A young woman named Irina approached the doctor and began her story with a complaint that she was afraid to live because of oppressive hatred. The subject of this feeling was a mother suffering from dementia. She waited with horror and impatience for its end, so that she could finally live like a human being. Such situations are not uncommon. Dementia also drives the relatives of the sick person crazy. But still they find the strength to take care of him. This is what Irina said about her mother.
“One late evening my mother’s neighbor called me and asked me to urgently come to her. I immediately rushed over. Mom sat in the corridor with a knife in her hand, in some rags, with her face wrapped in a scarf, and claimed that bandits were breaking in on her. They allegedly release sleeping gas into the apartment through the keyhole in order to get inside, rob and kill her. Before this incident, I believed my mother that someone was trying to break into her house, and I even changed the locks on the front door. Now it became clear that it was time to see a doctor. The diagnosis became a death sentence: Alzheimer's. Mom was admitted to a psychiatric hospital for a long time. The antipsychotics worked, she became calmer and I took her home. But I soon noticed that my mother began to walk somehow strangely and I stopped giving them to her without consulting doctors. At first everything was fine, she went out for walks and closed the door behind her. Then she told me that she had met some friends and was going to go home with them. A week later, trouble happened again. Left alone at home, my mother suddenly began destroying everything around her in the apartment, banging on the door, screaming that she was being beaten and raped. The psychiatric team took her to the hospital. There she stopped recognizing me and claimed that I was an impostor who had kidnapped her own daughter. She demanded that her relatives be found and protected from thieves who were robbing her of money. Now my mother lives with me. He takes medications regularly, but there is no improvement. All that was left of my loving mother was the outer shell; she tormented me with frequent whims, reproaches, and began to have difficulty moving. My life has turned into a nightmare. I am afraid to go home, not knowing what awaits me there: “poisoned” food thrown out the window, cabinets emptied in search of “bandits,” a saucepan that was used as a toilet, etc. But I hold on, believing that this is my cross, my daughter’s duty. I’m just scared for my children, will they be able to bear all this if something similar happens to me?”
This fear is not groundless. Predisposition to Alzheimer's disease is inherited, so in such a situation you need to pay maximum attention to your health and consult a doctor at the first symptoms. In the early stages of dementia, its progression can be slowed down and a person's sanity can be extended for years. Progress does not stop; new drugs and treatment methods are emerging. Remember how many people died from AIDS in the 80s? And now, taking new drugs, HIV-infected people live to old age.
About the disease
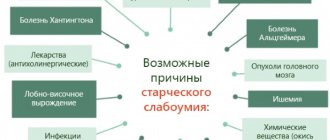
A disorder of nervous activity leading to a decrease in intellectual abilities, memory loss, and loss of self-care is diagnosed as dementia. The causes of the pathology are brain injuries, infectious and vascular diseases, Alzheimer's disease, alcoholism, and drug addiction.
People with dementia can live for many years. Life expectancy depends on the progression of the disease, which occurs individually in each patient. Death from dementia occurs at the last stage of the pathology and is more often associated with concomitant diseases.
Etiology
Alzheimer's type dementia is caused by the following etiological factors:
- hemorrhagic and ischemic stroke;
- hypertension with frequent attacks;
- vasculitis;
- atherosclerosis;
- acute heart failure;
- cerebral ischemia in a chronic form (blockage of small vessels occurs).
A hereditary predisposition cannot be ruled out either. If there is a family history of Alzheimer's disease, then there is a high probability that the same illnesses will occur in a generation at the same age.
In addition to the main etiological reasons, it is necessary to highlight a number of factors that are not the main ones, but predispose to the development of subcortical vascular dementia:
- bad habits;
- insufficient amount of physical activity;
- elderly age;
- diabetes;
- previous severe trauma or surgical intervention on the brain;
- a history of psychiatric illnesses;
- arterial hypertension.
The presence of several etiological factors significantly increases the risk of developing such a disease in old age.
Stages and symptoms
The first manifestations of dementia are difficult to notice even for an experienced doctor. Close people may note absent-mindedness, preoccupation, causeless mood swings, and indifference to their favorite hobby. Gradually, a person begins to forget current information and events, but remembers perfectly well what happened to him before. Some patients develop delusions that may arise from hallucinations. A person cannot adequately evaluate his actions; he does not notice that he has begun to behave in a different way.
As the pathology progresses, mental abilities, reading, writing, and self-care skills are lost. Conversation becomes unclear, sentences are short or broken. The patient does not understand someone else's speech well and does not respond when addressed.
The clinical picture depends on the location of the affected area of the brain, its size, and the causes of dementia. In medicine, it is customary to divide the disease into several stages. Each stage has specific symptoms that progress along with the dementia.
| Stages of dementia | Symptoms |
| Lightweight |
|
| Early |
|
| Intermediate |
|
| Heavy |
|
The last stage of dementia before death is accompanied by the following symptoms:
- The need for food decreases, the body becomes exhausted;
- The patient cannot hold his head up or sit on his own.
- There are no facial movements, the facial muscles weaken and atrophy.
- A person loses the ability to chew and swallow, resulting in paralysis.
- Coordination of movements is impaired, stupor or coma may occur with a fatal outcome.
In the last stage, dementia before death can last up to one and a half years, but usually a person dies within 6 months.
Note. Impaired swallowing function often causes food particles to enter the respiratory system, which can cause pneumonia and death.
Early stage dementia
As the process of destruction and disorganization of neurons in the brain intensifies, the disease moves into the next stage of development, and its manifestations intensify.
At the early stage of developing dementia, mental impairment increases. If you ask to read a short text and then retell it, the person will not cope with the task.
At this stage, cases of forgetfulness of recent events and disorientation in familiar areas become more frequent.
Early dementia is accompanied by:
- pronounced emotional lability (from aggression to complacency);
- the appearance of anxiety, apathy, depression;
- increasing memory impairment.
At an early stage, tearfulness and irritability may appear. The person becomes apathetic and drowsy. With vascular dementia, dizziness, attacks of uncontrollable anger, or, conversely, periods of euphoria are noted.
The character of a person also changes. Negative traits appear in him or existing ones intensify, such as stubbornness, indifference to others, fussiness, and rudeness.
Brain dysfunction at the end of the stage of early dementia manifests itself:
- loss of the ability to tell time using an analog clock;
- the appearance of problems at work (can’t remember faces, doesn’t assimilate new information, doesn’t remember where he put important documents);
- difficulties with driving a car.
As a result of the loss of work skills at the early stage of dementia, a person may lose his job, which aggravates the course of the disease and accelerates the transition to a more severe stage. Relatives of the patient at this stage of the disease can provide effective assistance.
How to help with early dementia
The task of treatment at the stage of early dementia is complicated by the fact that the patient often denies the disease. It will take a lot of patience from those around him to convince him to take medications, follow a daily routine, follow a diet, perform feasible physical exercises and train his memory.
Early dementia - stage features and solutions
To help the patient, you need to:
- Identify the cause of the disease, for which you will need to visit a psychiatrist or neurologist.
- Check ability in everyday life (ability to use gas, electrical appliances).
- Provide extended care, including cooking and cleaning the house.
- Monitor the intake of prescribed medications.
- Teach all family members how to care for the sick.
- Coordinate the actions of relatives and friends to care for the ward (draw up a schedule of medical and hygienic procedures, walks, memory training).
- Coordinate the actions of relatives and caring staff at the patient’s place of attachment (in a clinic or hospital).
A person with dementia needs emotional support
It is important to ensure the possibility of constant contact with the patient, spend more time with him, communicate more often by phone
Relatives should be able to independently assess memory loss at each stage of the disease. To do this, you can use special tests for dementia, and to slow down the process of neuron destruction, neurologists recommend performing brain exercises.
Memory training
During the stage of MCI and early dementia, thinking is improved by memory training. The patient can do the exercises on his own, but it is best if he trains his memory at home with a close relative or friend.
To improve brain activity, perform exercises:
- Learning words.
- Working with images of objects (repetition of names).
- Reading and repeating sentences and entire semantic passages.
- Solving logical problems.
- Direct and reverse counting.
Training in familiar home conditions is more comfortable than training outside the home or with strangers. An unusual environment and the presence of hospital staff can increase the level of anxiety and cause stiffness and fear in the patient. This contributes to increased disorientation in space and confusion.
Overwork, lack of adequate sleep, travel, or a change of residence can accelerate the increase in symptoms of dementia. Although new experiences are necessary to stimulate brain activity, in large quantities they can cause stress.
Dementia is a deadly disease cause
Dementia causes a number of diseases before death. An immobilized and unconscious person cannot identify the necessary needs, and often the symptoms of dangerous diseases are not noticeable by relatives.
The following diseases and conditions can accelerate death:
- Poor circulation increases the risk of blood clots, which can lead to death.
- Prolonged immobility provokes the formation of bedsores. A weakened body is not able to regenerate tissue normally. Infection of open wounds complicates the condition and leads to the development of sepsis, which in 90% of cases is fatal.
- Long-term use of antipsychotic drugs provokes intestinal obstruction, liver disease, and gastrointestinal tract disease. This is also the cause of death.
- Pneumonia. It is the most common cause of death in people with dementia. At this stage, dementia is a sign of imminent death. Stagnation of blood causes pulmonary edema (filling with fluid). The organ cannot provide the body with enough oxygen. Metabolism is disrupted and the condition of the brain worsens. The consequence is the rapid departure of a person from life.
Less commonly, people with dementia die from heart attacks and strokes. Their cause is delirium - a mental disorder and hallucinations that induce fear, excitement, and panic.
Frontal dementia
Another name for brain pathology is Pick's disease.
The disease begins at a younger age - 45-50 years, when the body is subject to hormonal changes.
The first signs appear in a sharp change in behavior. A person is capable of showing aggression where it should not be.
Dissatisfaction with oneself and life, as well as uncontrollable behavior, appears. It's difficult to control yourself. A responsible, decent and law-abiding citizen is gradually degrading, and his actions defy any logic.
It is difficult for a person to communicate with people; they lose the ability to construct sentences correctly, as well as fully express their feelings and emotions. With all this, the skills and experience are retained for quite a long time, the patient does not experience difficulties in performing the assigned tasks. Memory also does not suffer; a person can easily remember what he did last summer.
Similar symptoms are characteristic of moderate frontal dementia. A more progressive stage of the disease involves the addition of additional symptoms, such as lack of self-control, inappropriate behavior, and memory deterioration.
Life expectancy depends on the period of life at which dementia began and what triggered it. Statistics show that a person can live quite fully for 5-10 years, since the symptoms do not threaten others or himself. Then everything depends on the situation and the rate of progression of the disease.
With the help of drug therapy, it is possible to slow down degenerative processes in the brain. However, diagnosis is complicated by the scant symptoms of the early period.
A person may not even suspect that he has problems with the frontal part of the brain, and his aggression and disorders are usually associated with hormonal changes (menopause).
Thus, life prognosis and its duration depend entirely on the severity of dementia, its type and the age of the patient.
Statistics show that the most favorable prognosis and high life expectancy with the disease are those patients who saw the manifestation of the disease at a late age - after 65-70 years. The early manifestation of dementia is marked by the rapid course of the disease, as well as the lightning-fast addition of new symptoms.
Terminal state
At the last stage of the disease, the person no longer shows vital activity. He is deeply indifferent to the world around him, close people, physiological needs. This condition indicates imminent death. Quality care for a bedridden patient can delay care by several months.
Signs of death in a person with dementia:
- long suspended animation sleep;
- difficulty urinating, minimal output of dark-colored urine with a specific odor;
- lack of stool;
- coldness of the extremities associated with decreased blood circulation;
- dark spots on the skin caused by decreased metabolism and damage to soft tissues;
- constriction of the pupils.
The next stage is pre-agony - the slow death of the body. Blood pressure drops sharply, tachycardia begins, and oxygen delivery to the brain decreases.
Agony is the last outbreak of the body’s activity. During this period, the functions of the higher parts of the brain are activated, which may not have been involved in life. Sometimes people with dementia become lucid before death. This phenomenon is known to science as pre-death clearing. The case is rare, but leaves a strong impression on people caring for dementia patients. Basically, a person dies insane. The agony can last from a few minutes to an hour and is accompanied by muscle cramps, normal heart contractions and breathing rhythms. Next comes clinical and then biological death.
Many people believe that dementia is a sign of imminent death, but this is not true. With timely treatment, you can delay the process of parting with your loved one. Proper care, proper use of medications, classes to develop brain activity, and “imitation” lessons can prolong life and slow down the progression of dementia. The main goal of loved ones is not to give up and not give up.
Stage of minor cognitive impairment (MCI)
The first stage of dementia, when changes in brain function have already appeared but do not manifest clinical symptoms, is considered the stage of preclinical symptoms of MCI (Mild Cognitive Impairment).
The first manifestations of the pathology are nonspecific. The risk of MCI is indicated by the appearance of lack of initiative, narrowing of interests, and minor changes in behavior.
The nature of the first symptoms depends on the type of dementia. If the cerebral cortex is affected, as in Alzheimer's disease or frontal lobe dementia, then the first signs of cognitive disorder are manifested by mild forgetfulness and difficulty choosing words in a conversation.
In Parkinson's disease, the brain's motor neurons, which are responsible for motor activity, are destroyed. The first symptoms of dementia in Parkinson's disease appear at the MCI stage with changes in gait, trembling of fingers, and poor facial expressions.
Damage to the frontotemporal lobes of the brain causes frontotemporal degeneration, which is characterized at an early stage by deviations in the emotional sphere and inadequate assessment of the actions and intentions of others.
The initial signs of vascular dementia may include memory impairment and loss of orientation in a familiar room. For dementia with Lewy bodies, in which connections between neurons are destroyed, the appearance of slight stiffness of movements and a decrease in the speed of thinking are typical at the MCI stage.
How to help a patient
MCI – stage features and solutions
At the stage of mild cognitive impairment, a person is able to adequately assess his condition. He understands that the emerging memory problems are abnormal and is actively involved in the treatment process.
Potential interventions for the cognitive impairment stage of MCI include:
- performing physical exercises;
- walks;
- healthy sleep;
- diet;
- expanding your social circle (attending group classes, communicating with relatives and friends);
- stimulation of mental activity (solving logical problems, crosswords, playing chess).
A Mediterranean diet is beneficial for proper brain function. The diet should include whole grains, fish, nuts, fruits, fish, olive oil, avocado, seafood.
Lentils, berries, especially blueberries, cabbage (broccoli, cauliflower, Brussels sprouts), and low-fat dairy products are good for brain health. The diet is limited to red meat, fatty, salty, smoked foods.
Moderate physical activity helps maintain mental alertness into old age. Just 30 minutes a day of dancing, Nordic walking or swimming is enough to maintain active longevity.
To preserve brain function, you should protect your hearing. Disruption of the auditory analyzer changes the performance of the brain as a whole. And, of course, you need to completely give up bad habits.
An indicator of destructive changes in the brain is a deterioration in the sense of smell. Statistics show that the risk of developing dementia in old age increases 3 years after the loss of smell.
Life expectancy in the final stages of Alzheimer's disease
Alzheimer's disease is a pathology whose mechanisms aggravate the functioning of the central nervous system. Patients' intellect decreases, their psyche suffers, and their personality disintegrates. They lose their memory and ability to care for themselves, and lose the ability to sit and walk.
How many people live with Alzheimer's disease in the last stage, if it is extremely difficult? If symptoms progress slowly, patients may live a long time. The prognosis depends on how long the process of disintegration of the human psyche and personality will be.
The disease has other names: senile dementia, senile insanity, although it develops not only in older people after 50–65 years. There are known cases of early brain disease at the age of 28–40 years.
Alleged factors for the development of the disease
There are no exact descriptions of the causes of Alzheimer's disease yet. Based on research, it is known that brain tissue accumulates neurofibrillary tangles or plaques. They are the reason for the start of the atrophic process. Therefore, patients begin to forget their first and last names, periodically may not recognize relatives and friends, run away from home and do not find a place to live.
Many researchers argue that genes are associated with the disease, that is, the pathology can be inherited. It is also assumed that the disease can occur due to:
- head trauma;
- poisoning with toxic chemicals;
- excess weight and physical inactivity;
- hypertension;
- bad habits and bad ecology.
Classification: forms, stages of the disease
There are senile and presenile forms of the disease.
When confirming the senile form, it is stated that it begins late, after 65 years, and is caused by the lipoprotein ApoE - a specific protein deposit unique to this disease.
The toxic protein β-amyloid (amyloid plaques) is deposited between brain neurons. And in the cells, peculiar microstructures appear - neurofibrillary tangles. They are formed by another type of protein - tau protein.
It is assumed that the plaques disrupt neural interaction and, as a result, the functional functioning of the brain. Moreover, the cells die, and the pathological phase of the process is finally completed by neurofibrillary tangles. The development of diffuse cortical atrophy begins primarily in the area of the temples and crown, then the frontal lobes of the brain are affected.
The progression of the senile form can last from 10 to 15 – 20 years. The main symptom is increasing memory impairment.
The progression of the presenile form is rapid and develops in people aged 50–65 years, rarely in young people with a genetic predisposition. The disease is formed due to the mutation of three genes: amyloid precursor, presenilin 1 and presenilin 2.
This form is characterized by speech disorder (aphasia), visual memory (agnosia) and disability. People can live 8 to 10 years with this type of illness.
Stages of the disease
1. The first stage is pre-dementia.
Patients develop symptoms that are ignored due to age or fatigue. Namely, people:
- forget about events that happened recently;
- have trouble remembering new information;
- cannot concentrate when communicating with people;
- are unable to remember some words;
- are often apathetic.
At the first stage, a person can work, do everyday life and fully take care of himself.
2. The second stage is early dementia.
At the second stage, it is no longer possible to talk about symptoms as natural processes of aging of the body. The patient’s behavior is characterized by deviations that are noticeable to everyone around him:
- memory is upset: new information is not absorbed, there is no memory for recent events, but it is retained for distant and professional skills;
- speech is disrupted: the pace decreases and the vocabulary becomes poor;
- Fine motor skills are deteriorating: it is difficult to fasten buttons, put on clothes, and write, so the help of loved ones is required.
3. The third stage is moderate dementia.
At the third stage, cognitive functions noticeably decrease:
- when pronouncing phrases, speech gets confused, becomes meaningless, patients forget words or pronounce them incorrectly;
- reading and writing skills are lost;
- patients cannot cope with household activities, clothing, eat food and require help;
- intelligence changes for the worse, people do not recognize loved ones and cannot remember early and late events;
- a person becomes apathetic or overly emotional, whiny and aggressive, and leaves home;
- when walking is impaired, patients often fall, break limbs, especially the femoral neck, and get hit by vehicles moving on the streets;
- Symptoms of delirium and urinary incontinence appear.
Important. With moderate dementia, the disease often worsens, so patients behave extremely inappropriately. This is a good reason for admitting a “violent senile person” to a hospital. Symptomatic physiotherapy and treatment will slow down the pathological process and relieve exacerbation.
4. Stage four – severe dementia.
At the last, fourth stage, patients require full care from family and friends. The vocabulary becomes minimal, verbal skills are lost, but the person is able to perceive gestures addressed to them. They eat when fed, but lose weight.
They may have difficulty moving, then stop doing so altogether and do not get out of bed. This leads to the formation of infected bedsores and the appearance of pneumonia, influenza, and thrombosis. Patients require diapers and special wipes to absorb moisture on the bed.
With severe apathy, attacks of aggression occasionally occur, and speech is completely lost.
How long do people live with late stage Alzheimer's disease? Unfortunately, during this period, the health of patients deteriorates, the body is exhausted physically and mentally. Patients with severe dementia can live for six months or a year, but with good care much longer.
The processes occurring in the cerebral cortex are considered irreversible, and Alzheimer's disease is considered incurable.
With early detection and timely initiation of treatment, proper care can enable a sick person to live longer.
When carrying out therapy that improves hemodynamics, microcirculation and metabolic processes in the brain, pathological processes slow down, quality of life and life expectancy improve.
Diagnostics
Family members always notice that an elderly relative cannot think logically, is inattentive, is disoriented in time and space, cannot normally express his thoughts and choose words, and does not listen to anyone. If his behavior has changed: he has become aggressive or too calm and silent, it is necessary to contact a medical center and undergo a diagnosis.
If Alzheimer's disease is suspected, the following is carried out:
- computed tomography with nuclear magnetic resonance to determine the state of the brain;
- study of general and biochemical blood tests to identify blood diseases, hormonal disorders, infections, etc.;
- questionnaire tests to determine symptoms of the disease;
- eye drops to detect affected cells and give a positive or negative response.
How to prolong the life of a patient
In order to slow down the complete destruction of the personality and help the patient remain adequate for several more years, improve his life, it is necessary to treat him: give medications prescribed by the doctor, do massages and other physical procedures, and also balance the diet.
If necessary, patients are placed in a hospital for a course of psychotropic medications.
Many doctors are of the opinion that with such a severe brain disease, it is undesirable to treat patients in a hospital for a long time.
It is always better for them at home, where they can join in a useful activity that the patient is still able to carry out. Exercise stimulates the brain to work and inhibits the degeneration process.
To avoid worsening dementia, you must:
- surround the patient only with familiar people;
- do not leave alone for a long time and in the dark (you need to turn on low lighting at night);
- eliminate external stimuli, including contact with strangers;
- create a comfortable room temperature to prevent overheating and loss of fluid or hypothermia;
- exclude infectious diseases;
- give medications on time.
Important. Surgical interventions should be performed under anesthesia only in connection with vital indications in patients.
Practical advice
To cope with the situation and caring for a sick person, you need to use several recommendations:
- The patient retains his usual activities, maintains independence, but is introduced to a routine.
- The patient maintains self-esteem, prevents conflicts, and maintains a sense of humor.
- They ensure safety in the home and personal premises, remove everything that the ward may swallow: dog food, jewelry, flower bulbs, etc.
- They encourage healthy but not burdensome physical exercise and communicate more often.
- Support the patient's memory with visual aids.
- Stimulate independence when putting on clothes by laying out each item in turn.
- They teach how to brush their teeth by example, using the desire to imitate.
- They are taught to go to the toilet according to a schedule: in the morning after sleep, after eating or drinking, etc. Then patients show anxiety before the desire to relieve natural need.
- Do not bring the ward into a dark room; turn on the light in advance. Mirrors are removed so as not to cause fear in a person from the sight of their reflection.
- They bathe their children in the bath, since the water from the shower can scare them.
- The patient is served food in dishes without pictures and commands are voiced, helping him to eat food independently: “take a spoon”, “put soup or porridge into it”, etc.
Only with adequate care for patients with Alzheimer's syndrome can their lives be improved and extended. At the same time, we should not forget about our own health and psyche. It is important not to panic, not to get depressed, to get rid of daily stress by frequent walks, sports, watching an interesting movie, doing something you love or doing a hobby.
Source: https://glmozg.ru/bolezni/psihicheskie/zhizn-na-poslednej-stadii-altsgejmera.html
Diagnostics
If vascular dementia was identified at the initial stage of development, then timely treatment gives the patient a chance for a full recovery and a normal life. If the pathology has already developed, then treatment can slow down this process. For diagnosis, the doctor needs:
- Study the history of the development of dementia and the characteristics of the patient’s life.
- Monitor blood pressure regularly.
Neurologist Alexey Valerievich Alekseev tells more about the specifics of diagnosing the disease:
- Conducting psychological testing, which allows us to identify various cognitive disorders.
- Regularly take a clinical blood test and monitor your sugar levels.
- Control of cholesterol and lipid levels in the blood.
Instrumental methods for diagnosing vascular dementia include:
- Radioisotope examination of the brain.
- Magnetic resonance or computed tomography.
- Ultrasound of the brain.
Echocardiography is an ultrasound method that diagnoses morphological and functional changes in the heart and its valve apparatus
- Electroencephalogram.
- Dopplerography of cerebral vessels.
- Echocardiography.
- Angiography.
The results of the studies make it possible to identify vascular dementia and begin its treatment.