
Clinical death does not always mean that the patient will definitely die. Sometimes doctors manage to bring a person out of a state of clinical death. The prognosis will be influenced by what circumstance led to such a condition and what resuscitation measures were taken. The main condition is to restore blood circulation in the first 3-5 minutes. Sometimes resuscitation is carried out for up to 20-40 minutes.
Even if partial extinction and death of neurons has occurred, the functions of the medulla can be restored. If biological death or brain death is established, it is impossible to bring the patient back to life, you need to come to terms with this.
The peculiarity of the human brain is that it strives to preserve its functions by any means. If some neurons die, their tasks can be redistributed to other zones. Patients who have suffered a stroke, ischemia, and even serious TBI often return to a full life.
Cytokine storm
Encephalopathy (dystrophic damage to brain tissue) can develop due to the fact that the cells of the immune system of a person infected with coronavirus begin to actively release cytokines into the blood. This class of substances includes about a hundred complex proteins involved in many immune and inflammatory processes in the human body, Nikolai Karpov, an employee of the Institute of Biology of Tyumen State University, told Izvestia. The increase in the concentration of such proteins is called a “cytokine storm.”
“In excess, these substances can damage the walls of blood vessels and cause hemorrhages in the brain, which leads to the development of certain neurological symptoms (depending on the affected area),” the expert said. “It is also possible that the virus can penetrate the blood-brain barrier directly into the brain tissue.
Electron microscopic image of coronavirus reproduction
Photo: REUTERS/US NIAID-RML
According to the scientist, not only coronavirus, but also influenza, as well as other acute respiratory viral infections, can cause encephalopathy, but this complication is rare. In general, science knows dozens of viral diseases, which in a certain percentage of cases cause neurological complications. For example, the viruses of tick-borne encephalitis, measles, herpes types 1 and 2 and West Nile fever, almost all alphaviruses, including the Karelian fever virus (an acute infection believed to be carried by mosquitoes of the genus Culex. - Izvestia) and a lot others.
Corona pressure: hypertension has become the most common companion of COVID-19
At the same time, stress and panic can worsen the course of cardiovascular diseases, Russian scientists believe
Symptoms
The following symptoms indicate brain death:
- there is no consciousness, and this process is persistent;
- there are no reactions to tingling, stroking, handling, no tactile sensitivity;
- no movement of the eyeballs;
- the heart has stopped, as evidenced by a straight line on the ECG;
- there is urinary and fecal incontinence;
- breathing is impaired, the chest does not rise.
Determining whether a patient has died is an extremely important task. Doctors do not immediately diagnose death. Even if all of the listed signs are detected, the person is monitored in the hospital for up to 12 hours. Sometimes, although rarely, signs of brain activity may appear. If during this time the patient does not react in any way, there are no trunk reflexes, then biological death can be stated.
It is important how the brain dies, what triggered the death of neurons. If poisoning has led to such serious consequences, the patient should be monitored for at least a day. If the cause is TBI, the observation time is reduced to 6 hours. The specific decision must be made by the neurosurgeon. It is important that the doctor monitors the patient from the onset of this condition, then he will have a complete picture of events that will allow him to make the right decision.
The onset of biological death is determined exclusively by a neurologist. It is based on subjective and objective criteria. If signs of brain death are clearly identified, the person must be disconnected from life support. This difficult decision is especially difficult to make if the disaster happened suddenly. Often relatives are literally horrified by such a message. If a person is sick for a long time, his loved ones eventually become at least a little accustomed to the idea that their loved one will be gone. In any case, this decision is very difficult.