Non-occlusive hydrocephalus: symptoms, treatment and factors determining its development
Pathological conditions of the brain pose a threat to the health and life of patients. Their list includes non-occlusive hydrocephalus. The development of a neurological disease occurs against the background of an excess of cerebrospinal fluid, called cerebrospinal fluid, in the ventricular system of the brain. Patients of all age categories, including newborn infants, are at risk. People call this dangerous disease dropsy.
Treatment
The most common treatments since the 50s are bypass surgery and endoscopy. At the same time, for the last three decades, endoscopy, which appeared in the 80s, has occupied a leading position. Both of these operations are aimed at restoring normal circulation of cerebrospinal fluid.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
Bypass surgery, in particular, has a large number of disadvantages. The number of revisions after bypass surgery is at least two, and a person’s life depends entirely on the proper operation of the shunt. In addition, in almost half of the cases bypass surgery is fraught with complications. Therefore, endoscopy is currently the priority and most progressive direction of treatment.
Neuroendoscopic operations are also very effective, in particular, ventriculocisternostomy of the bottom of the third ventricle, during which pathways for the outflow of cerebrospinal fluid into the cisterns of the brain are artificially created. During this process, the secretion is reabsorbed, and the absence of foreign bodies (as with bypass surgery) minimizes the risk of complications and infections.
The least popular method is external drainage. It represents the removal of liquor from the outside. This method is extremely risky, associated with a high probability of infection and a huge number of complications.
With successful surgical intervention, a person has the opportunity to recover and return to a normal, fulfilling life. However, often even surgical intervention can only slow down the progression of the disease.
Causes of pathology
The development of brain pathology is determined by a number of factors. Their list includes:
- impaired blood flow to the brain, stroke;
- birth injuries and skull damage due to road accidents, emergency situations, head impacts;
- aneurysm rupture;
- congenital pathologies of the central nervous system;
- inflammatory processes of the meningeal membranes and parenchyma of the brain, ependyma of its ventricles;
- alcohol poisoning, intoxication of the body;
- neoplasms and vascular pathology of the brain;
- arterial hypertension and pathologies of the endocrine system.
An increase in excess volume of cerebrospinal fluid causes the progression of the disease. In infants, non-occlusive hydrocephalus of the brain most often occurs as a result of infections suffered by the mother during gestation.
Carrying out prenatal examinations can prevent the development of neurological pathology in a newborn child.
Symptoms of the disease
A neurological disease has pronounced symptoms caused by impaired brain function. Signs of non-occlusive hydrocephalus include:
- increase in head circumference;
- increased irritability, drowsiness, lethargy, nausea, gag reflex;
- severe headaches, cramps and rolling of the eyeballs downward;
- blurred vision, blurred vision;
- involuntary urination;
- deterioration of gait, problems with coordination of movement, body balance;
- memory loss, decreased performance, deterioration of attention;
- inappropriate behavior and lack of ability to self-care.
The presence of non-occlusive hydrocephalus in newborn babies can also be indicated by a number of signs, such as a disproportionately large forehead, thinned skull bones, eyebrows hanging over the eyes, a swollen fontanelle, veins visible on the head, and strabismus. Knowing what it is, parents will always be able to detect the symptoms of pathology and provide effective treatment to their children in a timely manner.
If signs of a neurological disease that is dangerous to the health or life of patients appear, urgently seek the help of qualified specialists.
Timely treatment is the key to obtaining a positive result in an adult patient or child, and also eliminates the risk of death.
Clinical manifestations of acute dropsy
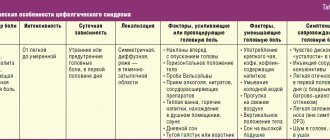
External hydrocephalus of the brain in adults leads to significantly increased pressure inside the skull. The presence of neurological disorders indicates the progression of dropsy. Symptoms of hydrocephalus in adults include:
- feeling of heaviness in the head;
- nausea;
- vomit;
- headache of varying intensity;
- hiccups;
- feeling of squeezing of the eyeballs;
- drowsiness;
- yawn;
- instability of blood pressure;
- cardiopalmus;
- increased sweating;
- presence of dark circles under the eyes.
Such people always have a headache. This is the main manifestation of cerebral hydrocele. Increased pain is observed in the morning. This is due to the fact that during sleep the pressure increases even more. Moderate hydrocephalus is manifested by mild pain. Nausea and vomiting are almost always observed.
Dropsy leads to disruption of the heart. It starts beating faster or slower. With acute dropsy of the brain, dislocation syndrome sometimes develops. It is caused by displacement of structures and nerve fibers in the brain area. This manifests itself as depression of consciousness. In the absence of proper assistance, coma develops.
Mixed hydrocephalus of the brain is very dangerous, in which compression of the areas responsible for the functioning of the heart and respiratory organs occurs. This can cause death. In severe cases of hydrocephalus, neurological symptoms appear. These include: visual disturbances, impaired gait and coordination of movements, changes in handwriting, paresis, paralysis, decreased vision, contractures, dizziness, tinnitus.
Types of pathology
The classification criteria for non-occlusive hydrocephalus include a number of factors:
- The period of development of neurological pathology.
- Location of cerebrospinal fluid.
- Timing of manifestation and rate of progression of disease symptoms.
- The number of dilated ventricles of the GM.
- ICP level.
Based on the time of appearance of excess cerebrospinal fluid in the ventricular system of the brain, a neurological disease of congenital and acquired type is distinguished. In the first case, the pathology is diagnosed during the period of intrauterine development of the fetus. The acquired form of neurological disease develops under the influence of external factors, including infection, injury, and inflammatory processes in the brain.
The location of the cerebrospinal fluid determines the diagnosis of internal and external varieties of hydrocele. In the first case, the development of pathology is associated with an excessive content of cerebrospinal fluid in the gastric system of the brain. External non-occlusive hydrocephalus is diagnosed when cerebrospinal fluid accumulates in the subarachnoid space.
The timing of the manifestation of symptoms of a dangerous brain disease determines several forms of its development. Its acute form indicates the development of the pathological process up to 72 hours. The progressive or subacute form of the disease manifests itself within 30 days. The period of development of chronic hydrocephalus varies from 21 days to six months.
Based on the rate of progression of pathological signs, active, passive and regressive stages of the disease are distinguished. The first of them occurs with clearly expressed signs and a rapid increase in the volume of excess cerebrospinal fluid. Passive or stabilized hydrocephalus is characterized by the absence of an increase in the clinical picture of the pathology. When diagnosing a regressive stage of a neurological disease, the disappearance of its symptoms without treatment is noted.
In addition, internal non-occlusive hydrocephalus can be of asymmetric or symmetric type. The number of dilated ventricles is the basis for the classification of the disease. In the first case, excess cerebrospinal fluid will be observed in one of them. Symmetric hydrocephalus indicates enlargement of both ventricles of the brain. The level of ICP makes it possible to identify hypertensive, normotensive and hypotensive forms of the disease.
Diagnosis of the disease
The pronounced symptoms of non-occlusive hydrocephalus provide an opportunity for doctors to identify the disease during the first examination of the patient. After collecting anamnesis, clarifying past infections, and skull injuries, a comprehensive examination is prescribed. Its purpose is to determine the onset and form of development of the pathology. The list of diagnostic measures includes:
- radiography of the skull;
- echoencephalography, which is an ultrasound aimed at determining the degree of increase in intracranial pressure;
- computed tomography and MRI aimed at identifying vascular disorders of the brain;
- PCR diagnostics, prescribed for the diagnosis of congenital dropsy of infectious origin in order to determine the type of causative agent of pathogenic microflora;
- consultation with an ophthalmologist necessary to assess visual impairment;
- spinal puncture, cerebrospinal fluid analysis.
The results of diagnostic studies help determine the onset and course of the pathology, as well as decide the feasibility and effectiveness of drug therapy or surgery.
It is not recommended to postpone indefinitely a visit to a neurologist when the first symptoms of the disease are detected.
Good to know
During normal functioning of the body, cerebrospinal fluid is absorbed by the tissues. The slightest failure in this process can lead to excessive release of cerebrospinal fluid, as a result of which it will not have time to be absorbed by the tissues and will begin to put pressure on the brain, which will lead to increased intracranial pressure and the development of the disease.
Bypass surgery is impossible if the dropsy resulted from hemorrhage in the lateral ventricles (so-called post-hemorrhagic hydrocephalus), since the cerebrospinal fluid contains blood, the entry of which into the abdominal cavity is fraught with serious complications.
The use of endoscopy in such a clinical picture also does not always end positively, since the hole formed during the operation quickly closes due to inflammation of the ventricles.
This disease is one of the most difficult that a child can face. The most favorable prognosis awaits patients with a mild form of hydrocephalus. When a disease is detected at an early stage of development, it is much easier to combat it.
Possible complications
The lack of timely effective treatment for non-occlusive hydrocephalus of the brain causes the development of complications and irreparable consequences. Among them it is necessary to note:
- delayed psychomotor development of children;
- attacks of severe headache;
- severe complications that negatively affect the development of speech, hearing, and vision;
- retardation in mental and physical development;
- loss of ability to work;
- epilepsy, coma and death.
Timely diagnosis of pathology provides an opportunity to avoid the development of complications that reduce the quality of life of small and adult patients.
Consequences and complications
The consequences of the lack of surgical intervention and progression of the disease may be the following:
- decrease in visual or its complete loss;
- respiratory dysfunction ;
- loss ;
- metabolic disease ;
- atrophy ;
- probability of death ;
- disturbances in the functioning of the heart and its blood supply;
Usually, as a result of bypass surgery, people live normally with the shunts implanted as a result of the operation. They lead a normal, measured lifestyle. After a few years, if the clinical picture is moderate, the shunt can be removed, and if hydrocephalus does not occur again, then there is a possibility of complete recovery.
As you know, it is easier to prevent a disease than to cure it. Among the work important for preventing the occurrence of this disease are the prevention of severe infections, such as meningitis (inflammation of the soft meninges), encephalitis (inflammation of the brain), syphilis (a sexually transmitted infectious disease affecting the skin, mucous membranes, internal organs, bones, nervous system ). It is also recommended to avoid stressful situations and overwork.
Treatment of the disease
To effectively solve the problem of excess cerebrospinal fluid in the ventricular system of the brain, drug therapy and surgical intervention are used. Treatment with pharmaceutical drugs is aimed at eliminating the initial stages of the disease. Their list includes medications whose action is aimed at reducing ICP, removing excess fluid, and also improving the nutrition of brain cells. In case of diagnosing acute or chronic forms of pathology, surgical operations are prescribed. These include:
- external ventricular drainage, which makes it possible to ensure the outflow of cerebrospinal fluid and administer blood thinners;
- cerebrospinal fluid shunting, based on the removal of excess volumes of cerebrospinal fluid using a system of valves and tubes in the patient’s body cavity, including the atrium, peritoneum, etc.;
- endoscopic plastic surgery of the interventricular foramen, aimed at freeing the natural outflow pathways of cerebrospinal fluid from the lateral ventricles.
The form and stage of development of the pathologist determines the method of treatment.
Causes of the disease
Hydrocephalus can be congenital or acquired and can be caused by a variety of internal and external factors.
Shunting for hydrocephalus of the brain
Hydrocephalus is a life-threatening disease.
The most common causes of congenital hydrocephalus are considered to be:
- inflammation of the meninges suffered in the womb
- deviations in brain development as a result of pathology of fetal formation;
- cerebral hemorrhage suffered in the womb
- taking potent medications .
In such a situation, the occurrence of this disease cannot be ruled out. The development of the disease is characterized by brain deformation. As the disease progresses, the patient's brain changes significantly in size and becomes smaller than the volume of the cranium.
The space freed up as a result of the reduction in brain size is filled with the produced cerebrospinal fluid. At the same time, the size of the skull increases due to an increase in intracranial pressure, and its walls and bone tissue become narrower. At the same time, the patient’s blood circulation is also impaired.
The causes of acquired hydrocephalus may be as follows:
- malfunction of the body due to exposure to toxins;
- infectious disease (measles, meningitis, etc.) that occurs with complications;
- due to diseases spread by parasites ;
- benign and malignant tumors;
- stroke;
- thrombus formations in the blood vessels of the brain.
One of the factors described above is enough to disrupt the production of this secretion, which will inevitably lead to the occurrence of this disease.
Disease prevention
Carrying out preventive measures can significantly reduce the risk of diagnosing hydrocele. Their list includes:
- regular prenatal examination;
- vaccination against infectious diseases, complications after which the outflow of cerebrospinal fluid is disrupted;
- compliance with safety rules when riding bicycles, scooters, skateboards, and playing with children;
- timely neurological diagnostics.
It is recommended to pay special attention to preventive measures.
Patients should always remember that timely, qualified medical care when signs of cerebral hydrocele are detected will help maintain health, ability to work and eliminate the risk of death.
Source of the article: https://mozgexpert.ru/zabolevaniya/gidrocefaliya/neokklyuzionnaya-gidrocefaliya
Internal hydrocephalus of the brain
Impaired production, absorption or circulation of cerebrospinal fluid causes the development of hydrocephalus. The disease is characterized by the accumulation of excess amounts of cerebrospinal fluid in the cavities of the brain. At the Yusupov Hospital, all conditions have been created for the treatment of patients suffering from internal hydrocephalus of the brain:
- cozy rooms of different comfort classes;
- examination using modern diagnostic devices from leading companies in the world;
- the use of effective drugs for treatment that have a minimal range of side effects;
- an individual approach to the choice of management tactics for each patient;
- attentive attitude of the staff.
The Neurology Clinic employs candidates and doctors of medical sciences, who are leading neurologists. All complex cases of internal hydrocephalus are discussed at a meeting of the expert council. Doctors make a collective decision on the treatment tactics for a patient suffering from severe hydrocephalus.
Types and forms of internal hydrocephalus
Depending on the cause of the disease, two forms of hydrocephalus are distinguished - open, communicating and closed (occlusive). Open hydrocephalus occurs as a result of increased secretion or impaired absorption of cerebrospinal fluid. Closed hydrocephalus develops when the patency of the cerebrospinal fluid outflow tract is obstructed by a tumor, inflammatory infiltrate, or adhesions.
Internal non-occlusive hydrocephalus can be congenital or acquired. Congenital hydrocephalus occurs during intrauterine development of the fetus. Acquired hydrocephalus develops under the influence of various diseases and injuries after the birth of a child.
The acute form of hydrocephalus is characterized by the rapid onset of symptoms of the disease within 3 days. In the subacute course of the disease, the increase in signs of hydrocephalus continues up to 1 month from the onset of the disease. Chronic hydrocephalus can take anywhere from several weeks to six months to develop.
Depending on the rate of progression of the symptoms of the disease, 3 forms of internal hydrocephalus are distinguished:
- progressive or active – occurs with rapid accumulation of cerebrospinal fluid and severity of symptoms;
- stabilized or passive – signs of the disease do not increase;
- regressive - symptoms of the disease disappear without treatment.
Neurologists distinguish compensated, subcompensated and decompensated stages of hydrocephalus. Depending on the level of intracranial pressure, there are hypertensive (with increased cerebrospinal fluid pressure) and normotensive (with normal intracranial pressure) internal hydrocephalus. Internal asymmetric non-occlusive hydrocephalus is characterized by dilation of one ventricle; in the presence of symmetric hydrocephalus, both ventricles of the brain are dilated.
Classification of dropsy
Patients may experience:
- External HGM, which is characterized by the fact that cerebrospinal fluid is not absorbed into the bloodstream. And this is the big problem.
- Internal GGM. It differs in that there is an accumulation of a certain amount of cerebrospinal fluid in the subarachnoid space and the ventricles of the brain.
- Mixed GGM. It is characterized by the fact that cerebrospinal fluid accumulates not only in the cisterns and ventricles of the brain (that is, inside), but also under its membranes (that is, outside).
- Internal replacement hydrocephalus of the brain, which results in atrophy of brain tissue and its replacement with cerebrospinal fluid. It is very serious. Most often, such “metamorphoses” occur due to age-related factors. But internal replacement hydrocephalus of the brain in an adult can also be caused by other reasons (for example, alcoholism or infections).
- Closed (or occlusive) hydrocephalus. The disease occurs due to the fact that the outflow of cerebrospinal fluid is impossible due to the presence of a neoplasm, with the growth of which the situation only gets worse. Very severe form.
- Internal open hydrocephalus of the brain (or communicating HGM). There is hypersecretion of cerebrospinal fluid and a failure in the process of its absorption.
- Spicy. The disease progresses rapidly and symptoms expand.
- Subacute. The increase in symptoms occurs gradually (over 1-1.5 months).
- Chronic. The development of clearly noticeable manifestations of the disease is observed no earlier than 6-12 months after the onset of the pathology.
- Vicarious hydrocephalus. With this disease, the ventricles become enlarged. Moreover, no changes in the structure of the organ itself in terms of anatomy are observed.
- Internal asymmetric hydrocephalus of the brain. In this case, either an enlargement of one ventricle or all of them may be observed.
- Hypertensive. In this case, there is a significant increase in intracranial pressure.
- Normotensive. The size of the ventricles changes, but the pressure does not differ from normal.
On a note! External and internal hydrocephalus of the brain can be either congenital (that is, appear at the stage of intrauterine development of the fetus) or acquired (that is, appear during a person’s life).
Depending on the reasons for the impossibility of outflow of cerebrospinal fluid, the following forms of the disease are distinguished:
The form of development of the disease can be:
On a note! Moderate internal hydrocephalus of the brain is very poorly recognized, and is generally diagnosed completely randomly. Pronounced symptoms are observed when significant structural brain disorders occur, as well as a failure in the blood circulation of the main organ of the central nervous system. We shouldn't forget about this. And visit a medical facility more often in order to prevent serious pathologies and treat them. Remember: the development of moderate internal hydrocephalus of the brain in adults can lead to serious complications.
Depending on changes in the size of the ventricles, the disease is divided into:
Hydrocephalus can be:
Important! Regardless of what type of dropsy is diagnosed, remember: this is a very dangerous neurological disease that requires observation by a specialist and, if the condition worsens, immediate surgical intervention.
Causes of congenital internal hydrocephalus
Internal non-occlusive hydrocephalus of the brain develops under the influence of the following factors:
- infectious diseases of a woman during pregnancy (respiratory viral infection, mumps, herpesvirus or cytomegalovirus infections, rubella, syphilis);
- abnormalities of intrauterine development that interfere with the circulation and absorption of cerebrospinal fluid;
- brain injuries;
- inflammation of the substance and membranes of the brain (meningitis, meningoencephalitis, arachnoiditis);
- hemorrhage as a result of injuries and diseases of the cerebral vessels;
- oxygen starvation or cerebral circulatory disorders.
- intoxication with chemicals or alcohol;
- genetic defects.
Internal hydrocephalus of the brain in adults can develop in the presence of oncological tumors of the brain, which are localized in the cerebellum or brain stem, acute cerebrovascular accident (stroke), arterial hypertension, and diabetes mellitus.
Prevention of hydrocele of the brain
Observation and examination of a pregnant woman will help identify abnormalities in the development of the fetus and promptly treat the infectious disease. Women whose close relatives suffer from hydrocephalus require special attention.
Caring for the fetus will protect it from intrauterine injuries and diseases. Newborns at risk require observation by a specialist.
It is necessary to protect young children from traumatic brain injuries and protect them from neuroinfections. This will also prevent the development of the disease in adults.
Congenital hydrocephalus stops its development, but is not cured. Treatment for older children may be beneficial. It depends on the severity of the disease, timeliness and quality of treatment.
Acquired hydrocephalus of the brain in an adult is most often a complication of other diseases. This pathology is characterized by the accumulation of cerebrospinal fluid. In advanced cases, surgical intervention (bypass surgery, drainage) is required. In common parlance this disease is called dropsy of the brain.
Symptoms of internal non-occlusive hydrocephalus
The main symptom of hydrocephalus in children is an increase in the size of the head. In young children, the bones of the skull are thinned, soft, and the sutures between them diverge. A convex fontanelle stands out, which does not close for a long time. The skin on the skull is thin, shiny, and venous vessels are visible under it. Babies are lagging behind in physical and mental development, they are capricious, and cry constantly. The eyes are deep-set, looking down. Visual acuity decreases. With high intracranial pressure, nausea, vomiting occurs, and convulsions develop.
In older children, the signs of the disease worsen: irritability with attacks of aggression, lethargy, headaches, impaired memory, attention and consciousness. Coordination of movements and intelligence are impaired, learning problems appear, and mental retardation develops.
The characteristic signs of internal hydrocephalus in adults are:
- shaky, unsteady gait;
- loss of urinary control;
- memory impairment;
- headaches that are not always relieved by painkillers;
- blurred vision;
- vision deteriorates, pressure is felt on the eyes;
- nausea and vomiting.
Patients experience scattered attention and decreased concentration, and loss of thinking skills. Signs of mental disorders appear:
- emotional instability;
- attacks of aggression;
- neurasthenia;
- replacement of apathy with emotional upsurge.
Impaired motor functions appear. Impaired walking, contracture in the joints or paresis of the lower extremities develops. Patients often do not attach importance to these symptoms, mistaking them for signs of normal aging and do not consult a doctor.
Etiological reasons
With internal asymmetric hydrocephalus, the internal liquorodynamic pathways are damaged. The process of cerebrospinal fluid stagnation may involve 1 of the 4 ventricles or several at once. The cause of impaired outflow of liquorodynamic fluid is tumor processes, cystic formations, swelling of the ducts (central canal, interventricular foramina, foramen of Magendie and others).
Etiology of hydrocephalus with asymmetry in adults:
- cerebral blood flow disorders, history of strokes;
- tumor neoplasms;
- infectious and viral lesions of brain structures: meningitis, ventriculitis, brain tuberculosis;
- diabetes;
- injuries (closed, open TBI, gunshot wounds, falls from a height);
- hypoxic brain damage;
- chronic alcoholism, drug addiction.
Why does hydrocephalus occur in children? In childhood, congenital hydrocephalus with asymmetric damage to the internal liquorodynamic pathways occurs due to trauma during childbirth, cancer, and congenital intrauterine infection. Hydrocephalus in a child is provoked by inflammatory changes in the cerebral cortex and hypoxia. Also, children can develop hydrocephalic syndrome due to genetic damage that is inherited.
Tumor or cystic formations that appear in the brain compress or block the channels, openings and the horns themselves. Liquor begins to accumulate in the cavities of the ventricles, but cannot flow out of them. The pressure inside the skull begins to increase, the membranes of the brain are stretched. Over time, the cerebrospinal fluid puts pressure on the brain tissue, damaging it.
Hydrocephalic syndrome can occur in adults and children due to injury or surgery. After severe head injuries, hematomas may appear, which begin to damage the brain and ventricles. The transport of cerebrospinal fluid is disrupted. The cause of hydrocephalus can be venticulitis (inflammation of the ventricles) and meningoencephalitis (inflammation of brain tissue). Swelling of the tissues impedes the outflow of liquorodynamic fluid during inflammation.
Hydrocephalic syndrome often occurs after brain surgery. In this case, adhesive formations appear that block the ducts. The cerebrospinal fluid cannot flow normally, the pressure inside the skull increases, and brain tissue is damaged.
Internal asymmetric non-occlusive hydrocephalus develops due to excessive formation of cerebrospinal fluid and the inability to absorb it. The fluid does not have time to leave the ventricles. This condition is most often observed in children and is congenital.
Diagnosis of internal hydrocephalus
The clinical symptoms of internal hydrocephalus are usually so characteristic that they allow the neurologist at the Yusupov Hospital to suspect its presence during the first examination of the patient. To determine the type and degree of hydrocephalus, as well as to identify the pathological process that caused the disease, doctors conduct a comprehensive examination of the patient, which includes radiography of the skull, ultrasound, computed tomography or magnetic resonance imaging.
X-ray signs of hydrocephalus are thinning of the skull bones and divergence of the sutures between them; a symptom of “finger impressions” is observed on the inner surface of the cranial vault. With hydrocephalus caused by stenosis of the cerebral aqueduct, a decrease in the volume of the posterior cranial fossa is determined on radiographs of the skull. An increase in the volume of the posterior cranial fossa on craniograms is a sign of hydrocephalus in Dandy-Walker syndrome. If one of the interventricular communications is closed, the asymmetry of the skull is visible on the craniogram.
Echoencephalography (ultrasound) allows you to determine the degree of increase in intracranial pressure. In children of the first year of life, an ultrasound scan of the brain is performed through an open fontanel using ultrasonography. The most informative are tomographic diagnostic methods. They make it possible to determine the nature of hydrocephalus, identify the location of blockage of the cerebrospinal fluid tract or an existing congenital anomaly, and diagnose a neoplasm, cyst or hematoma. Monoventricular internal hydrocephalus is characterized by an increase in the volume of one ventricle of the brain.
If vascular disorders are suspected, magnetic resonance angiography is performed. For congenital hydrocephalus of infectious origin, PCR diagnostics are performed to determine the type of pathogen that caused it. Visual disturbances and the condition of the optic discs are assessed by an ophthalmologist at the Yusupov Hospital. Neurosurgeons at partner clinics decide on the need or advisability of surgical intervention.
Diagnostics
To make a diagnosis of “Internal hydrocephalus”, the following diagnostic procedures are prescribed:
- measuring head circumference with a centimeter tape;
- fundus examination;
- magnetic resonance and computed tomography;
- ultrasound examination of the skull;
- echoencephalography;
- rheoencephalography;
- Lumbar puncture.
In newborns, the presence of pathology is very easy to suspect due to the unusual, convex shape of the skull.
Treatment of internal hydrocephalus of the brain
In the case of a compensated stage of the disease, neurologists at the Yusupov Hospital carry out dynamic monitoring of patients with hydrocephalus. Sometimes doctors prescribe diuretics, drugs aimed at improving cerebral circulation, and vitamin and mineral complexes. For severe internal hydrocephalus, drug treatment is prescribed in the initial stages of the disease. For patients, intracranial pressure is reduced and the condition is alleviated with diuretics, medications are used to treat the underlying disease that caused the dropsy, and the tumor is surgically removed.
The radical method of treating internal hydrocephalus is surgical intervention. During neurosurgery, a shunt is inserted into the brain and an output tube is inserted into the abdominal or pleural cavity, atrium, or bladder to create a new drainage path for cerebrospinal fluid. In the congenital form of the disease, it is left permanently. Bypass surgery is repeated several times during the patient's life. In case of damage to the veins, the development of infectious complications, epilepsy, or the formation of hematomas, the shunt is changed. In severe cases requiring urgent reduction of intracranial pressure and drainage of fluid, external drainage is performed.
At the partner clinics of the Yusupov Hospital, neurosurgeons use the neuroendoscopic method for treating hydrocephalus. Doctors are creating new pathways for fluid drainage using a neuroendoscope with a mini-camera. Endoscopic operations have a number of advantages: they are low-traumatic, do not require the installation of a foreign body - a shunt, complications rarely develop, and the patient’s quality of life increases.
If you have signs of internal hydrocephalus, call. You will be scheduled for an appointment with a neurologist. Doctors at the Yusupov Hospital use innovative methods for treating internal non-occlusive hydrocephalus of the brain.
Source of the article: https://yusupovs.com/articles/neurology/vnutrennyaya-gidrotsefaliya-golovnogo-mozga/
Therapeutic measures
Therapy for hydrocephalus includes conservative and surgical techniques. Conservatively, doctors prescribe diuretics to reduce the amount of cerebrospinal fluid in the brain. If the patient’s cause of hydrocephalic syndrome is inflammation, then therapy is aimed at reducing the inflammatory reaction with the help of anti-inflammatory and antibacterial agents. The patient is prescribed nootropic drugs to improve brain activity, as well as antiplatelet agents and painkillers.
If conservative measures are not effective, surgical treatment is performed. Bypass operations are performed more often. The shunt helps reduce pressure inside the ventricles by ensuring normal outflow of cerebrodynamic fluid.
Types of surgical treatment:
- subcutaneous ventricular reservoir;
- plastic plumbing;
- ventriculovenous shunting;
- endoscopic ventriculostomy of the 3rd ventricle;
- venticuloatherial;
- ventriculoperitoneal shunt;
- interventriculostomy.
The tactics of surgical treatment are chosen by the neurologist depending on the type of hydrocephalus. Premedication is administered before the intervention. The operations are performed under endotracheal anesthesia.
Hydrocephalus in adults
Hydrocephalus in adults is a pathological condition that is characterized by excessive accumulation of cerebrospinal fluid in the cerebrospinal fluid spaces of the brain. Hydrocephalus can be an independent disease or a consequence of various pathological processes in the brain. Long-term hydrocephalus can lead to disability or death. Effective treatment of hydrocephalus in adults is carried out by neurologists at the Yusupov Hospital.
The neurology clinic employs candidates and doctors of medical sciences, doctors of the highest category. They examine patients with hydrocephalus using modern equipment from leading companies in the world. Doctors use individual treatment regimens with the most effective drugs registered in the Russian Federation. Neurosurgical operations are performed in partner clinics.
About cerebrospinal fluid and its functional significance
Cerebrospinal fluid is primarily produced in the choroid plexuses of the ventricles of the brain.
It fills the ventricular system and subarachnoid spaces of the brain and moves along them, constantly being renewed. Cerebrospinal fluid protects the brain, mitigating the effects of external mechanical influences, and transports nutrition for nerve tissue, hormones and biologically active substances. It also removes waste from metabolic processes in its cells, stabilizes intracranial pressure and respiratory function.
In addition, it ensures the stability of the environment surrounding the brain (homeostasis), an immunological barrier that prevents the penetration of pathogenic bacteria, viruses, tumor cells and others.
Therefore, any changes in the production, circulation and composition of the cerebrospinal fluid lead to disruptions in the functioning of the central nervous system and the occurrence of pathologies.
Excessive accumulation of fluid in the cavities of the ventricles of the brain is called internal hydrocephalus. The disease is most common among young children, especially the first year of life.
Symptoms of hydrocephalus
Hydrocephalus can be congenital or acquired. Depending on the mechanism of development, the following types of hydrocephalus in adults are distinguished:
- occlusive hydrocephalus in adults - develops due to disruption of the flow of cerebrospinal fluid due to a block of the cerebrospinal fluid pathways by a blood clot, part of a tumor or adhesion;
- open hydrocephalus - occurs due to impaired absorption into the venous system of the brain at the level of venous sinuses, pachyonic granulations, arachnoid villi, cells;
- hypersecretory hydrocephalus - develops with excessive production of cerebrospinal fluid by the choroid plexuses of the ventricles.
Open hydrocephalus is called “communicating hydrocephalus of the brain in adults.” Replacement hydrocephalus of the brain in adults is one of the types of the disease. It is accompanied by a gradual decrease in the volume of brain matter and replacement of cerebrospinal fluid.
There are internal and external hydrocephalus. Internal hydrocephalus is characterized by excessive cerebrospinal fluid content in the ventricles. External hydrocephalus is characterized by excessive content of cerebrospinal fluid in the subarachnoid space while at the same time normal levels of its content in the ventricles.
Depending on the level of intracranial pressure, hydrocephalus in adults can be:
- normotensive (cerebrospinal fluid pressure is normal);
- hypertensive (cerebrospinal fluid pressure is increased);
- hypotensive (low cerebrospinal fluid pressure).
Acute hydrocephalus develops within 3 days, chronic - from 3 weeks to 6 months or more.
Hydrocephalus in adults develops due to the following reasons:
- infectious diseases of the brain and its membranes (encephalitis, meningitis, ventriculitis);
- neoplasms of the brain stem, peri-brain structures or ventricles of the brain);
- vascular pathology of the brain (subarachnoid and intraventricular hemorrhage as a result of rupture of improper connections of arteriovenous vessels or aneurysms);
- encephalopathy (toxic, alcoholic);
- malformations of the nervous system;
- brain injuries and post-traumatic conditions.
The clinical picture depends on the period of formation of hydrocephalus, the mechanism of development and the level of cerebrospinal fluid pressure. In acute and subacute occlusive hydrocephalus, patients complain of headache, more pronounced in the morning (especially after sleep), which is accompanied by nausea and vomiting, which brings relief. There is a feeling of pressure on the eyeballs from the inside, a feeling of “sand” in the eyes and a burning sensation. The pain is bursting in nature. Redness of the sclera may occur.
If the cerebrospinal fluid pressure increases, drowsiness occurs. This is a bad prognostic sign, as it indicates an increase in symptoms and threatens loss of consciousness. Vision may deteriorate and a feeling of “fog” may appear before the eyes. In the fundus, ophthalmologists detect congestive optic discs. If the patient is not provided with medical assistance, the content of cerebrospinal fluid and intracranial pressure will increase.
Subsequently, dislocation syndrome develops, a condition that threatens the patient’s life. When the midbrain is compressed, consciousness is rapidly depressed to the point of coma, upward gaze paresis, divergent strabismus, and reflex depression develop. When compression of the medulla oblongata occurs, swallowing is impaired, the voice changes to the point of loss of consciousness, breathing and cardiac activity are inhibited.
Communicating hydrocephalus of the brain in adults often has a chronic course. The disease develops gradually, several months after exposure to the provoking factor. Initially, the sleep cycle is disrupted, drowsiness or insomnia appears. Patients' memory deteriorates, fatigue and lethargy appear. As the disease progresses, cognitive impairment worsens, leading to dementia. Patients behave inappropriately and lose the ability to self-care.
With chronic hydrocephalus in adults, walking is impaired. The gait becomes unstable and slow. Then comes difficulty in starting to move and uncertainty when standing. The patient, in a sitting or lying position, can imitate riding a bicycle or walking. In a vertical position, this ability is instantly lost. The gait becomes “magnetic”. The patient seems to be glued to the floor, and, having moved from his place, he takes shuffling small steps on widely spaced legs or marks time. Increased muscle tone is detected. In advanced cases, muscle strength decreases and paresis appears in the lower extremities. Balance disorders progress, up to the inability to sit or stand independently.
Patients with chronic hydrocephalus may urinate more frequently, especially at night. Gradually, an imperative urge to urinate begins, requiring immediate emptying. Over time, urinary incontinence develops.
Moderate external hydrocephalus in an adult can be a primary or secondary disease. It develops after a stroke, meningitis, as a result of arterial hypertension, cancer pathology, instability of the cervical spine, cerebral atherosclerosis. Moderate external hydrocephalus is often asymptomatic and leads to brain hypoxia. Patients have the following signs of external hydrocephalus:
- migraine-like headaches;
- fast fatiguability;
- nausea and vomiting;
- hearing and vision impairment.
Minor hydrocephalus manifests itself with mild symptoms.
Diagnosis and treatment of hydrocephalus
Hydrocephalus
Hydrocephalus is a progressive increase in the size of the head due to excess fluid accumulation in the cranial cavity.
The cause of hydrocephalus can be congenital malformations of the cerebrospinal fluid system, for example, a narrowing of the cerebral aqueduct that creates obstacles to the normal circulation of cerebrospinal fluid. Inflammatory processes in the meninges (meningitis, arachnoiditis) can lead to changes in their structure, the formation of adhesions and adhesions. In these processes, the main cause of hydrocephalus is the excessive formation of cerebrospinal fluid, and a decrease in its reabsorption. Hydrocephalus develops due to compression of the cerebrospinal fluid tract by brain tumors or their growth into the ventricular system of the brain.
A pathological examination of the brain reveals expansion of the ventricular cavities, thinning of the brain substance, atrophy of the choroid plexuses, compaction of the arachnoid membrane of the brain, and fusion of the meninges. The degree of changes in brain matter depends on the severity of hydrocephalus. In severe cases, the cerebral hemispheres turn into thin-walled bags filled with cerebrospinal fluid, the amount of which reaches 1-2 liters. The convolutions of the brain are flattened, the furrows are smoothed, the blood vessels are reduced and deformed. The bones of the skull are thinned, its base is flattened.
A constant clinical sign of hydrocephalus is progressive enlargement of the head.
In cases of congenital hydrocephalus, it can be detected at birth, in the first days or months of life. The skull increases in all directions, but the frontal tuberosity protrudes predominantly. The frontal region seems to overhang, as a result of which the facial skull appears smaller. Sometimes the skull is asymmetrical due to the accumulation of fluid in certain areas of the ventricular system. The sutures of the skull separate, the large fontanelle enlarges, bulges, becomes tense, and pulsates. The veins of the cranial vault dilate, the skin becomes thinner and becomes shiny. The eyeballs are usually turned downwards (a symptom of the setting sun). Possible disturbances in the movement of the eyeballs: divergent or convergent strabismus, floating movements of the main apples, nystagmus, etc. The consequence of the pressure of cerebrospinal fluid on the optic nerve is its atrophy and a progressive decrease in vision up to complete blindness. Hearing loss may occur. As hydrocephalus increases, exophthalmos (protrusion of the eyeballs), spastic paresis, paralysis, and impaired coordination of movements develop. Autonomic functions suffer: thermoregulation, sweating, water-salt metabolism, etc.
Hydrocephalus has a progressive or stationary (non-progressive) course. A stationary course is observed when pathological processes leading to hydrocephalus are compensated.
With hydrocephalus, peculiar mental changes occur. At the beginning of the disease, mechanical memory is good. Patients quickly remember poetry. Mechanical memory predominates (however, this sign is not mandatory; it is more often expressed with compensated hydrocephalus). Some children have developed musical or artistic abilities. Performance is uneven. Purposeful activity is impaired. Such children are very exhausted, have difficulty concentrating on anything, and are easily distracted. There is a tendency to mood swings, often towards euphoria (elevated, cheerful mood). Transitions from an impulsive to an inhibited state are possible; in some patients, one of these conditions predominates. During the period of decompensation of hydrocephalus, elements of uncritical behavior are observed.
Intellectual impairments in hydrocephalus range from deep idiocy to mild debility.
This largely depends on the degree of compensation for hydrocephalus, the nature of the pathological process that caused it and the degree of brain damage. With compensated hydrocephalus, the child’s intellectual development can be normal, he is able to study in a public school. With a decrease in intelligence, the child’s ability to learn depends on the degree of mental retardation. In a state of debility, children can be educated in auxiliary schools for mentally retarded children.
There are cases when an intellectually intact child with hydrocephalus is mistakenly classified as mentally retarded. The reasons for such a diagnosis may be increased exhaustion of the main nervous processes, decreased performance, and distractibility.
The listed phenomena are especially pronounced during the period of decompensation - a sharp increase in intracranial pressure. These include headache, nausea, dizziness, and impaired coordination of movements. In children with reduced intelligence with decompensated hydrocephalus, changes in behavior and academic performance occur more sharply. A teacher-defectologist should be aware of these features of the course of hydrocephalus or hydrocephalic syndrome and promptly inform a neuropathologist, neuropsychiatrist or pediatrician about this.
Preschool children with hydrocephalus may appear well developed due to good mechanical memory, reasoning, musical and artistic abilities. However, a psychological study can reveal their weak mental processes, unproductive thinking, weak logical memory, stereotyped speech, low expressiveness, and poor vocabulary. All this is important for a speech pathologist to take into account when working with children suffering from hydrocephalus or hydrocephalic-hypertensive syndrome.
As hydrocephalus progresses and brain atrophy increases, the level of mental development noticeably decreases. Memory weakens. Speech becomes poor and unemotional.
Mechanical repetition of what is heard predominates. Dementia gradually develops, aggravated by visual and hearing defects and epileptiform seizures.
For hydrocephalus, cerebrospinal fluid examination, electroencephalography, echoencephalography, skull radiography, fundus examination, angiography, pneumoencephalography, and computed tomography are performed. All this is done in order to identify the underlying pathological process that caused hydrocephalus. It is especially important to promptly diagnose progressive hydrocephalus caused by a brain tumor or an ongoing inflammatory process - arachnoiditis.
Treatment of hydrocephalus depends on the nature of the progression of the process. With a rapid increase in skull circumference, neurosurgical intervention is indicated. In cases of slow progression of hydrocephalus, it is recommended to use drugs that reduce intracranial pressure.
If there is a delay in mental and speech development, children need special speech therapy and pedagogical measures, the nature of which largely depends on the degree of intellectual defect and the severity of decompensation of hydrocephalus. In each specific case, the question of correction methods should be discussed with a doctor, taking into account the mental characteristics of patients mentioned above.
Hydrocephalus is an increase in the volume of cerebrospinal fluid in the cranial cavity.
Etiology and pathogenesis
Impaired resorption and circulation of cerebrospinal fluid or its excessive secretion. The cause is usually an adhesive process due to a previous neuroinfection or head injury, as well as brain tumors, congenital anomalies of the brain and its membranes.
Clinical picture
With hydrocephalus in newborns, the most characteristic features are an enlarged head, an emphasis on the venous network of the skull, and drooping eyes (a symptom of the setting sun); the volume of the head, gradually increasing, can reach gigantic sizes (skull circumference up to 60 cm or more).
The cranial sutures are widened, the anterior fontanel is sharply enlarged. Due to the pliability of the skull in children, symptoms of hypertension are rare.
Cranial nerve palsies are common, in particular decreased visual acuity due to atrophy of the optic nerves. Spastic disturbances are usually observed in the legs. In severe cases, mental retardation is inevitable.
Hydrocephalus in adults is characterized by signs of increased intracranial pressure: headache, vomiting, congestive optic discs, dizziness. The disease, which occurs after the age of 17-18 years, is not accompanied by an increase in head size.
Diagnostics and differential diagnostics
X-rays of the skull are changed depending on the age at which hydrocephalus developed: in adults, there is destruction of the sella turcica and increased digital impressions on the cranial vault. Computed tomography and ventriculography reveal sharply enlarged ventricles of the brain and atrophy of the medulla.
Hydrocephalus of newborns is distinguished primarily from rachitic enlargement of the head, which is characterized by the proliferation of bone tissue of the skull and skeletal changes typical of rickets.
In case of hydrocephalus in adults, it is necessary to find out the cause of the disturbance in the circulation of cerebrospinal fluid, first of all, to promptly recognize a brain tumor.
Treatment
To reduce intracranial pressure, diuretics, glucocorticoid hormones, and glycerin are prescribed. Surgical treatment of hydrocephalus in newborns consists of creating additional pathways for the outflow of cerebrospinal fluid from the cranial cavity (shunting); with hydrocephalus in adults, in most cases it is necessary to eliminate the cause of obstruction of the cerebrospinal fluid outflow tract (for example, tumor removal, dissection of adhesions).
The prognosis for hydrocephalus in newborns is unfavorable; The outcome of hydrocephalus in adults is determined by the possibility of surgical correction of the causes that caused the disease.
Hydrocephalus is a brain disease, the name of which comes from the merger of the roots of two Greek words “hydro” - water and “kephalus” - head (literally - dropsy of the brain). According to various sources, hydrocephalus is observed in 5–15 children per 1000 births. For a more detailed understanding of the development of this disease, it is necessary to have an understanding of the anatomy of the brain. Liquor, cerebrospinal fluid (CSF), is produced in the choroid plexuses of the ventricles of the brain. A person produces and absorbs about 400 ml of cerebrospinal fluid per day. Liqueur contains protein, sugar, a small amount of blood cells (lymphocytes, neutrophils), and microelements. Functionally, the fluid performs protective and hydrodynamic (maintaining intracranial pressure) functions. The ventricular system of the brain is represented by 4 cavities containing cerebrospinal fluid: two lateral ventricles, symmetrically located in the cerebral hemispheres, the third ventricle (located in the middle of the brain) and the 4th ventricle (in the area of the table of the brain and cerebellum). The ventricles are connected to each other by openings. Liquor, produced in the lateral and, partially, in the 4th ventricle, flows into the spaces under the membranes of the brain and spinal cord, where it is absorbed into the circulatory system. Normally, there is a strict correspondence between the production and absorption of cerebrospinal fluid. Hydrocephalus develops as a result of blockage of the cerebrospinal fluid pathways at various levels and when the relationship between the processes of production and absorption of CSF is disrupted.
There are congenital and acquired hydrocephalus.
Congenital hydrocephalus is a disease that develops in the fetus during pregnancy and the child is born sick. The main causes of congenital hydrocephalus are developmental defects, less often intrauterine infection, much less often the cause of hydrocephalus is hemorrhage into the ventricles of the brain in the fetus.
Acquired hydrocephalus - the disease develops after the birth of a child, sometimes in the earliest stages of life. The causes of acquired hydrocephalus are intraventricular hemorrhages, infections affecting the central nervous system (CNS) - meningitis, encephalitis, traumatic brain injury, brain tumors. The form of hydrocephalus is of primary importance for the course of the disease and its treatment. Essentially, the disease can be divided into two forms: communicating (open) and occlusive (closed).
Communicating hydrocephalus occurs as a result of a violation of the process of absorption of cerebrospinal fluid - immaturity of the system of resorption (absorption) of cerebrospinal fluid, the consequences of hemorrhages under the membranes of the brain, atrophic changes in the brain due to hypoxia (oxygen starvation), disturbances in cerebral blood flow. With communicating hydrocephalus, moderate dilation of the ventricles of the brain and expansion of the spaces between the brain and its membranes (subarachnoid spaces) develop.
Occlusive hydrocephalus is a disease that is associated with a block in the outflow of cerebrospinal fluid. Depending on the level of the cerebrospinal fluid block, monoventricular (one lateral ventricle expands), biventricular (both lateral ventricles are involved in the process), triventricular and tetraventricular hydrocephalus are distinguished. Monoventricular hydrocephalus develops when one interventricular foramen (foramen of Monro) is narrowed or blocked; with biventricular hydrocephalus, both foramina of Monro are closed. Triventricular hydrocephalus is characteristic of a block at the level of the cerebral aqueduct, tetraventricular - at the level of the exit from the 4th ventricle (the foramen of Luschka and Magendie).
Manifestations of the disease The disease can appear either from the first days of life or begin later, at any age. The severity of symptoms of hydrocephalus depends on its form, rate of progression, and characteristics of diseases complicated by cerebral hydrocephalus. The main syndrome that determines the clinical manifestations of the disease is the syndrome of increased intracranial pressure (hypertension, intracranial hypertension syndrome). Early manifestations of the disease are changes in the child’s behavior: children become restless, cry frequently and monotonously, throw their heads back, and often burp. The size of the head increases, there is an expansion of the sutures and fontanelles of the skull, bulging of the large fontanelle, tension of the saphenous veins of the head, while the size of the cerebral skull exceeds the facial skull. The so-called hydrocephalic shape of the skull is formed. Characterized by sparse hair growth. In the early stages of the development of the disease, the “setting sun” symptom (Graefe’s symptom) appears, in which the eyeballs move downward and a strip of the white membrane appears above the iris. Children, as a rule, develop with delayed mental, motor and speech development. In older children, an early symptom is headache, especially in the morning, and vomiting that is not associated with food intake. Vomiting is not accompanied by nausea, occurs at the height of the headache and brings relief.
Diagnosis. The diagnosis of hydrocephalus is established on the basis of clinical manifestations and is confirmed by neurosonography (NSG), computed tomography and magnetic resonance imaging (CT and MRI). Neurosonography: a method based on the use of ultrasound. With NSG there is no radiation exposure. The study does not require preliminary preparation or anesthesia, and can be repeated within one day. The information content of NSG in young children with open ultrasound windows (large fontanel) is very high. Computed tomography is a technique based on the use of x-rays. Highly informative examination method. The disadvantages of the method are radiation exposure and the need for anesthesia for young patients, usually up to 3 years. Magnetic resonance therapy – this technique uses a strong magnetic field. Negative effects on the body have not been described. Just like with CT, MRI in young children requires anesthesia. The fundamental difference between the MRI image is the possibility of scanning in the sagittal plane (the plane runs parallel to the longitudinal axis of the body, which allows for a detailed assessment of the third ventricle, the cerebral aqueduct, the fourth ventricle, its exits and the transition of the cerebrospinal fluid system to the spinal cerebrospinal fluid system).
Treatment After an adequate full examination, the main purpose of which is to determine the form of hydrocephalus, its severity, and assess the causes of the disease, the doctor is faced with the decision of choosing a treatment method. As a rule, open hydrocephalus is treated conservatively. The drug of choice for this disease is diacarb. Its difference from other medicinal substances that increase urine output (diuretics) and, accordingly, reduce fluid content in the body is the inhibition of cerebrospinal fluid production. The dose of diacarb is 30-50 mg/kg of the child’s weight. The maximum permissible dose of the drug 100 mg/kg body weight can be prescribed for a period of no more than 1 week. If the effect of conservative therapy is insufficient, surgical treatment is indicated for the patient. Patients with occlusive hydrocephalus in most cases require surgical intervention. Surgical intervention should be carried out in a specialized neurosurgical department. If a patient is diagnosed with a formation that obstructs the outflow of cerebrospinal fluid (a tumor or cyst of the brain), the operation should be aimed at removing it and restoring the patency of the cerebrospinal fluid tract. In cases where a cerebrospinal fluid block occurs due to a developmental defect (stenosis of the cerebral aqueduct, underdevelopment of the interventricular foramina), adhesions as a result of previous infections and brain injuries, they resort to cerebrospinal fluid shunting operations. Liquor shunt surgery is essentially prosthetics of the cerebrospinal fluid system. With such interventions, the patient is implanted with a system of drainage tubes, which is equipped with a valve to maintain a certain intracranial pressure. In this case, the outflow of cerebrospinal fluid occurs into various cavities of the body - the abdominal cavity (the most common route), the pleural cavity, and the atrium. The choice of drainage path is determined individually in each case. Disadvantages of cerebrospinal fluid shunt operations: patient dependence on the operation of the system, the need for repeated operations (statistically, up to 25% of repeated interventions during the 1st year of life), infection and rejection of systems, migration of shunt areas. In the last decade, a completely new neuroendoscopic type of surgical intervention has been developed and is being actively introduced into practice. The basis of the method is the creation of an additional hole in the cerebrospinal fluid system (usually in the bottom of the third ventricle) in order to create a bypass path for the cerebrospinal fluid outflow using special instruments. With neuroendoscopic surgery, brain trauma is minimized, the physiological processes of cerebrospinal fluid circulation are normalized and foreign bodies are not implanted. The limitation for the operation is the early age of the child - up to 6 months.
To summarize the above, we can say that hydrocephalus is a severe, progressive disease of the nervous system that requires the use of modern diagnostic equipment and specialized treatment. Currently, thanks to the development of neurology and neurosurgery, significant advances have been made in the treatment of this disease, patients with hydrocele have the chance to significantly improve their quality of life. Between 1999 and 2004. More than 100 patients with hydrocephalus were operated on in the neurosurgical department of DIB No. 5. Based on a large number of observations, we propose the following algorithm for quality standards for examination and treatment of this disease.
Table. Quality standards for examination and treatment of hydrocephalus
The term "hydrocephalus" - dropsy in the head - means excessive accumulation of cerebrospinal fluid in the cranial cavity (from the Greek "hydor" - related to water and "kephale" - head). Normally, the substance of the brain and spinal cord is constantly washed on all sides by cerebrospinal fluid - cerebrospinal fluid. It is a clear, colorless liquid that carries several functions, the main ones being additional nutrition and brain protection.
Outside the brain, cerebrospinal fluid circulates between the pia mater and the choroid over the entire surface of the cerebral hemispheres and the cerebellum. This space is called the subarachnoid space. Under the brain, at the base of the skull, there are several more places where fluid accumulates, called “cisterns.” These tanks, connecting with each other in different directions, pass into the cerebrospinal fluid subarachnoid space of the brain, and also connect with the subarachnoid space of the spinal cord, where cerebrospinal fluid washes the surface of the spinal cord from the cervical to the lumbar region.
Inside the brain, cerebrospinal fluid is located in the so-called ventricles of the brain. There are several of them: two lateral ones, located deep in the cerebral hemispheres. 3rd ventricle located in the midline. Further down, fluid passes through a thin channel in the brainstem called the aqueduct of Sylvius into the 4th ventricle, located between the brainstem and the cerebellum. This ventricle is connected by two lateral openings to the cisterns of the base of the brain and below passes into the central canal of the spinal cord, through which the cerebrospinal fluid spreads downward almost to the lumbar region.
CSF is formed during the diffusion of blood plasma through the vascular wall of capillaries in the so-called choroid plexuses, the main of which are located in the lateral ventricles (95% of CSF production) and, partially, in the 4th ventricle. The absorption of cerebrospinal fluid is carried out by the choroid of the brain, which consists of one or several layers of cells, and to a greater extent at the base of the brain and in the area of passage of large venous vessels. Being absorbed, the cerebrospinal fluid enters the circulatory system at the level of capillaries, and then veins, and, mixing with blood, is carried outside the cranial cavity. In total, a person contains about 150 ml of cerebrospinal fluid, and during the day this amount is completely renewed 3 times.
Normally, the production (formation) and resorption (absorption) of cerebrospinal fluid are in dynamic equilibrium, which makes it possible to maintain an almost constant amount of fluid at each time and, accordingly, a fairly constant level of cerebrospinal fluid pressure, which in the normal state depends on blood pressure - arterial and venous .
Excessive fluid accumulation is possible under two main conditions - when fluid circulation is impaired and when the production-resorption balance is disrupted, when, against the background of the normal amount of fluid produced, much less of it is absorbed. These two mechanisms are leading in the occurrence and development of hydrocephalus.
Violation of the circulation of cerebrospinal fluid is associated, as a rule, with the appearance of a static obstacle to the flow of fluid from the overlying parts of the brain to the underlying ones. Such an obstacle may be a large process, for example, a tumor or hematoma, scars or adhesions. The latter may be caused by head injuries, neurosurgical operations, strokes or inflammatory processes. In these cases, first of all, those parts of the liquor system that have the smallest diameter suffer. These are openings and canals connecting the ventricles of the brain to each other and to the subarachnoid space. Compression or blocking of one of the sections of the cerebrospinal fluid system causes excessive accumulation of fluid in its overlying sections. In clinical practice, such an accumulation of fluid is called occlusive hydrocephalus (from the Latin “occlusus” - locked).
The cranial cavity is a closed space strictly limited by the skeleton of the skull. Therefore, according to physical laws, an increase in the volume of fluid in this space certainly leads to an increase in intracranial pressure. The main danger of this condition is that with increasing accumulation of cerebrospinal fluid in the cranial cavity, intracranial pressure continues to increase. This is very dangerous, since compression occurs on the vital structures of the brain, primarily the brain stem, in which the main vital functions of the body are located, such as breathing, blood circulation and some others. Dysfunction of this part of the brain leads to severe, often irreversible changes. In addition, an increase in intracranial pressure, especially a rapidly developing one, leads to impaired blood circulation in the brain, which is also manifested by severe neurological loss.
Another serious consequence of increased intracranial pressure is visual disturbances. The fact is that the vascular system of the eye is directly connected to the vascular system of the brain. When intracranial pressure increases, the outflow of blood through the veins of the fundus becomes difficult. This leads to swelling of the optic discs and small hemorrhages in the retina. With long-term disc swelling, vision loss develops, which in advanced stages leads to irreversible consequences, including blindness.
Manifestations of occlusive hydrocephalus are associated with increased intracranial pressure. The main subjective symptom of this condition is a fairly characteristic headache. It occurs mainly in the morning and is often accompanied by nausea and vomiting. In advanced cases of the disease, attacks of loss of consciousness may develop, often with short-term disturbances in respiratory and cardiac activity.
The most reliable objective sign of increased intracranial pressure is the condition of the optic discs, which is determined during an ophthalmological examination. The presence of congestive optic discs in the fundus is a direct sign of increased intracranial pressure, while the above symptoms can only indirectly indicate this.
A general violation of the absorption of cerebrospinal fluid by the meninges is the cause of the development of another type of hydrocephalus, which is called aresorptive or hyporesorptive. An imbalance between the amount of fluid produced and absorbed leads to excess accumulation. This type of hydrocephalus has two different subtypes: with increased intracranial pressure - it is called hypertensive and is almost similar to occlusive hydrocephalus and without increased intracranial pressure. The last type of hydrocephalus is designated as normotensive. Manifestations of this type of hydrocephalus are associated with disorders of predominantly higher cortical functions. The American neurophysiologist and neurosurgeon Hakim formulated the main triad of symptoms of normal pressure hydrocephalus:
o mental disorders (disorders of memory, orientation, speech, etc.),
o impaired control of pelvic organ function (spontaneous urination)
o static disturbances (incorrect orientation of the body and limbs in space) and gait.
There is another type of hydrocephalus, referred to as Ex vacuo hydrocephalus, when an increase in the content of cerebrospinal fluid in the cranial cavity occurs not due to disruption of circulation or the balance of cerebrospinal fluid exchange, but due to a decrease in the volume of the brain matter. In this case, the cerebrospinal fluid occupies part of the brain volume as the latter decreases. This occurs with atrophy of the brain matter in old age or with certain diseases, such as Alzheimer's disease, chronic alcoholism, chronic intoxication, etc. In such cases, clinical manifestations are not caused by hydrocephalus, but by brain atrophy.
In the diagnosis of hydrocephalus, as in other organic brain lesions, the leading role is played by computed tomography or magnetic resonance imaging. These studies make it possible to assess the condition of the cerebral ventricles and subarachnoid intracranial spaces, their size, location and deformation, as well as the fluid content in the thickness of the medulla. Only on the basis of these studies can the presence of hydrocephalus and its type be reliably determined, which determines treatment tactics.
Treatment of hydrocephalus depends primarily on the cause of the disease.
For tumor hydrocephalus, treatment is surgical and is aimed primarily at removing the tumor.
For occlusive hydrocephalus of inflammatory or other origin and hypertensive types of aresorptive hydrocephalus, treatment is also surgical, since conservative drug treatment reduces intracranial pressure only temporarily. Surgical treatment consists of creating bypass anastomoses (shunts). When creating bypass anastomoses within the cranial cavity, artificial (silicone) tubes are used, which are installed above and below the site of occlusion (for example, ventriculocisternostomy surgery).
When cerebrospinal fluid is removed outside the cranial cavity, more complex shunt systems are installed. Of the large number of proposed ways to remove cerebrospinal fluid, the most effective are the removal of cerebrospinal fluid into the circulatory system or into the abdominal cavity. In the first case, the ventricular system of the brain connects to the right atrium of the heart, in the second, the fluid flows from the ventricles into the abdominal cavity, where, due to the properties of the peritoneum, it is completely absorbed. The complex shunt systems used are an achievement of modern neurosurgery. They consist of catheters and valves that ensure the outflow of cerebrospinal fluid from the cranial cavity in a strictly defined direction and at a strictly defined pressure.
Currently, in connection with the development of endoscopic technology, a method has emerged that allows, using an endoscope inserted into the cerebrospinal fluid system of the brain, to successfully restore the cerebrospinal fluid outflow tract. The advantage of this method is that it does not involve the implantation of artificial systems, but it is only applicable for certain types of occlusive hydrocephalus.
For normal pressure hydrocephalus, drug treatment is effective in some cases. If it is ineffective, installation of shunt systems is performed.
For Ex vacuo hydrocephalus, surgical treatment is ineffective and can often worsen the patient's condition. With this type of hydrocephalus, treatment should be aimed at treating the underlying disease.
In conclusion, it should be noted that such a common disease as hydrocephalus, although serious and in some cases dangerous, can be completely cured thanks to modern neurosurgical methods.
Information about the work “Diagnostics and treatment of hydrocephalus”
Section: Medicine, health Number of characters with spaces: 29699 Number of tables: 0 Number of images: 1
Similar works
Hydrocephalus - a syndrome of organic brain damage
22688
0
0
... quite varied. It usually appears at a time when the child’s head circumference exceeds the normal size by several centimeters. The initial signs of organic brain damage, called hydrocephalus, include spastic paraparesis of the legs with high tendon reflexes, foot clonus, and clear pathological reflexes. As hydrocephalus progresses...
Literature - Pediatrics (Book Ultrasound Methods in Neuropathology and Neurosurgery
239764
0
0
... symptoms and prophets of the development of other organs and systems. Sometimes the detection of pathology in NSG is an accidental finding. III. Systematics of B-scanning methods of the brain from the perspective of pediatric neuropathology and neurosurgery Depending on the sensors used, linear scanning or sectoral scanning is performed. Depending on the ultrasonic window used, there are ...
Emergency care in neuropathology
524428
0
0
... laryngospasm. The pain radiates to the ear and is provoked by eating and swallowing. The pain point is determined on the lateral surface of the neck, slightly above the thyroid cartilage. Giving help. Emergency care is similar to that provided to patients with trigeminal neuralgia. Glossalgia. Clinic. Glossalgia is caused by damage to the peripheral somatic formations of the oral cavity, but mainly...
Scientific and practical approach to clinical issues and diagnosis and surgical treatment of TBI
16111
0
0
... is hydrocephalus accompanied by intracranial hypertension or occurs with normal or reduced ICP. Diagnosis consists of anamnesis, neurological examination, fundus examination, diagnostic LP, EEG, CT. brain. Recently, various types of surgical treatment have been used, in combination with complex conservative treatment. With occlusive dropsy, ...
Diagnosis of hydrocephalus in adults
Doctors at the Yusupov Hospital diagnose hydrocephalus using computed tomography and magnetic resonance imaging. These methods make it possible to determine the size and shape of the ventricles, brain cisterns, and subarachnoid space. If doctors at a neurology clinic detect early signs of hydrocephalus on an MRI, they prescribe medication to stop the progression of the disease. X-ray of the cisterns at the base of the brain allows us to clarify the type of hydrocephalus and assess the direction of the cerebrospinal fluid flow.
A trial diagnostic lumbar puncture with removal of 30-50 ml of cerebrospinal fluid is carried out to diagnose the disease. After the procedure, the patient’s condition temporarily improves due to the restoration of blood supply to ischemic brain tissue against the background of a decrease in intracranial pressure. In acute hydrocephalus, lumbar puncture is not performed due to the high risk of brainstem herniation and the development of dislocation syndrome.
To clarify the diagnosis, neurologists at the Yusupov Hospital prescribe craniography, ultrasound, and angiography. The results of the examination are discussed at a meeting of the expert council, where tactics for managing a patient with hydrocephalus are developed.
How does dropsy manifest itself?
With moderate development of the process, minor neurological disorders appear. You can't ignore:
- Nausea;
- Headache;
- Vomiting;
- Deterioration of vision;
- Changes in the appearance of the eyeballs;
- Problems with the vestibular system;
- Mental abnormalities.
The open external form has manifestations similar to mental disorders. If the diagnosis is made incorrectly, the patient will be treated in a psychiatric clinic, and the underlying disease will go unnoticed. To make a correct diagnosis, the neurologist prescribes additional tests:
- MRI of the brain is clear - the results of tomographic diagnostics will show the localization of the pathology and the catalyst for the disorders (infants may be prescribed neurosonography instead of MRI);
- puncture - children are tested using general anesthesia;
- fundus examination.
At the initial stages of the development of the process, an accurate diagnosis can only be made using instrumental methods.