Surgery in the area of the brain and spinal cord is considered one of the most dangerous in medical practice, and is therefore associated with a number of side effects and complications. To eliminate them and prevent the patient’s well-being from deteriorating, competent and timely rehabilitation under the guidance of experienced doctors is required.
Specialists at the Blagopoluchie medical and social rehabilitation center provide assistance to patients with disabilities of any degree of complexity. A comprehensive recovery program is based on an individual approach and consists of various aspects: medical, psychological and social. At each stage, the patient has access to consultations with highly specialized specialists. Direct control over the effectiveness of recovery and the general condition of the patient is carried out by a rehabilitation physician.
Diagnosis of brain tumors
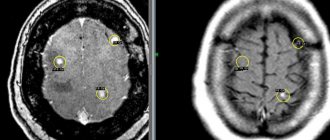
The primary method used to indicate problems is radiographs. However, this study in the diagnosis of brain tumors is considered to be of little information, so specialists at the Oncology Center of the Yusupov Hospital prefer more effective and accurate methods - magnetic resonance imaging (MRI) and computed tomography (CT). In addition, positron emission tomography (PET) is part of a comprehensive examination to detect a brain tumor. The use of these diagnostic methods ensures the correct diagnosis, thanks to which the most effective treatment program is selected.
Neurosurgeons
In Moscow, operations for brain cancer are performed on our patients by experienced and highly qualified surgeons with an excellent reputation and extensive international experience. Among the doctors we can invite for surgery are Professor Alexey Krivoshapkin, one of the world's best experts in brain tumor removal, Professor Evaldas Chesnulis from Switzerland, who masterfully performs brain surgery, we can also refer you to Professor Vladimir Krylov, chief neurosurgeon RF. Both examination and operations are carried out according to modern international protocols using the most advanced techniques. Other leading neurosurgeons are certainly Albert Sufianov, an outstanding Russian doctor, included in the Top 100 of world neurosurgery, the doctor worked in Japan for 16 years. Dr. Sufianov specializes in neurosurgery of tumors, cysts and abscesses, as well as the treatment of hydrocephalus, craniosynostosis and vascular malformations. The doctor is a master of endoscopic neurosurgery, one of the few in the world.
Surgeries for childhood brain cancer are a separate specialization. We can involve such specialists in treatment - these are pediatric doctors Dr. Valentin Palm, a well-known specialist in the Russian Federation, Dr. Shlomi Konstantini, an Israeli specialist, to whom children are taken even from the almighty USA and Germany.
What do you get when you seek treatment from us:
- quick and accurate understanding of your problem,
- carrying out all diagnostic measures as soon as possible,
- our consultant is always in touch with you,
- the right strategic decision from a council of top-class specialists, the decision is made not by one doctor, but by the heads of departments and clinics: leading specialists in your problem areas, a specialized surgeon if necessary, a diagnostician - an Israeli general practitioner,
- the best treatment option in the Russian Federation according to international standards, these are the most qualified doctors, and their work according to Western standards, guaranteeing the best result,
- solving all problems at all stages, that is, Dr. Aronov is always “with you”, for everything we will offer the best solution,
- peace of mind, clear steps in treatment - you get all the benefits of Israeli and European medicine in Russia, care of an Israeli doctor in Russia.
Surgery to remove a brain tumor
Removal of a brain tumor (complete or partial) by surgery is the main method of treating cancer.
- stereotactic surgery – this method provides the most accurate access to the affected area of the brain
- shunting - installation of a shunt (a tube connecting the vessels and the cavity) helps restore spinal cerebrospinal fluid, the disruption of which can cause headaches, nausea and other symptoms characteristic of spinal hypertension
- HIFU treatment for brain tumor. The essence of this method is to expose the pathological focus to high-power ultrasound, due to which the tumor is destroyed. After the procedure, the remaining fragments of the tumor are removed.
Surgical treatment of brain tumors is usually complemented by chemotherapy and radiation therapy, after which the patient requires a course of rehabilitation treatment, which can be carried out at the rehabilitation center of the Yusupov Hospital.
Clinical picture
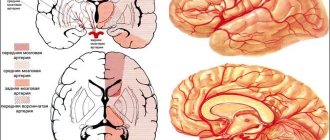
The clinical manifestations of brain tumors are determined by their location in a limited volume of the cranial cavity. Compression or destruction of brain tissue in the tumor area (due to tumor growth) causes the so-called primary, or focal, symptoms. As the disease progresses, so-called cerebral symptoms appear, caused by impaired hemodynamics and intracranial hypertension.
Focal symptoms
Focal symptoms are largely determined by the location of the tumor. The following groups can be distinguished:
Sensory impairment
The ability to perceive external stimuli acting on the skin - thermal, painful, tactile - decreases or disappears. The ability to determine the position of parts of one's body in space may be lost. For example, with his eyes closed, the patient is unable to tell whether he is holding his hand with his palm up or down.
Memory impairment
When the cerebral cortex responsible for memory is damaged, complete or partial memory loss occurs. From not being able to recognize your loved ones to not being able to recognize or recognize letters.
Motor disorders (paresis, paralysis)
Muscle activity decreases due to damage to the pathways transmitting motor impulses. Depending on the location of the tumor, the pattern of the lesion differs. Both lesions of individual parts of the body and complete or partial lesions of the limbs and torso can develop. When the transmission of motor impulses from the cerebral cortex is disrupted, central type paralysis occurs, that is, a signal is received from the spinal cord to the muscles, they are in hypertonicity, but control signals from the brain do not enter the spinal cord, voluntary movements are impossible. When the spinal cord is damaged, peripheral paralysis develops; the signal from the brain enters the spinal cord, but the spinal cord cannot transmit it to the muscles, and the muscles are hypotonic.
Epileptic seizures
Convulsive seizures appear due to the formation of a focus of congestive excitation in the cortex.
Hearing and speech recognition impairment
When the auditory nerve is damaged, the ability to receive signals from the hearing organs is lost. When the area of the cortex responsible for recognizing sound and speech is damaged, for the patient all audible sounds turn into meaningless noise.
Impaired vision, object and text recognition
When the tumor is located in the area of the optic nerve or quadrigeminal region, complete or partial loss of vision occurs due to the inability to deliver a signal from the retina to the cerebral cortex. When areas in the cortex responsible for image analysis are damaged, a variety of problems occur, ranging from the inability to understand incoming signals to the inability to understand written language or recognize moving objects.
Speech impairment, oral and written
When areas of the cortex responsible for written and oral speech are damaged, their complete or partial loss occurs. This process, as a rule, is gradual and intensifies as the tumor grows - at first the patient’s speech becomes slurred (like that of a 2-3 year old child), his handwriting gradually changes, then the changes increase until it is completely impossible to understand his speech and handwriting in the form of a jagged line.
Autonomic disorders
Weakness and fatigue appear, the patient cannot get up quickly, he becomes dizzy, and fluctuations in pulse and blood pressure occur. This is due to impaired control of vascular tone and the influence of the vagus nerve.
Hormonal disorders
The hormonal background changes, the level of all hypothalamic-pituitary-dependent hormones may fluctuate.
Loss of coordination
When the cerebellum and midbrain are damaged, coordination is impaired, gait changes, and the patient is unable to make precise movements without vision control. For example, he misses when trying to reach the tip of his nose with his eyes closed. The patient is unstable in the Romberg position.
Psychomotor and cognitive impairment
Memory and attention are impaired, the patient becomes distracted, irritable, and his character changes. The severity of symptoms depends on the size and location of the affected area. The spectrum of symptoms ranges from absent-mindedness to complete loss of orientation in time, space and self. Episodes of psychomotor agitation and confusion are possible.
Intellectual and emotional disorders
When the brain is damaged due to space-occupying formations, intellectual functions and those personal characteristics that reflect the characteristics of social interaction are most affected: social conformity and psychoticism. The lateral features of this effect are that when the functions of the left hemisphere are impaired due to the development of a tumor, psychoticism increases to a greater extent, and when there is a deficit in the functioning of the right hemisphere, social conformity increases. Hemispheric features in changes in cognitive status in cases of space-occupying brain lesions are less pronounced than changes in personal characteristics. It should be noted, however, that damage to the left hemisphere causes a relatively greater decrease in intelligence, and to the right hemisphere - in creativity indicators.
Hallucinations
When areas in the cerebral cortex responsible for image analysis are damaged, the patient begins to hallucinate (usually simple: the patient sees flashes of light, a solar halo). The patient hears monotonous sounds (ringing in the ears, endless knocking).
General cerebral symptoms
General cerebral symptoms are symptoms that occur when intracranial pressure increases and compression of the main structures of the brain.
Headache
A distinctive feature of oncological diseases is the constant nature and high intensity of headaches, and their poor response to non-narcotic analgesics. Reducing intracranial pressure brings relief.
Vomiting (regardless of food intake)
Vomiting of central origin usually occurs due to an effect on the vomiting center in the midbrain. Nausea and vomiting constantly bother the patient; changes in intracranial pressure trigger the gag reflex. Also, the patient is unable to eat food and sometimes drink water due to the high activity of the vomiting center. Any foreign object that lands on the root of the tongue causes vomiting.
Dizziness
May occur as a result of compression of the cerebellar structures. The functioning of the vestibular analyzer is disrupted, the patient has central type dizziness, horizontal nystagmus, and often has the feeling that he, while remaining motionless, is turning or moving to one side or another. Dizziness can also be caused by tumor growth, leading to a deterioration in blood supply to the brain.
Removal of a brain tumor: consequences
Any surgical intervention is accompanied by poor health after it. As a rule, patients complain of dizziness and confusion. These symptoms are episodic, appearing and disappearing on their own.
The development of potential side effects depends on factors such as:
- type of operation
- tumor localization
- neurological status of the patient before surgery
- general health of the patient
- complete or partial removal of the tumor was performed
- whether healthy tissue was damaged during the operation.
The main possible undesirable consequences include the following:
- development of bleeding (intra- or postoperative), which is accompanied by neurological changes
- the occurrence of pain - to relieve it, specialists at the Yusupov Hospital prescribe analgesics of the latest generation
- development of edema in the incision area (disappears after 2-4 days)
- wound infection - to prevent the development of this complication, patients are prescribed antibacterial drugs
- swelling of brain tissue: relieved by taking corticosteroids, one of which is dexamethasone, a hormonal drug that has an immunomodulatory, anti-inflammatory, antiallergic and membrane-stabilizing effect. Dexamethasone for brain tumors is used as a decongestant drug that helps reduce intracranial pressure;
- development of neurological disorders that prevent the restoration of normal neurological function;
- the occurrence of seizures and convulsive syndrome, which can be prevented by taking anticonvulsants;
- thrombus formation - to reduce the risk of blood clots, specialists at the Yusupov Hospital recommend changing the patient’s body position in the postoperative period and developing special exercises for the legs. In addition, the patient must stop smoking;
- hydrocephalus – if this complication occurs, the patient needs endoscopic ventriculostomy, drainage installation, and shunting;
- leakage of cerebrospinal fluid through the incision made for the operation - another surgical intervention is performed to restore the flow of cerebrospinal fluid;
- divergence of the edges of the staples installed to fasten the edges of the postoperative wound - to prevent this complication, the patient must refrain from physical activity for one to one and a half months after surgery.
Malignant tumors are primary and secondary:
The most common primary brain tumor is glioma.
In adult patients, gliomas are the most prominent type of brain tumor, accounting for approximately 37% to 45% of all brain tumors.
Additionally, gliomas are characterized depending on what type of cells they consist of:
Astrocytoma is a tumor that develops from stellate glial cells called astrocytes. In adults, astrocytomas usually develop in the forebrain. In children, they are found in the brain stem, forebrain and cerebellum.
Grade III (G III) astrocytoma is sometimes called anaplastic astrocytoma. Astrocytoma with grade IV (G IV) is usually called glioblastoma multiforme.
- GI (pilocytic astrocytoma): slow growing, low propensity to invade surrounding brain tissue. Most common in children and adolescents.
- G II (diffuse astrocytoma): has non-progressive growth, some tendency to penetrate into surrounding brain tissue. Found mainly in young adults.
- G III (anaplastic/malignant astrocytoma): These tumors grow relatively quickly compared to previous ones, and tend to invade surrounding brain tissue.
- G IV (glioblastoma multiforme, GBM): an extremely aggressive form of malignant brain tumor. Unfortunately, it is the most common form of all brain tumors in adults, accounting for 54% to 67% of all astrocytomas.
- Brainstem glioma is a tumor that forms from the lowest part of the brain. Brainstem gliomas are diagnosed mainly in young children and middle-aged people.
- Ependymoma. This tumor develops from cells that line the ventricles of the brain or the central canal of the spinal cord.
- Oligodendroglioma. This is an exceptional tumor that develops from cells that produce a fatty substance that covers and protects nerves.
Radiation therapy for brain cancer
One of the most effective methods of treating cancer pathologies is radiation therapy. Radiation therapy for brain tumors helps to reduce the size of the tumor if it is not possible to completely remove it.
This method is based on irradiation of the affected area of the brain. However, it is necessary to understand that radiation has a detrimental effect on all cells of the body, including healthy ones. But pathological cells are more sensitive, so this effect is more pronounced for them.
Radiation therapy is used to treat both benign and malignant tumors. It is often combined with surgical treatment and chemotherapy.
Radiation therapy for brain tumors can be carried out in several ways:
- traditional - involves remote irradiation, in which the head of the device is placed at a certain distance from the patient’s head;
- brachytherapy - radioactive material is implanted directly into the tumor, so the tumor is irradiated from the inside;
- targeted irradiation method - a narrow, thin beam of radiation is used. To carry out this method, a gamma and cyber knife is used.
Treatment
Treatment of brain tumors, like all cancers, must be comprehensive. All activities carried out during the course of treatment can be divided into the following groups.
Symptomatic therapy
All measures belonging to this group do not affect the cause of the disease itself, but only soften its course, allowing the patient to live or improve his quality of life.
- Glucocorticosteroids (prednisolone, dexamethasone) - relieve swelling of brain tissue and reduce cerebral symptoms.
- Antiemetic drugs (metoclopramide) - relieve vomiting that occurs as a result of an increase in cerebral symptoms or after combined chemo-radiation therapy.
- Sedatives are prescribed depending on the level of psychomotor agitation and the severity of mental disorders.
- Nonsteroidal anti-inflammatory drugs (NSAIDs - for example, ketonal) - relieve pain.
- Narcotic analgesics (morphine, omnopon) - relieve pain, psychomotor agitation, and vomiting of central origin.
Surgical treatment of tumors of the brain and spinal cord is the main, most effective method, but removing a tumor from brain tissue presents significant difficulties. Each such intervention is a complex neurosurgical operation. Since the surgeon needs to excise the tumor within healthy tissue (to avoid relapse), each such operation is traumatic, and often completely impossible due to the large size of the tumor or its localization in vital areas of the brain. Depending on the size, location, type of tumor, and the patient’s condition, a decision is made on the need for surgery, the extent of surgery and the method of performing it. The use of modern laser and ultrasound technology in brain tumor surgery has made it possible to slightly increase its effectiveness. The specific route of intervention and the method of its implementation is individual and depends on the location of the tumor, its size and cellular composition.
Radiation therapy
Radiation therapy plays an important role in the treatment of brain tumors. Radiation therapy can be carried out both in addition to surgical treatment, and independently in cases where surgical treatment is impossible or the patient refuses surgical intervention. When planning radiation therapy for patients with brain tumors, it is very important to determine the rational amount of radiation. For this purpose, it is necessary to use data obtained during surgery, pre- and postoperative computed tomography, magnetic resonance imaging, angiography, and positron emission tomography. Determining a rational level of radiation will avoid or minimize the negative consequences of therapy. The effect of radiation therapy is based on the effect of ionizing radiation on tissue cells located in the path of the radiation beam. External beam radiation therapy is used to treat brain tumors. The optimal start time is 14-21 days after surgery, and preferably no later than 2 months. Radiation is administered locally to the area of the tumor itself, the tumor bed, residual tumor, relapse or metastasis. It is also possible to conduct total irradiation to the entire brain for multiple (>3) metastases or certain histological types of tumors (glioblastoma, astrocytoma, and others). Radiation therapy is usually carried out in one course of 10-30 fractions (procedures), the total isoeffective (that is, equivalent to a dose with fractionation of 2 Gy) dose of ionizing radiation for total irradiation of the brain should not exceed 50-60 Gy, for local irradiation - 70 Gy . The size of a single radiation dose (per 1 session) ranges from 0.8 to 3 Gy. Radiation therapy is selected individually depending on the cellular composition of the tumor, its size and location. Despite its effectiveness, radiation therapy is a rather difficult procedure for the patient; its use is accompanied by radiation reactions, which are usually relieved by corrective anti-edematous therapy. Depending on the types of tumors, various schemes of radiation therapy and combinations with chemotherapy are formed.
Radiosurgery
Stereotactic radiosurgery is part of radiation therapy, but due to its increasing importance for the treatment of brain tumors, it deserves special attention. Stereotactic radiosurgery was first used by Swedish neurosurgeon Lars Leksell in 1969 as a substitute for surgery for patients in whom surgery is contraindicated or undesirable due to a high risk of complications. Radiosurgery uses a combination of the advantages of stereotactic navigation (spatial navigation with submillimeter precision) and the selective action of ionizing radiation specifically on tumor cells, characteristic of radiation therapy. This makes it possible to achieve complete destruction of the tumor focus without invasive, highly traumatic surgical treatment, but with minimal complications compared to classical radiation therapy. The main cases when radiosurgery is indicated are: metastatic brain damage (with the identified primary tumor localization and a small number of metastases), recurrence of the primary brain tumor after surgical and/or radiation treatment. For benign brain tumors, radiosurgery is a complete alternative to surgical treatment and is considered the method of choice for the patient. In case of contraindications or refusal of surgical treatment, radiosurgery can be performed as an independent method of treatment if there is histological verification of the diagnosis. Sometimes it is possible to perform radiosurgery in combination with total brain irradiation.
Chemotherapy
Before chemotherapy, it is necessary to carry out histological verification of the tumor to select an adequate dose and the most effective drug. If surgery has not been performed, the diagnosis should be confirmed by stereotactic biopsy. The use of chemotherapy is significantly limited by the small number of drugs that penetrate the blood-brain barrier. A prerequisite for chemotherapy is to determine the patient's individual sensitivity to the drug. The route of administration is selected based on the possibility of creating the highest concentration of the drug in the tumor tissues. For chemotherapy, drugs of the alkylating group, antimetabolites, drugs of natural origin, antiblastic antibiotics, synthetic and semi-synthetic drugs are used. The most effective chemotherapy is combined with radiation therapy and a course consisting of several drugs.
The drugs are administered in courses lasting from 1 to 3 weeks, at intervals of 1-3 days, until the entire prescribed dose of the drug is administered. The drug is administered under the control of the blood picture, since all drugs used in therapy affect the most actively dividing cells, including bone marrow cells. Based on the results of the tests, the course of therapy may be interrupted, and in some cases even cancelled. Concomitant antiemetic therapy is also of great importance for the patient. An important parameter from the point of view of the patient’s quality of life is emetogenicity - the ability to induce vomiting. High emetogenicity indicates that 90% of those receiving the drug without antiemetic therapy experienced vomiting. According to this criterion, 4 groups are distinguished:
- > 90% – high
- 30-90% - average
- 10-30% - low
- < 10% - minimum
Adequacy of antiemetic therapy is achieved by a combination of drugs that inhibit the activity of the vomiting center, together with sedatives. The choice of a specific combination depends on individual sensitivity, duration of chemotherapy and financial capabilities.
Cryosurgery
The goal of cryosurgery is cryodestruction of cells in a given volume of frozen pathological tissue, both on the surface of the body and deep in the organ, without damaging surrounding healthy cells. There are two main types of devices used in cryosurgery: cryoapplicators and cryoprobes. Cryoapplicators are designed for the destruction of large amounts of biological tissue, since they are in contact with the surface of the frozen object and are quite large in size. Therefore, cryoapplicators are widely used in dermatology, mammology, gastroenterology and liver surgery. Cryoprobes are used for minimally invasive effects deep in a tissue or organ on a small pathological focus, when gentle treatment of surrounding tissues is necessary. Cryosurgery for brain tumors can either complement the main stage of surgical removal or be an independent type of treatment of tumor tissue. Cryodestruction is used for: 1. tumors located in functionally significant areas of the brain. 2. tumors that cannot be removed by traditional surgical methods. 3. deeply located multiple formations (metastases to the brain). 4. unremoved tumor fragments (residual meningioma tissue). 5. tumors of the chiasmal-sellar localization. 6. metastatic lesions of the vertebrae. Cryosurgery can be combined with radiation or chemotherapy and conventional surgery.
The cryosurgical method has a wide range of exposure volumes and is also relevant for hard-to-reach or widespread tumors, especially in elderly patients and in the presence of concomitant diseases.
Combination of radiation and chemotherapy
Recent clinical studies have shown that for low-grade gliomas, higher three-year survival is achieved with a combination of radiation and chemotherapy. Such gliomas can progress over time to stages III-IV, turning into glioblastoma.
The question of which agent is most effective for treating gliomas is controversial. A phase II study conducted jointly by Ohio University Cancer Center and the University of Maryland, Ontario, shows that combining radiation therapy with temozolomide chemotherapy improves prognosis compared with a control group that received radiation therapy alone. Patients with low-grade gliomas and a high risk of recurrence showed a three-year survival rate of 73% in the study when treated with simultaneous chemotherapy and radiation therapy. In the control group receiving radiation therapy alone, the three-year survival rate was 54%.
Radiation therapy to the brain: consequences
Radiation therapy, like other treatments, has side effects due to the fact that healthy cells are also adversely affected by radiation exposure to the brain. The effects of radiation therapy disappear as the patient’s body recovers.
Most often, patients complain of the following symptoms:
- burns, spots and redness on the skin;
- fatigue and weakness;
- nausea and vomiting;
- hair loss;
- decreased appetite.
A competent scheme of rehabilitation treatment, selected by specialists from the Yusupov Hospital individually for each patient, ensures rapid relief from these negative consequences in a short time.
Operation efficiency
In 2000, it was found that surgical treatment of certain forms of epilepsy (temporal lobe epilepsy, for example) is equivalent to an additional year of conservative treatment for this disease. In addition, drug treatment turned out to be 8 times less effective compared to surgical treatment. 64% of patients who lay on the operating table were able to completely get rid of attacks.
If a person meets all the indications for surgical treatment, then it should be started as soon as possible. A possible consequence of the operation may also be that the person is unadapted to life without seizures. Therefore, surgical intervention must be carried out together with medical and social rehabilitation.
It is also worth remembering that the patient always takes a small, but still risk. Even if he is an ideal candidate for surgery, personality changes or cognitive impairment may occur. However, this is not an argument in favor of not needing treatment. The doctor must choose a specific method of therapy on an individual basis.
Also, you should not completely abandon conservative treatment. Even if the surgery gives a good result, you must take antiepileptic drugs for 2 years. This is necessary for the brain to adapt. Although in some cases this rule can be neglected by the doctor’s decision.
Patient reviews
Natalya Semyonovna: Professor Krivoshapkin performed an operation on my son, it was a craniotomy, and it just so happened that this trouble came. And the doctor coped with it, now the situation is normal, and all thanks to the skill of the surgeon.
Anton Mikhailovich Nosov: When I was diagnosed with a brain tumor, there was a very careful approach to the best treatment, that is, to the most effective option. Fortunately, it turned out that the nature of the small tumor was such that radiotherapy was sufficient, which is what they did to me in Moscow. I chose the best option thanks to Dr. Aronov.