Epilepsy is a neurological chronic disease of the brain. It is considered one of the most severe and most common neurological diseases.
Epilepsy is usually detected at an early age. Spontaneous, short-term, convulsive seizures that occur with an unknown frequency, and loss of consciousness can accompany the patient throughout his life.
Doctors classify the disease into primary and secondary epilepsy. The primary form of the disease is congenital, so attacks can appear already in childhood and adolescence.
The secondary (symptomatic) type of epileptic seizures develops after damage to the structure of the brain (as a result of trauma) or after a disruption of the metabolic process in it (failure in metabolic processes can be triggered by a number of diseases: tumor, stroke, infectious diseases, drug and alcohol addiction).
The disease is not new; for the first time its description was found in Ancient Egypt even BC. Falling disease is what epilepsy is called in Russia. Epileptic seizures occur in every hundredth person in the world.
If doctors cannot select medications for the treatment of epileptic seizures that would adequately control the patient’s recurring seizures, there is only one way out - surgical treatment.
Operation efficiency
In 2000, it was found that surgical treatment of certain forms of epilepsy (temporal lobe epilepsy, for example) is equivalent to an additional year of conservative treatment for this disease. In addition, drug treatment turned out to be 8 times less effective compared to surgical treatment. 64% of patients who lay on the operating table were able to completely get rid of attacks.
If a person meets all the indications for surgical treatment, then it should be started as soon as possible. A possible consequence of the operation may also be that the person is unadapted to life without seizures. Therefore, surgical intervention must be carried out together with medical and social rehabilitation.
It is also worth remembering that the patient always takes a small, but still risk. Even if he is an ideal candidate for surgery, personality changes or cognitive impairment may occur. However, this is not an argument in favor of not needing treatment. The doctor must choose a specific method of therapy on an individual basis.
Also, you should not completely abandon conservative treatment. Even if the surgery gives a good result, you must take antiepileptic drugs for 2 years. This is necessary for the brain to adapt. Although in some cases this rule can be neglected by the doctor’s decision.
In which cases is it impossible to do without surgical intervention?
Surgical interventions for epilepsy first began to be performed more than forty years ago, in the early 80s of the last century. The first operations brought conflicting results - on the one hand, doctors achieved positive results in treating the disease, on the other hand, the lesions forced them to look for ways to improve existing techniques.
Epilepsy, previously considered incurable, is increasingly subject to surgical treatment, which can significantly alleviate the course of the disease, and in some cases lead to a cure.
The choice of surgical method is carried out after identifying the exact localization of the focus of activity.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
Compared to the last century, today's interventions are more successful. In recent years, the number of patients in Russia who want to use surgical treatment as a way to combat the disease has increased.
Surgical treatment is not indicated for seizures that do not affect the quality of life, for generalized idiopathic epilepsy or benign epileptic syndromes, for severe concomitant pathology and severe mental disorders.
In the case of symptomatic drug-resistant forms of epilepsy, surgical treatment eliminates seizures in 26-72% of patients.If there are indications for surgical treatment, then the sooner the operation is performed from the onset of epilepsy, the higher the effectiveness.
Neurologist
Pershina Natalia Sergeevna
8 years of experience
As practice shows, it is possible to cure pathology surgically without threatening the health of patients in twenty percent of patients. This means that every fifth person after surgery can become a completely healthy person, forgetting about epileptic seizures.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
Doctors are considering surgery if the lesion is localized in a limited area of the brain that is not responsible for vital functions. Surgeons do not intervene in those places that control hearing, speech, and language. The purpose of the operation is to reduce the frequency of epileptic seizures and return the patient to normal life.
Epilepsy in sleep
Epilepsy is a brain pathology in which seizures recur periodically and begin suddenly.
The following conditions are immediate indications:
- medial temporal sclerosis;
- simple attacks with preservation of consciousness at the very beginning of the attack;
- complex seizures accompanied by loss of consciousness;
- atonic seizures (drop attacks) with sudden falls without the onset of seizures.
Doctors also consider other important factors that influence the possibility or impossibility of surgery. These include:
- frequency of epileptic seizures;
- severity of seizures (time course, consequences, etc.);
- compliance with antiepileptic therapy and certification of its ineffectiveness;
- degree of addiction to certain drugs (usually after 3-5 years the drugs may have a much weaker effect than at the very beginning of taking them);
- neurological status, exact localization of the pathological zone in the brain;
- degree of cognitive impairment;
- possibility of surgery, absence of contraindications;
- prediction of postoperative disorders.
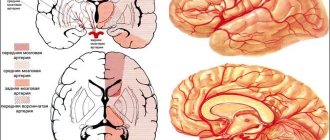
Usually, when performing surgery, doctors are faced with the need to remove a tumor in the brain that has caused epileptic seizures. The second most common cause of pathology is sclerosis of the hippocampus of the temporal lobe.
Operations are performed not only when it is possible to cure a patient of epilepsy. In some cases, intervention is required to prevent the pathology from affecting other parts of the brain.
The outcome of the operation is favorable - in some patients, seizures disappear forever, while in others they cease to be so frequent and can be suppressed with antiepileptic drugs. Complications occur rarely and only when functionally significant areas of the brain are removed.
Indications for surgery
Surgical treatment of epilepsy is prescribed only after appropriate diagnosis. It begins with the Wada test, the purpose of which is to determine the areas that are responsible for speech and memory. To do this, amobarbital is injected into the carotid artery (that is, the carotid artery). As a rule, before surgery, electrodes are implanted directly into the brain, which make it possible to track any changes in a person’s condition and understand from which area of the brain the attacks begin. Such diagnostics show significantly better results than classic EEG.
Experts have identified three types of epilepsy for which neurosurgical intervention is indicated:
- Focal seizures. These are seizures that do not extend beyond one area of the brain. Manifestations may vary, ranging from inexplicable emotions to loss of consciousness with preservation of motor automatisms.
- Seizures that start out as focal seizures but then spread to other areas of the brain.
- Unilateral multifocal epilepsy with infantile hemiplegia. These are epileptic seizures in infants that affect multiple areas of the brain.
However, even in these cases, surgical treatment of epilepsy is not prescribed immediately, but only if two or three medications have not helped or if the area of the brain affected by the disease can be clearly identified.
Also, surgery is needed to eliminate the root cause that causes secondary epilepsy - a pathological neoplasm in the brain, hydrocephalus and other diseases.
Preparing for surgery for epilepsy
Any neurosurgical intervention involves a full comprehensive examination, pursuing two goals. The first is to identify the exact location of the epileptic zone. The second is to make sure that the patient’s body can withstand such a load (long stay under general anesthesia, rehabilitation after surgery).
To diagnose the brain and identify the source of excitation, the following studies are used:
- EEG (electroencephalography – records brain activity);
- MRI (magnetic resonance imaging - reveals the localization of affected areas of the brain and their parameters: size, structure, shape);
- electroneurography – assesses the state of the peripheral nervous system;
- electromyography – studies bioelectric potentials, i.e. brain reaction to stimuli;
- Doppler sonography – examines the blood vessels of the brain and the processes occurring in them;
- PET (positron emission tomography - detects oncological pathologies in the brain).
Neuropsychological testing is also carried out with the patient, which allows us to determine the characteristics of thinking, worldview and nervous reactions of a person with epilepsy. After the operation, a repeat diagnosis is made to determine the changes that have occurred to the patient.
Eliminating the focus of a seizure
This operation (called a lobectomy) is the most common. The surgeon simply removes the area of the epileptic's brain in which the disease is localized (focal area). Obviously, such an intervention will only help with the focal form. The effectiveness of this “therapeutic measure” depends on how clearly defined the area in which the attacks occur is. If good, then the probability of cure is 55-70%.
The most common area to be removed is the temporal lobe. This is the most effective type of lobectomy, which leads to positive dynamics in 70-90% of cases.
Types of surgical treatment for epilepsy
Various types of surgery are used to treat epilepsy. The different types of surgery used depend on how the disease manifests itself and what part of the brain is affected.
Temporal lobe resection
The largest part of the brain is divided into 4 paired sections called lobes (frontal, parietal, occipital and temporal). Temporal epilepsy, which is localized in the temporal lobe, is the most common type of pathology in adolescents and adults.
During temporal lobe resection, the brain tissue in this area is cut away. Extratemporal resection involves removing brain tissue from areas outside the temporal lobe.
Lesionectomy
This surgery repairs a brain lesion—a defective area, such as a brain tumor or damaged blood vessel, that causes seizures. In most cases, attacks stop after removal of the damaged area.
Callosotomy of the corpus callosum
The corpus callosum is a plexus of nerve fibers that connects the hemispheres of the brain. During this operation, the doctor cuts the corpus callosum, which breaks the connection between the hemispheres and prevents seizures from spreading from one side of the brain to the other. It is best suited for people with extreme forms of uncontrolled epilepsy, with intense seizures that can lead to falls and severe injury.
Functional hemispherectomy
A hemispherectomy involves removing the entire hemisphere of the brain. If a functional hemispherectomy is performed, the hemisphere remains in place but is disconnected from the rest of the brain. In this case, only a limited area of tissue is removed.
Vagus nerve stimulation
This method is used if resection is impossible. The device, placed under the skin in the neck, sends an electronic impulse to the vagus nerve, which controls the activity of the brain and major internal organs. It reduces seizure activity in some people with focal (partial) seizures.
Multiple subpial incisions
This procedure helps control seizures that occur in areas of the brain that cannot be safely removed. The surgeon makes a series of small incisions in the brain tissue. These incisions stop or reduce seizures but do not interfere with normal brain activity, which preserves the patient's full function.
Implantation of the RNS neurostimulator
Doctors place a small neurostimulator in the skull, just under the skin. They connect it to 1 or 2 wires (called electrodes) that they place either in the part of the brain where the seizure begins or on the surface of the brain. The device detects abnormal electrical activity in the area and sends an electrical current. This can stop the process that leads to seizures.
Multiple subpial transsection
This type of treatment is used in cases where the damaged area of the brain cannot be safely removed. In this case, the focus is not removed, but notches are made on the surface of the brain. This helps prevent the attack from spreading to other areas. Multiple subpial transsection is often used simultaneously with resection of other areas that are safer in terms of the consequences of surgical intervention.
One example of this operation in a child is the treatment of Landau-Kleffner syndrome, which affects the areas responsible for speech and perception.
The operation is performed under general anesthesia. The surgeon opens the skull and gains access to the dura mater of the brain. Next, several parallel incisions are applied to the gray matter. The operation is carried out on the part of the brain that is identified as the focus of seizures. After this procedure, the dura mater and part of the skull are put back in place. The effectiveness of the operation is 70% in adults, but how reliable these data are is unknown, since this method of treatment was invented recently.
Possible complications after surgery:
- Brain swelling.
- Nausea, headaches, emotional disturbances (depression).
- Speech and memory dysfunctions.
After the operation, you need to remain under the supervision of doctors for another day or two. Recovery takes about a month and a half, during which you need to take antiepileptic drugs. When the attacks stop, you can reduce the dosage of medications or stop them altogether.
Treatment of epilepsy in children
These features of the developing brain determine the clinical specificity of epilepsy in childhood. In particular, the manifestation and course of all idiopathic (i.e., caused by the intrinsic properties of the brain) epilepsies, which in children account for about half of all cases of the disease, occur in childhood. Symptomatic forms of epilepsy, associated in most cases with perinatal and intrauterine harm [1,4,11], due to the listed features of hyperexcitability, often take a pharmacoresistant course and lead to developmental disorders. At the same time, since the course of epilepsy during this period is determined to a significant extent by developmental factors, the long-term prognosis for seizures in children is much better than in adults [7,11]. Features of the treatment of epilepsy in children are also determined by the fact that, due to the high metabolic rate, drug doses per body weight are usually higher than in adults. General principles of treatment of epilepsy The goal of treatment of epilepsy is the complete cessation of seizures without neuropsychic and somatic side effects and ensuring the pedagogical, professional and social adaptation of the patient. With the correct patient management tactics and pharmacotherapy, a cure for epilepsy is achieved in more than half of the cases. Not all cases of epileptic seizures require medication. You can refrain from drug treatment in the following cases: a) the first isolated epileptic seizure; b) rare or mild epileptic seizures in relatively benign idiopathic forms of epilepsy that do not maladapt the patient; c) rare (no more than 1 per year) seizures, if the EEG does not reveal epileptiform and focal pathological activity, since it is not known whether there will be another one. The patient and relatives should be instructed to avoid high-risk situations and provoking factors. Specific long-term drug antiepileptic treatment should be started only in case of a definite epileptic disorder with recurrent seizures and/or mental, communicative, cognitive impairments that maladapt the patient. Regular sleep is indicated (premature awakenings are contraindicated), mental comfort, and an active lifestyle to the best of your ability. Hyperinsolation and hyperthermia, excessive intake of tea and coffee, and alcohol should be avoided. The following drugs are contraindicated: antihistamines, some antidepressants, neuroleptics, dopamine agonists, local anesthetics, cerebrolysin, prostaglandin, sympathomimetic stimulants (phenitylline, pemoline, methylphenidate), chloroquine, indomethacin, interferon, isoniazid, vasopressin, virostatics and cytostatics, penicillin in large doses, theophylline and its derivatives, quinolone and piperazine. J Vaccination against diphtheria is carried out with a vaccine with a reduced content of the antigenic component “d”. J Vaccination against chickenpox, hepatitis A, pneumococcus, meningococcus is permissible only in cases of extreme necessity. J Vaccination with whole pertussis virus, parenteral vaccination against typhoid, paratyphoid and cholera are contraindicated. Laboratory tests to determine drug tolerability should be repeated 1 and 3 months from the start of treatment and then at intervals of 4–6 months. Treatment of epilepsy is based on the diagnosis of the form of epilepsy according to the Classification of Epilepsies and Epileptic Syndromes [1,8], since the choice of antiepileptic drug depends on this. The main factors for assigning a particular form are etiology and cerebral localization. From the point of view of etiology, all epilepsies and syndromes are divided into idiopathic, symptomatic and presumably symptomatic (cryptogenic). Idiopathic - epilepsy associated with polygenic or multifactorial inheritance, not caused by structural damage to the brain or other known disease. Symptomatic – epilepsy or syndromes caused by detectable cerebral-organic damage, a known metabolic disorder, or a developing pathological process. Symptomatic epilepsy is characterized by: 1) macrostructural or cytoarchitectonic brain damage with localization corresponding to the type of seizures; 2) cerebral non-attack symptoms corresponding to the clinical picture of seizures. The prognosis depends on the etiology of the disease - resistance and impaired neuropsychological development are often noted. Cryptogenic – presumably symptomatic epilepsies and syndromes, the cause of which is not clear. From the point of view of localization, all epilepsies and syndromes are divided into: 1) associated with localization (focal, partial); 2) generalized and 3) uncertain as to whether they are focal or generalized. Pharmacotherapy depending on the form of epilepsy From a practical point of view, it is advisable to use a modification of the Classification of Epilepsies and Epileptic Syndromes proposed by the Commission on Terminology and Classification of the International League Against Epilepsy (IEL) [8] (Table 1). The main subgroups of forms of epilepsy and epileptic syndromes are formed according to features of significant similarity within the subgroup. In Table 1, the new headings are: focal familial autosomal dominant, separated from the group of idiopathic focal ones based on evidence of the type of inheritance, and epileptic encephalopathies, separated from the three main sections of the 1989 classification based on the presence of severe permanent non-attack psycho-neurological disorders caused by epileptic activity brain Their characteristics and treatment approaches are outlined below. Progressive myoclonus-epilepsy accounts for no more than 1-2% of all cases of epileptic seizures, since they are a manifestation of numerous autosomal recessive diseases, in most cases they have an unfavorable prognosis. Consideration of the management of such patients goes beyond the treatment of epilepsy as an independent disease. Regarding “seizures not necessarily requiring a diagnosis of epilepsy,” grouped under the last heading, general tactics are given at the beginning of the previous section. Pharmacological treatment should begin with monotherapy with one of the traditional first-choice drugs (valproic acid - VPA or carbamazepine - CBZ) with the dose adjusted to an effective one. If no improvement is achieved at the maximum permissible dose for a period corresponding to the equalized plasma concentration of the drug, another drug corresponding to the form of epilepsy is added, and if successful, an attempt is made to switch to monotherapy with this drug. If complete withdrawal of the first drug is unsuccessful, the patient is left on duotherapy. If traditional drugs are unsuccessful, they gradually switch to a new drug (lamotrigine - LTG, levetiracetam - LVTC, topiramate - TPM, oxcarbazepine - OKBZ, gabapentin - GBP) according to the same rules. It is recommended to use no more than two anticonvulsants at a time, with the exception of adding a third anticonvulsant drug (usually a benzodiazepine) for a short time. Due to a significant number of complications, first-generation drugs (barbiturates and phenytoin - FT) are used when those listed above are ineffective. Benzodiazepines (clonazepam - KZP, nitrazepam - NZP, clobazam - KLBZ) are recommended to be used only if other drugs are ineffective for up to 3-6 weeks in order to avoid the development of tolerance and addiction only in case of uncontrolled worsening and increased frequency of seizures or severe epileptic encephalopathies. The choice of pharmacological treatment depends on the achievable accuracy of the diagnosis: a) diagnosis of epilepsy, but it was not possible to clarify the form; b) a form of epilepsy has been established, belonging to one of the main subgroups of classification and terminology: 1) focal idiopathic, 2) focal symptomatic (or cryptogenic), 3) generalized idiopathic, 4) epileptic encephalopathy. Pharmacotherapy of epilepsy in an unspecified form If you are uncertain about the form of epilepsy, you should start with a drug with the widest spectrum of action - VPA. If VPA is unsuccessful, the form of epilepsy is specified and a drug more specific to this form is selected. With success and drug remission at the age of 2–5 years, the question of gradual withdrawal of pharmacotherapy may be raised (Fig. 1). Pharmacotherapy of focal idiopathic epilepsies Due to the usually favorable course and prognosis, in cases where seizures do not maladapt the patient and there are no mental and behavioral disorders, you can refrain from pharmacotherapy. Otherwise, for most focal idiopathic epilepsies, valproic acid is the drug of choice. Therapy is usually discontinued if there are no seizures for 1–2 years with a normal EEG. If valproic acid in sufficient doses is not effective, LVTC, LTG, TPM or other drugs should be tried (Fig. 2). For idiopathic focal epilepsies, the following drugs are used: VPA, LTG, TPM, LVTC, CBZ, OKBZ, FT, phenobarbital (PB). Table 2 shows the features of treatment of individual forms of idiopathic focal epilepsy. Pharmacotherapy of focal symptomatic (cryptogenic) epilepsies The first choice drugs are CBZ and VPA. CBZ is selected if there are no bilaterally synchronous epileptiform discharges in the EEG. It is also preferable for frontal lobe epilepsy, in the absence of bilaterally synchronous epileptiform discharges in the EEG. In other cases, and also when there is no certainty about the focal nature of seizures or the symptomatic origin of epilepsy, VPA is preferable. If the first drug is insufficiently effective, an alternative traditional drug is tried. If unsuccessful, new drugs are used (Fig. 3). Table 3 provides empirical data on the preferred choice of drugs depending on the type of seizures and form of epilepsy. The drugs are given in order of choice. Pharmacotherapy of idiopathic generalized epilepsies The first choice drug for all idiopathic generalized epilepsies is VPA. If VPA at a sufficient therapeutic dose is not effective, further choices are made depending on the form of the seizures. If the main drugs in mono- and polytherapy are not effective, benzodiazepines are used for serial seizures before selecting basic therapy: KZP, KLBZ, MDZL. Treatment of idiopathic epilepsy with generalized tonic-clonic seizures The drug of choice is VPA. In case of failure in the absence of bilaterally synchronous epileptiform discharges in the EEG, CBZ is selected. If CBZ is unsuccessful, new drugs are tried: LVTC, LTG, TPM, GBPT, OKBZ in that order. The same drugs, in the presence of bilaterally synchronous epileptiform discharges in the EEG, bypassing CBZ, are used in case of ineffective VPA. If the additional drug is successful, an attempt is made to switch to monotherapy with this drug. If seizures become more severe when the dose of the first drug is reduced, the patient remains on duotherapy. If the above drugs are ineffective, FB, PRM and other combinations are tried (Fig. 4). Treatment of idiopathic epilepsy with absence seizures In the treatment of childhood absence epilepsy (occurring without generalized tonic-clonic seizures), the first choice drugs are VPA, the second choice is ethosuximide (ESM), LTG, LVTC, TPM. KBZ, OKBZ, FT, FB are not shown. Treatment of juvenile epilepsy with absence seizures is carried out with the same drugs with the peculiarity that ESM should not be used in monotherapy due to its inability to control generalized tonic-clonic seizures (Fig. 5). Treatment of childhood and adolescent idiopathic generalized epilepsy with myoclonic seizures (juvenile myoclonic epilepsy, epilepsy with myoclonic-astatic seizures, epilepsy with myoclonic absence seizures) The drug of first choice is VPA. If VPA is unsuccessful, LVTC is used. Drugs of further choice: TPM, ESM, KZP, FB, PRM. In the absence of absence seizures, it is not advisable to try ESM. KBZ, FT are not shown. LTG may aggravate myoclonic seizures (Fig. 6). Forms and treatment of epileptic encephalopathies Epileptic encephalopathies are a group of epilepsies and epileptic syndromes in which epileptic discharges detected by EEG lead to progressive brain dysfunction with neurological, mental or behavioral symptoms [3, 8]. Their main forms are shown in Table 4. The first group refers to usually incurable symptomatic epileptic disorders of infancy and childhood with a poor prognosis in terms of seizure control, severe impairment of psychomotor development and life expectancy. They are based on severe structural disorders of the brain or genetic defects. The second subgroup differs in that the main problem of patients is cognitive, mental and behavioral disorders, usually with rare or even absent seizures. Treatment of “catastrophic” epileptic encephalopathies. Treatment of epilepsy with infantile spasms (West syndrome) Drugs: adrenocorticotropic hormone (ACTH) (40–180 IU per day), VPA (40–100 mg/kg per day), B6 – pyridoxine (20–30 mg/kg per day) , benzodiazepines, vigabatrin (VHBT) (40–100 mg/kg per day), LVTC (40–100 mg/kg per day), TPM, LTG. The beginning of treatment is vitamin B6 (pyridoxine) 20–30 mg/kg per day orally (in Russia, the corresponding dosages are provided by the drug Neuromultivit) under EEG monitoring. The effect is visible during the first two weeks of treatment in the form of cessation of hypsarrhythmia in the EEG and spasms. If pyridoxine is ineffective - VPA + ACTH. In Russia, a synthetic analogue of ACTH is used - tetracosactide (1 mg/1 ml - ampoules) intramuscularly 0.1 ml after 2 days on the third - 3 injections, then 0.2 ml after 2 days on the third - 3 injections, then injections are repeated after 2 days on the third, increasing the single dose by 0.1 ml every week until the dose at which the attacks stop. At this dose, treatment lasts up to 2 weeks. Then the dose is gradually reduced over 3 months. Other doses and regimens are possible. If ineffective, NWP is used at a dose of 0.4–3 mg/kg/day three times a day. The effectiveness of VHBT, LTG, TPM has been shown (Fig. 7) [1,10,12]. Treatment of Lennox–Gastaut syndrome Drugs: VPA (20–50 mg/kg per day), ESM, benzodiazepines, ACTH (40–180 IU per day), B6 (20–30 mg/kg per day), LVTC (30–100 mg/kg per day), TPM, LTG (Fig. 8). CBZ, OKBZ, GBP, FB, LTG can aggravate myoclonic seizures; FB aggravates cognitive and behavioral symptoms. Forms and treatment of encephalopathies with predominant cognitive, mental and behavioral symptoms (often without seizures) Name: Epileptic encephalopathy or epileptic brain dysfunction with behavioral, mental or neuropsychological disorders. Definition: Epileptic encephalopathy or epileptic dysfunction with behavioral, mental, neuropsychological symptoms is a disorder, the main or only manifestation of which is persistent disorders of the specified type, caused by epileptic discharges in the brain, objectively recorded by electroencephalography in the form of epileptiform activity. They constitute up to 5–50% (depending on the form) of disorders usually classified as behavioral and mental disorders according to ICD-10, and about 5% of all epileptic syndromes in childhood. In the absence of proper antiepileptic treatment, they tend to progress. Age of manifestation: usually 3–15 years, sometimes later. Seizures: Absent or rare or in distant history. Usually focal with impaired consciousness, secondary generalized, typical and atypical absences, frontal “pseudo-absences”. EEG: Mandatory presence of gross epileptiform activity. The nature and location of the disorders correspond to the form of psycho-cognitive-communicative disorders. Neurology: Depends on etiology. Often without significant deviations in the sensory-motor sphere. Neuropsychological symptoms associated with the main mental disorder: aphasia, speech dyspraxia, mutism, agnosia, spatial disorientation, disturbances of wakefulness, attention, memory, thinking processes, frontal symptoms. Sometimes disturbances of motor functions, general praxis, ataxic, dystonic. Psyche: Depending on the form - behavioral, hyperkinetic disorders, autism, mental retardation, speech development, obsessive-compulsive symptoms, aggression and auto-aggression, depressive, anxiety disorders, dysfunction of executive functions, socialization functions; pedagogical, labor and social maladjustment. Neuroradiology: Usually without significant structural changes. Etiology: pre- and perinatal disorders, in some cases - idiopathic or autosomal -dominant, in most cases - cryptogenic. Forecast: depends on the etiology. In the absence of significant macrostructural brain disorders and its congenital pathology with proper treatment, is favorable. With insufficiently persistent treatment aimed at suppressing epileptic activity in the EEG - the progress of psycho -cognitive disorders with the probability of severe social disorders. It is possible to join seizures. Therapy: Means of the first choice: Slot. Funds of the second choice: LVTC, LTG, ESM, Sultiam, ACTH, Vitamin B6 in large doses (Fig. 8). Not shown - FT, FB, KBZ, neuroleptics of the phenotiazines group, tricyclic antidepressants, nootropics. Pharmacotherapy is primarily aimed at suppressing epileptiform activity in the EEG, since the improvement of mental functions (especially cognitive and speech) lags behind neurophysiological dynamics. In pharmacoresistant cases, neurosurgical surgery of subpical transl in the bark in an epileptic focus is indicated. Treatment of syndromes and epilepsy with a specific way of causing. These include epileptic syndromes with seizures, exclusively or almost exclusively caused by some external influence or mental activity - mainly the so -called reflex epilepsy: 1) photogenic epilepsy (flickering of light or pattern, including epilepsy of reading); 2) gaptogenic epilepsy (seizures caused by somatonstoric influences); 3) audiogenic epilepsy; 4) start -epilepsy (seizures caused by fright); 5) seizures caused by certain experiences, thoughts and mental operations. The most common reflex epilepsy is photogenic. Therapy: avoiding specific situations and influences that provoke a seizure. Anticonvulsants are usually not shown. Sleep, LVTC, etc. - only in cases of self -stimulation of the patient to cause pleasant sensations associated with the seizure. With photogenic epilepsy, where seizures are provoked by flickering light or visual pattern (in particular, the flickering of frames on the TV screen), the following prevention is used: 1) watch TV from a distance of at least 2 m from the screen located at a level of no higher than the eyes; 2) with a reduced level of contrast and brightness; 3) high quality of the image, it is better with a frame rate of 100 Hz; 4) in the lighting room; 5) if necessary, look through glasses with one closed glass (one eye) or through glasses with polarizing lenses; 6) do not watch TV after sleep deprivation; 7) Avoid looking at a stable flickering rhythmic pattern. With the failure of non -drug methods - sail, LVTC, benzodiazepines, destroyers. The treatment of febrile seizures of febriles is the epileptic seizures that occur in children only during fever. Therapy: temperature control with salicylates and paracetamol. During seizures - transpectal administration of DZP 0.5 mg/kg in a 0.05% solution. The rinse of the oral cavity for 5 minutes with a solution of 1 mg (1 ml) of midazolam in 5-10 ml of mint water is also effective. Prevention: prevention of high fever, with infectious and licopary states - DZP Perenotally 0.5 mg/kg/day or orally 0.2-0.5 mg/kg/day. Features of the course and treatment of epilepsy of childhood since epileptogenesis in childhood is associated with immaturity of the brain, changes in the process of growing up help to reduce the brain inclination to epileptic excitement, which determines in large numbers with proper treatment of favorable prognosis, therefore the main installation in the treatment of children's epilepsy is oriented. on the possibility of achieving a smelly remission and actual recovery. According to population studies, the frequency of wrapper remission in children's epilepsy is 50–70% [6,7,11,12]. The greatest probability of cure is with focal children's idiopathic epilepsy with centractal adhesions (90–98%), orphaned -dollar epilepsy with an early onset (up to 100%). The likelihood of a lack of relapse with youth epilepsy with absans is about 80%. However, with this form, there is a risk of generalized tonic -clonic seizures after the abolition of treatment at a later age. The prognosis of youth myoclonic epilepsy in relation to the control of seizures with correctly selected therapy (valproic acid, topiramate, levetiracetes in sufficient doses) is very good, however, after canceling the therapy, the probability of renewal of seizures is 80%. The risk of relapse is equally high when canceling therapy with idiopathic generalized epilepsy with tonic -clonic seizures [12]. The prognosis for focal symptomatic epilepsy is less favorable, where the probability of achieving drug remission is 30-50% and small probability of wested -blooded remission [4,6,7,12]. These data should be taken into account when deciding on the time of possible cancellation of pharmacotherapy in the absence of seizures. In cases of idiopathic epilepsy with a well -known good forecast, a period of 2 years is conventionally accepted. With symptomatic epilepsy, this period is 3-5 years or more. In addition to the term of drug remission, an extra -intake symptoms, neuroimaging data and EEG are taken into account. The probability of relapse is much higher in the presence of mental and neuropsychological disorders and structural brain disorders. It should also be remembered that the condition for canceling treatment is the absence of epileptiform activity and pathological waves in the EEG in the area of epileptogenic focus. An important point is the amount of the cancellation of the drug: the less it is, the less likely the cancellation seizures. The dose reduction rate should not be faster than 1/4 of the daily dose per month [1.4]. With large doses of the drug taken, a single dose reduction is 150–250 mg, KBZ 100 mg, LTH and TPM 25 mg, LVTC 250 mg. There are also features of the choice of drugs and their doses associated with age. It should be remembered that almost any drug can give a paradoxical effect of weighting epileptic seizures. Especially careful should be when prescribing children FT, KBZ, OKBZ. These three drugs are contraindicated to all patients who have bilateral -synchronous epileptiform discharges in the EEG. They are not effective for absance and myoclonic epilepsy and in more than half of cases weight seizures. For example, under youthful myoclonic epilepsy, weighting is observed in 70% of patients. These drugs also weight or cause mental and behavioral disorders in childalous rolandic epilepsy, epileptic aphasia Landau -Kleffner, epilepsy with constant complexes of spike -wave in a dream. In contrast, the KBZ and OKBZ are the drugs of the optimal choice for children's occipital epilepsy with the late beginning (Gasto form). LTG always causes a weight of severe myoclonic epilepsy of infancy (drave syndrome) [2–4]. Due to the high rate of metabolism and high enzymatic activity, the elimination of the drug in children is much faster than in adults, so the necessary daily doses for kg of body weight are higher than in adults (Table 5). It should also be remembered that with duotherapy, effective doses of drugs used in addition to inducers of the liver enzymes (KBZ, FT, FB) should be increased, and with a combination with a departure that overflows the activity of the liver enzymes, in order to avoid toxic effects associated with increasing the concentration of an additional drug [1].
Literature 1. Zenkov L.R. Treatment of epilepsy (a guide for doctors). - "Remedium". M. - 2001. 2. Zenkov L. R. Anticonvulsant pharmacotherapy can aggravate the course of epilepsy // Journal of neurology and psychiatry. – 2005. – T. 105. – P. 12–16 3. Zenkov L.R. Non-paroxysmal epileptic disorders. – “MEDpressinform”.M. – 2007. 4. Zenkov L.R., Prityko A.G. Drug-resistant epilepsies. "MEDpressinform".M. – 2003. 5. Mukhin K.Yu., Petrukhin A.S., Glukhova L.Yu. Epilepsy. Atlas of electroencephalographic diagnostics. Alvarez Publishing. M. – 2004. 6. Arts Willem FM, Brouwer Oebele F., Peters AC Boudewijn et al. Course and prognosis of childhood epilepsy: 5-year follow-up of the Dutch study of epilepsy in childhood // Brain. – 2004. – V. 127. – P. 1774–1784 7. Berg AT, Shinnar S., Levy SR and Testa FM Newly diagnosed epilepsy in children: presentation at diagnosis // Epilepsia. – 1999. – V. 40. – P. 445–452. 8. Engel J., Jr. A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: report of the ILAE Task Force on Classification and Terminology // Epilepsia. – 2001. – V. 42. – P. 796–803. 9. Holmes Gregory L., Yehezkiel Ben–Ari. The neurobiology and consequences of epilepsy in the developing brain // Pediatric Research.–2001.– V. 49.– 320–325 10. Ito M., Aiba H., Hashimoto K. et al. Low-dose ACTH therapy for West syndrome Initial effects and long-term outcome // Neurology.– 2002.– V. 58.– P. 110–114 11. Kwong KL, Chak WK, Wong SN, and So KT Epidemiology of childhood epilepsy in a cohort of 309 Chinese children // Pediatr Neurol. – 2001. – V. 24. – P. 276–282. 12. Panayotopoulos CP The epilepsies. Seizures, syndromes and management. Bladon Medical Publishing. Oxfordshire. – 2005.
Callosotomy of the corpus callosum
This form of surgery is indicated when the attack involves both hemispheres. The essence of the operation is that the doctor crosses the corpus callosum (a part of the brain that allows the hemispheres to exchange information with each other). This is done to prevent epileptic activity from moving from one hemisphere to the other. Of course, such treatment is unable to eliminate the attack, but there is still a positive effect in the form of reducing its intensity. Although, it must be said, crossing the paths of information transfer from one site to the second is not the best idea, but in the absence of fish, as they say, cancer is a fish.
Before the operation, a thorough examination of the patient using MRI, ECG, EEG is indicated. In some cases, PET scan is prescribed.
The operation itself is performed under general anesthesia in two stages:
- First, the doctor crosses the anterior two-thirds of the corpus callosum. This allows the hemispheres to exchange visual information with each other.
- If the first stage has no effect, then the remaining part of the corpus callosum is intersected.
However, now there is a more effective alternative - radiosurgery. This is a non-invasive method that does not provoke complications that are possible with surgical treatment.
In general, this method is far from ideal, given the inability of the hemispheres to exchange information with each other. With drop attacks, the effectiveness is 50-75%, which is quite low. The rehabilitation period is one and a half months.
Important: removal of interhemispheric connections leads to symptoms such as a decrease in psychomotor activity, akinetic mutism (when the patient unmotivatedly refuses to engage in conversation with other people even though he can talk and understands speech. He also does not move despite being able to do this ). Usually this condition goes away on its own within two weeks. In 20% of cases there is an increase in the frequency of partial seizures. But there is no need to worry, everything goes away after a while.
Material and methods
The study included 75 patients with supratentorial brain tumors - 42 boys and 33 girls, aged from 5 months to 17 years at the beginning of observation (average - 9.6 ± 5.3 years). All of them underwent examination and treatment at the Department of Neurology, Neurosurgery and Medical Genetics of the Pediatric Faculty of the Russian National Research Medical University. N.I. Pirogov and in the departments of neurosurgery and psychoneurology No. 2 at the Russian Children's Clinical Hospital in 2005-2012. with subsequent follow-up from 1 to 6 years.
Of the 75 patients, in 52 (69.3%) cases the presence of epilepsy was identified as the main clinical manifestation of the disease. Of the 52 patients with epilepsy, surgery was performed in 25 patients using ECoG and in 27 patients without ECoG. The postoperative outcome of epileptic seizures was assessed using the Engel classification.
Before surgery, patients were carefully examined, including using magnetic resonance imaging (MRI) and EEG. MRI was performed on a GE Signa infinity machine with a field strength of 1.5 Tesla. A standard study was carried out with a slice thickness of 4 or 5 mm (depending on the size of the head) and a pitch of 2 mm, an image matrix of 512 × 512 pixels, which included various imaging modes T1 and T2 weighted SE, FSE, FLAIR, DW and GRE T2 . Anesthetic aid to ensure immobility of the patient (method of sedation with sevoflurane). Anesthesia device Aestiva-5, monitoring was carried out using a Datex-Ochmeda 5/S device. We used intravascular contrast enhancement with half-molar (gadopentenate dimeglumine, Magnevist, Schering A.G..) and monomolar (gadobutrol 1.0, Gadovist 1.0, Schering A.G..). At the Institute of Neurosurgery named after. N.N. Burdenko, the study was carried out using a Magnetom Vision 1.5 Tesla device. The research results were consulted by the head of the Department of Radiation Diagnostics of the Russian Children's Clinical Hospital, Doctor of Medical Sciences, Prof. A.A. Alikhanov.
All patients underwent at least 3 video-EEG monitoring in states of wakefulness and sleep, performed before and after surgery, intensive preoperative video-EEG monitoring according to the 10-10 scheme, as well as intraoperative corticography (pre-resection and at least one post-resection ECoG recording) . Video-EEG monitoring devices were used: Encephalan-video RM-EEG-19/26, Encephalan-RM (NPF Medicom MTD, Taganrog), Biola NS425 (NPF Biola, Moscow), Grass-Telefactor Beehive and Aura ( USA). Intensive preoperative video-EEG monitoring according to the 10−10 scheme was performed on Biola NS432 and NS450 electroencephalographs (NPF Biola, Moscow), as well as Nihon Kohden 1200K (Japan). ECoG was performed using sterile strip 6- and 10-pin subdural electrodes (AD-TECH, USA).
Surgical operations were performed on patients at the Russian Children's Clinical Hospital, Research Institute of Neurosurgery named after. N.N. Burdenko and the clinic Behandlungszentrum Vogtareuth (Vogtareuth, Bavaria). Volumetric total resections of the tumor were performed in cases where this was possible; resection of the lesion was performed depending on the general indications. For a number of tumors localized in the left (dominant) lateral temporal region, when the epileptogenic zones were outside the tumor, extended resections were performed with adjustment of the size of the resection area during the operation using intraoperative ECoG and after preliminary mapping of the pathological area of the brain. Lobectomies were performed in cases of very large tumors. Repeat surgery was performed in cases where seizures remained uncontrolled after the first surgical procedure and some tumor substrate was believed to persist, or when there was residual tumor growth or tumor recurrence. In all patients, intraoperative frameless stereotactic navigation was used to assess tumor localization.
Histological tissue samples from patients were fixed in buffered formalin and embedded in paraffin and sectioned at 3 micrometer thickness. In all cases, routine hematoxylin and eosin staining was performed, as well as immunohistochemical examination with the following antibodies to glial fibrillary acidic protein (clone EP672Y), synaptophysin (clone MRQ-40), neurofilament protein (clone 2F11), vimentin (clone V9), CD34 (clone QBEnd/10), Ki-67 (clone 30−9), total cytokeratin (clone AE1/AE3&PCK26). Immunotyping technology was provided by the ultraView Universal DAB Detection Kit. The detection system and all antibodies used were manufactured by Ventana Medical Systems, Inc., USA. Diagnoses were formulated in accordance with the current WHO classification of CNS tumors (IARC, Lyon, 2007).
For statistical processing, Fisher's exact test and Student's t-test were used. Differences having p
(for the corresponding criterion) less than or equal to 0.05 were considered statistically significant. Calculations were carried out using the statistical software package Statistica (version 7.0).
Hemispherectomy
Hemispherectomy - removal of part of the brain hemisphere, and the corpus callosum is also divided. This method shows quite good effectiveness in cases of frequent severe attacks, which are very difficult to control with medications. The operation is performed in a manner similar to callosotomy. First, the skull and dura mater are opened, and the doctor removes the part of the hemisphere that is to blame for the occurrence of attacks. After this, the corpus callosum is divided. In fact, this procedure combines lobectomy and callosotomy. As with other methods, rehabilitation lasts about 6-7 weeks.
The method is very effective, in 85% of patients there is a significant decrease in the severity and frequency of attacks, and in 60% they go away completely. There are no functional problems because the remaining brain cells take over the functions of the severed ones.
In this case, side effects are possible in the form of numbness of the head, muscle weakness of half of the body, which was controlled by the severed part of the brain, depression, and impaired cognitive functions. As rehabilitation progresses, these unpleasant effects should go away on their own.
This method also has complications. For example, the patient may have impaired sensation on the side opposite to the part of the brain that was subjected to intervention. It can also be quite difficult to move the limbs that are on this part.
Vagus nerve stimulator
This is a fairly effective treatment method that is used if conservative methods do not work. Approved for use in 1997. Its essence is very simple - a special device is implanted in a person’s lower neck, which, when connected, stimulates the vagus nerve. This method allows you to reduce the frequency and intensity of attacks by 20-40%. As a rule, it is used along with conservative methods, although the dosage of drugs in most cases can be reduced thanks to such a device.
Possible side effects of vagus nerve stimulation include dysphonia (hoarseness), sore throat, ear pain, and nausea. Most of these unpleasant symptoms can be eliminated by adjusting the degree of stimulation. Although dysphonia remains in any case. It is also worth considering that the batteries need to be changed every five years, which requires a minor operation that can be done even on an outpatient basis.
Reviews about the treatment of epilepsy
All those who choose a doctor and medical institution for consultation should first review all reviews about the treatment of epilepsy. Of course, patients' opinions can be erroneous and subjective. But in most cases it allows you to get an overall picture. Based on the reviews, conclusions can be drawn about the best centers and doctors treating this disease. But if you want to contact a particular doctor, it would also be useful to find out the opinion of your friends, if any. However, all treatment methods and medications are presented on the Internet for informational purposes only.
Epilepsy after brain surgery
In some cases, epilepsy may occur after brain surgery. We can say that this is a common phenomenon that can occur for various reasons, both related to neurosurgery and not. Thus, seizures can occur due to infection at the site of plastic surgery, for example. In this case, it is necessary to influence the root cause of the disease, since epilepsy is secondary here. We are talking about methods of treating primary epilepsy.
To prevent epilepsy after brain surgery, it is necessary to take anticonvulsant medications. However, if they occur, the matter is serious, since there is a risk of hydrocephalus, cerebral edema, blood loss, and hypoglycemia. It is also worth considering that in some cases, convulsive syndrome does not manifest itself, since the anesthesia remains in effect. Therefore, the doctor needs to monitor the patient’s condition very closely.
Rehabilitation after surgery
The patient needs to understand that surgical treatment can bring both positive and negative results. In both cases, the patient will undergo postoperative rehabilitation, but its specificity primarily depends on the results of the operation.
First aid for epilepsy
Irritation of a pathological focus in the cerebral cortex, possibly involving both hemispheres in the process, causes an attack of epilepsy.
Usually, during rehabilitation after surgery, doctors recommend that patients not stop taking antiepileptic drugs. In some clinics in Russia, doctors are of the opinion that medications should be present in the patient’s life for at least another three to five years, even after a successful surgical intervention. This will help the body suppress residual epileptic outbreaks that may occur even after treatment.
Seizures after surgery occur in the first six months. It is very difficult to judge the outcome of surgical intervention in the early stages, since seizures occur in all epileptics and they are not complications as such. However, at this time it is not entirely clear whether the operation was successful, or whether the person did not get rid of the disease.
After a considerable period of time (about a year), one can judge what results surgical treatment gave the patient. If a patient reduction in the number of attacks by one year, we can expect that in the future this positive trend will only continue, and he will be completely cured.
conclusions
We see that none of the described forms of surgical treatment of epilepsy is ideal. In most cases, it is necessary to disrupt the functioning of the brain, which in fact cannot have a positive effect on some human functions. Although the decision about whether to resort to surgical intervention is made only as a last resort, according to the principle: “of two evils, the lesser.” In most cases, drug therapy will be sufficient.
We see that even if drug therapy does not work, it is still used, it’s just that surgery is added to it.
Possible risks and complications after surgery
Surgical treatment of epilepsy always involves unconditional risks associated, first of all, with the fact that the intervention is performed on the brain. And complications that arise after surgery are not only possible, they are even predicted.
Surgical problems
This includes various complications associated with the operation. These include bleeding, infection, and difficulty recovering from anesthesia. All of this can occur both during and after the intervention.
Neurological problems
If important nerves or areas of the brain are damaged, there is a risk that the patient will have impaired vision, speech, memory or motor activity. This can happen immediately after surgery or some time later. And this is not always a temporary consequence of anesthesia: sometimes a person becomes disabled for life.
Functional problems
They are associated with the ineffectiveness of the operation. Relapses after surgical treatment of epilepsy are not uncommon. And in some cases, the situation worsens, and the seizures become more severe or occur more frequently.
The doctor must tell the patient about all possible risks and complications before the operation. A person must weigh the pros and cons and make a decision. If you refuse intervention, you will have to write a written statement, especially if the epilepsy is severe and each attack can be fatal.