Man is a rational being, and in this he differs from animals. This determines his, if you like, human life. Exactly with the definition in the XYII century by Rene Descartes: “Cogito ergo sum.” Or, in Russian translation, “I think, therefore I exist.”
Our body is a shell for the brain, which is designed to provide the most favorable conditions for its functions, the most important of which is associated with the mind, thinking, and cognition. Cognitive, in other words, activity. How well it is able to implement its most important function depends on the state of the brain and its membrane.
From chronic fatigue to emotional burnout
Life in the modern world is a marathon of psycho-emotional overload. And also problems with physical health, a series of infections, primarily viral ones, which are not recognized. Cytomegalovirus, herpetic, adenovirus... The result is chronic fatigue syndrome. Best case scenario. Because chronic unresolved distress leads to a more severe syndrome - emotional burnout. Whether you are overcome by oppressive fatigue, emotional devastation or oversaturation, it doesn’t matter. And also memory and attention disorders, anxiety depressive disorders, aggressive reactions, outbursts of anger, decreased professional achievements with severe feelings of loss of competence and success in one’s activities. If these are all modalities of the most important (cognitive) function, what do you think of this function? It's worth thinking about.
“No matter where you throw it,” there’s disease everywhere
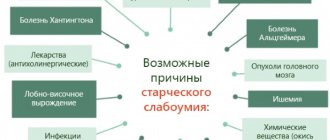
More severe, progressive cognitive impairment occurs due to diseases of the brain and the covering for the brain - our body. We are talking about somatic diseases, which are countless. The most important of them:
- atherosclerosis with damage to cerebral vessels;
- arterial hypertension, especially with disturbances in the daily periodicity of blood pressure (the so-called non dipper);
- cerebral stroke, again associated with atherosclerosis and arterial hypertension;
- diabetic antipathies.
They are followed by:
- toxic and metabolic brain damage
- post-traumatic brain damage
- Alzheimer's disease
- Parkinson's disease
- chronic heart failure
- chronic liver failure
- chronic renal failure
- chronic endocrine insufficiency
- hearing impairment; visual impairment
Development mechanism
Vascular dementia of the brain almost always refers to secondary pathological processes, that is, it is provoked by other diagnoses.
In the vast majority of cases, atherosclerosis is to blame.
Slightly less often, hypertension and a recent stroke are involved in the formation of disorders of higher nervous activity; the same phenomena are possible in chronic heart failure.
There are many culprit factors; such a variety of reasons creates some difficulties in terms of diagnosis.
Be that as it may, there is a gradual destruction of individual brain tissues. It is not avalanche-like or massive, as with a stroke, therefore changes in the nature of the central nervous system gradually deviate. Sometimes it is so slow that neither the patient nor even his relatives see the difference.
If the cause of the pathological process is an emergency condition, an acute cerebrovascular accident, then everything is immediately obvious.
The gradual death of neurons is irreversible; it is impossible to restore these tissues. However, for some time the body is able to compensate for the neurological deficit.
At a certain point, a turning point occurs in the situation; the central nervous system can no longer fully restore basic functions. The first symptoms appear.
Then the disease progresses faster because it does not meet resistance from the body, which is not able to compensate for the disorder.
The specific forms of neurological deficit depend on the location of the changes. The frontal, temporal, and parietal lobes are most often affected. Subcortical structures.
Attention:
Rarely ischemia affects only one area of the brain; this is almost impossible. Therefore, the symptoms are diffuse and multiple.
In the early stages, there is still a chance to stop the progression of dementia, prevent personality degradation, and mental breakdown. In the expressed cases, the likelihood of even partial recovery is controversial and vague.
As for neglected varieties, there is no chance of minimal correction. All that remains is to help the patient, relieve anxiety, eliminate aggression.
The mechanism of vascular dementia is always based on impaired nutrition of brain tissue, their gradual destruction, extinction of intellectual functions and more.
These diseases are congenital and acquired
Congenital ones appear at an earlier age, and acquired ones more often in adulthood. Accordingly, cognitive impairment occurs earlier in the former, and later in the latter. Focusing on progressive vascular diseases of the brain, it is important to emphasize that the vast majority of them occur in the elderly and senile age. But this age also means a variety of other somatic diseases, a decrease in physical and social activity and simply, excuse my frankness, old age.
Signs of pathology
Dementia in older people does not have one set of symptoms, as each person who develops dementia may behave differently. However, it is possible to identify some signs that will be the same for everyone. Most often, the patient experiences the following symptoms:
- Gait disturbance (lameness, body instability when walking, etc.).
- The appearance of epileptic seizures.
Neurologist Dmitry Nikolaevich Shubin tells how to recognize an epileptic seizure and how to help the patient:
- Urinary dysfunction.
- Deterioration of attention, memory and other cognitive impairment.
- Impairment of physical functions.
Also, symptoms depend on the stage of development of the pathology.
initial stage
It is difficult to identify manifestations of vascular dementia at this stage, since such symptoms can be characteristic of many diseases. Among them:
- The appearance of apathy, irritability or other neurosis-like disorders.
- Emotional instability and frequent mood swings.
- Depressive state.
Psychiatrist Mikhail Aleksandrovich Tetyushkin talks about the signs and treatment of depression:
- Inattention.
- Disorientation in space on the street or in an unfamiliar room.
- Sleep disorders (frequent nightmares, insomnia, etc.).
Middle stage
Now the symptoms are becoming clearer, and doctors can use them to diagnose vascular dementia:
- Sudden mood swings, when apathy suddenly changes into aggressive behavior.
- Memory lapses are still only short-term.
- Disturbance in home orientation.
This may be useful: What is cerebral ischemia in a newborn?
- Vestibular dysfunction or other physical disorders.
- Difficulty in communication. A person may forget the names of objects, be unable to carry on a conversation, etc.
Severe stage
At this stage, all the symptoms of vascular dementia become pronounced:
- A person cannot navigate in space.
- The occurrence of hallucinations or delusions.
- The appearance of aggression for no reason.
- Memory losses. The patient cannot say what happened a minute ago, does not recognize loved ones, etc.
- Difficulty moving or even being unable to get out of bed.
- The patient needs round-the-clock supervision by loved ones.
There are signs that are highly likely to indicate the development of pathology:
- Slight recovery of cognitive performance. Doctors have not yet been able to figure out what this might be connected with. Usually, this is preceded by mental stress. In this case, the patient’s condition may return to normal levels, but the pathology itself does not disappear and after a while, vascular dementia will begin to manifest itself again.
- A gradual development that often precludes diagnosis. In most cases, relatives admit that they noticed some changes in the patient, but they focused attention on this only when irreparable changes had occurred. After a stroke, vascular dementia develops only in 20-35% of cases.
- Surgical operations or treatment with coronary artery bypass surgery can precede the development of dementia.
Atherosclerotic encephalopathy
The reason follows from the name. Its morphological basis is predominantly superficial (granular atrophy of the cortex) foci of incomplete necrosis and small infarctions. Small and medium deep cortical-subcortical infarctions are possible. The clinical picture consists of a moderate decrease in cognitive functions, rarely reaching the level of dementia, with a predominance of moderately expressed focal disturbances of cortical functions (aphasia, alexia, agraphia, acalculia, apraxia, spatial agnosia).
Subcortical arteriosclerotic encephalopathy
This form of vascular encephalopathy is also called Binswanger disease, subacute arteriosclerotic Binswanger encephalopathy, chronic progressive subcortical encephalopathy, arteriosclerotic leukoencephalopathy.
In contrast to atherosclerotic encephalopathy, in 98% of cases its cause is long-term arterial hypertension with sharp fluctuations and disturbances in the daily periodicity of blood pressure in the absence of changes in the main arteries of the head. Other possible but rare causes are amyloid angiopathy and hereditary cerebral autosomal dominant angiopathy with subcortical infarcts and leukoencephalopathy, which manifest at a relatively young age.
The morphological basis is the defeat of small perforating arteries of the white matter with a diameter of up to 150 microns with hypertrophy, hyalinosis and sclerosis of the walls, with narrowing or complete closure of the lumen. There are signs of a combination of diffuse damage to the white matter (spongiosis, foci of incomplete necrosis, myelin disintegration, foci of encephalolysis) with small lacunar infarcts in the white matter, subcortical ganglia and pons.
The density of white matter decreases, especially around the anterior and, less commonly, posterior horns of the lateral ventricles—the phenomenon of “leukoaraosis.” Multiple small post-infarction cysts are formed after lacunar (mostly clinically silent) infarctions in the white matter and subcortical nodes. Enlargement of the ventricles of the brain is also characteristic. The clinical picture is dominated by progressive cognitive impairment, impaired walking function and pelvic disorders. In the end, dementia and complete helplessness of the patient develop.
Types of pathology
Vascular dementia is a disorder of intellectual abilities and memory of an acquired nature. The development of this condition is preceded by circulatory disorders in the brain. If its cells begin to lack oxygen and nutrients, they begin to gradually die.
There are the following types of vascular dementia:
- With an acute onset. In this case, the change in behavior occurs suddenly, usually several months after the stroke, embolism or cerebrovascular thrombosis.
- Multi-infarction (cortical) occurs gradually (usually over six months) after ischemic disorders.
- Subcortical (subcortical) dementia of vascular origin is characterized by damage to the white matter in the deep layers of the brain.
- Mixed (subcortical or cortical).
- Vascular dementia of an unspecified nature.
Multi-infarction condition
The cause of the multi-infarction condition, as well as subcortical arteriosclerotic encephalopathy, in most cases is arterial hypertension. Much less commonly, the cause is microembolization from thrombi of the left atrium (with atrial fibrillation) and disintegrating atherosclerotic plaques, as well as narrowing of the lumen of intracerebral arteries as a result of atherosclerotic stenosis, angiopathy and coagulopathy against the background of antiphospholipid syndrome, vasculitis, erythremia at a young age.
The morphological basis is multiple, predominantly lacunar, small infarctions with arteriosclerosis of vessels with a diameter of up to 500 microns in the white matter, subcortical nodes, internal capsule, and pons. The clinical picture is dominated by cognitive impairment, rarely reaching the level of dementia, pseudobulbar, subcortical, cerebellar syndromes, and transient paresis of the limbs. In subcortical arteriosclerotic encephalopathy, clinical symptoms develop gradually, and in a multi-infarction state, they develop stepwise, corresponding to microstrokes that develop sequentially over time.
Vascular dementia: how long do people live with this diagnosis?
Vascular dementia - we can say approximately how long patients with this diagnosis live. Approximately 67% of patients die within the first three years from the onset of the disease. The fact is that relatives take the “eccentricities” of an elderly relative for granted. They laugh at his changed gait, at his forgetfulness, and in general do not realize the seriousness of the disease. The patient himself, due to changes in his psyche, simply cannot adequately assess his condition and changes in behavior. Dementia is often discovered accidentally when an older person is referred to a nursing home or hospitalized for some other reason. In most cases, the brain damage is already so extensive that the disintegration of the personality cannot be stopped.
Relatives can only monitor and care for the patient. Approximately 70% of patients with dementia die from pneumonia. This disease kills quite quickly, especially in patients with weakened immune systems.
In second place in mortality are infections. In the terminal stage, a patient with dementia is immobilized and often bedsores appear on his body, which develop into trophic ulcers. Through these wounds, the body is open to all infections, fungi, and pathogenic flora, which are present even in hospital wards.
Due to immobility or poor motor activity, thrombophilia and thrombosis appear. In the case of dementia, any abnormalities in blood clotting can be fatal.
Due to the peculiarities of the diet of an immobile patient, the peristalsis of the digestive system is disrupted. The patient suffers from constipation and intestinal obstruction, which can cause a number of other diseases.
When treating with any medications, especially antipsychotics, you should expect side effects that are very difficult to stop.
There is no favorable prognosis for the treatment of dementia. The patient can live for 10–15 years, but it is impossible to completely recover from this disease.
Carolina Korableva
About the author: Hello! I am Karolina Korableva. I live in the Moscow region, in the city of Odintsovo. I love life and people. I try to be realistic and optimistic in life. What I value in people is their ability to behave. I am interested in psychology, in particular conflictology. Graduated from RGSU, Faculty of Occupational Psychology and Special Psychology.
The importance of localization of vascular lesions
The clinical picture is determined not only by the form, but also by the localization of vascular lesions. One of the most striking it turns out to be with vertebrobasilar insufficiency. The causes of vertebrobasilar insufficiency include atherosclerotic stenosis, deformation, congenital hypoplasia of the vertebral arteries, their compression along the path in the bone canal, etc.
Characteristic signs of vertebrobasilar insufficiency:
- frequent paroxysmal dizziness, accompanied by nausea and sometimes vomiting;
- unsteadiness of gait;
- occipital headaches;
- hearing loss, tinnitus;
- decreased memory for current events;
- attacks of “foggy” vision, the appearance of “spots”, “zigzags” in the field of vision;
- sudden falls against the background of preserved consciousness (“drop attacks”).
In old age, the most common is cochleovestibular syndrome with dizziness, unsteadiness, hearing loss, tinnitus and decreased memory for current events. Please note that any vascular lesions lead to cognitive impairment.
If you experience these symptoms, we recommend making an appointment with your doctor. Timely consultation will prevent negative consequences for your health. Phone number for appointment
Causes and essence of the disease
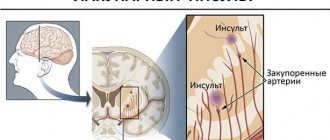
Vascular dementia develops due to disruption or cessation of blood circulation in one of the brain areas, as a result of which some brain cells die. The rate of progression of the process and the severity of symptoms will depend on how quickly the provoking factor acts.
Acute development of pathology is observed with stroke, ischemic or hemorrhagic. In the case of an ischemic stroke, a blood line is blocked by a thrombus. Its hemorrhagic form is characterized by rupture of the vessel. Both phenomena interfere with blood supply, which leads to irreversible death of cells in the brain area.
Typically, vascular dementia occurs in 25% of stroke patients. This happens if 50 ml of brain tissue is affected. The area and affected area play a big role. However, there are particularly sensitive areas of the brain, where even the slightest destruction entails disastrous consequences. These are, for example, the frontal lobes, visual hillocks.
For patients with vascular dementia, there is such a pattern: the first symptoms can appear either immediately after a stroke, or delayed, within six months. A period of 6 months is an indicative sign of vascular dementia. Typically, a stroke, especially a hemorrhagic one, leads to a rapid development of events, the appearance and increase of symptoms.
In a chronic destructive process, when small vessels are damaged, brain cell atrophy occurs gradually. Its compensatory mechanisms are activated, and symptoms increase gradually. The first signs are difficult to identify. Sometimes they hide not only from others, but also from the patient himself.
The main provoking factor that causes disruption of the patency and integrity of the blood network in the brain is atherosclerosis, that is, the deposition of sclerotic plaques on the vascular walls. Other reasons include:
- heart disease, cardiovascular failure;
- arterial hypertension;
- arterial hypotension;
- vasculitis – inflammation of the vessel wall;
- diabetes;
- hyperlipidemia;
- lack of estrogen;
- bad habits;
- excess body weight.
To... "nearby"
It is impossible to embrace the immensity. Therefore, in order to better understand the essence of brain dysfunction in the whole variety of somatic diseases, we will focus our attention on cerebrovascular insufficiency (dyscirculatory, vascular encephalopathy, angioencephalopathy).
At its core, as can be seen from the definition, is a progressive deterioration in the blood supply to the brain. Clinical symptoms of cerebrovascular insufficiency look like this:
- increase in cognitive impairment: decrease in memory, attention, intelligence with outcome in dementia;
- emotional impoverishment, loss of interest in life and narrowing of interests;
- static disturbances, destabilization of tempo, rhythm and coordination of movements, increased tendency to fall;
- development of a shuffling, mincing gait with small steps, up to the loss of the ability to walk;
- subcortical parkinson-like syndrome, in some cases with slowness of movements, poor facial expressions and a slight increase in tone of the extrapyramidal type;
- pseudobulbar disorders of varying severity with dysarthria, dysphagia, violent laughter and crying, positive symptoms of oral automatism;
- sometimes mild and moderate paresis of the limbs;
- gradual development of disorders of control over the function of the pelvic organs;
- social maladaptation, narrowing of the circle of interests and spontaneity in old age.
It is based on cognitive impairment that cerebrovascular insufficiency is divided into the following three stages or degrees of severity:
- decreased working memory, increased mental fatigue, frequent headaches, irritability, moderate disturbances of mnestic activity, decreased performance while maintaining social and everyday activity;
- worsening memory impairment with a decrease in attention and performance, an increase in intellectual and emotional disorders, the possible appearance of mild subcortical and pseudo-subcortical disorders, gait disturbances;
- dementia of varying degrees with social maladaptation and personality degradation, pseudo-bulbar and subcortical disorders, gait disorders, pelvic disorders.
Did you notice?! In cerebrovascular insufficiency, cognitive impairment is the “head of everything.” And yet, dementia is just a stone’s throw away.
How is vascular dementia confirmed?
Vascular dementia is accompanied by a decrease in the functions of the brain centers compared to the initial level, before the development of the disease, which leads to disruption of activity in communication and daily activities. In this case, deviations should not be associated with specific somatic problems and neurological deficits.
To establish a diagnosis of vascular dementia, it is necessary to take into account clinical symptoms, anamnesis, examination results, and the nature of the development of the disease. Its mandatory criteria are:
- cognitive impairment (memory disorder, lack of purpose, ability to abstract, plan);
- instrumentally confirmed fact of cerebral circulation pathology using CT, MRI and deviations in neurological status.
When examined by a neurologist, the following should be present or indicated in the medical history:
- paresis of half the body;
- decreased tone of the lower facial muscles;
- positive Babinski sign;
- impaired skin sensitivity;
- symptoms of damage to the extrapyramidal zone (if there is a lesion in it);
- inability to maintain balance, changes in gait;
- dysarthria.
Additional (secondary) signs of vascular dementia are:
- isolated cases of impaired range of active movements, coordination, asymmetry of reflexes, and other signs of pyramidal insufficiency;
- ataxia and other abnormalities while walking;
- history of frequent falls due to postural instability;
- changes in frequency of urination, urge without the presence of urological pathology;
- speech and swallowing disorders;
- depression, emotional instability, lethargy.
To clarify the diagnosis of vascular dementia, a person is consulted by a neurologist, cardiologist and psychiatrist. Sometimes communication with other specialists is required. It is important to differentiate it from Alzheimer's disease, which is accompanied by similar clinical symptoms. To do this, you need to pay attention to objective analysis data. The following signs should be considered in favor of a vascular origin:
- began acutely;
- accompanied by transient disturbances of cerebral blood flow;
- transient neurological disorders or short-term stupefaction were observed;
- the dementia clinic began in stages;
- the strength and severity of symptoms changed over a short period of time.
If there are also signs of local damage during brain examination, vascular disease and focal neurological symptoms, then it can almost certainly be stated that the patient has vascular dementia.
You should not make a diagnosis yourself, much less give potent drugs. Only a specialist with extensive experience, based on the studies performed, can determine vascular dementia.
Dementia as it is
Dementia (translated as feeble-mindedness) is understood as severe impairment of cognitive functions with a sharp decrease in memory, intelligence and the ability to abstract thinking, emotional impoverishment, personal degradation, reduction or collapse of professional, social and everyday activities. Dementia can be global or focal.
Global dementia is a disorder of all types of mental activity with loss of criticality and personality degradation. Focal dementia - preservation of personality and criticality, but a decrease in intellectual abilities and memory.
Main signs of dementia:
impairment of short-term and long-term memory;
presence of at least one of the following signs:
- violation of abstract thinking - inability to find similarities and differences between similar words, difficulties in defining words, concepts, misunderstanding of the meaning of proverbs and sayings, inability to solve simple semantic and arithmetic problems, etc.;
- violation of higher cortical functions - aphasia, apraxia, agnosia, constructive-spatial apraktoagnosia;
- impaired judgment - inability to make a purposeful plan, contact with other people, family;
- personal changes - changes or sharpening of premorbid traits, neglect of appearance, apathy, narrowing of interests;
- difficulty in normal social life and inability to work.
Levels of dementia and social activity:
- easy - maintaining the ability to live independently;
- moderate - some degree of care required;
- severe - the patient is completely helpless in everyday life.
Important note: dementia is diagnosed only when there is a combination of intellectual-mnestic disorders and signs of decline or collapse in professional, social and everyday activities. Take note, dementia is not all lost. Especially when we diagnose it in a timely manner. Simply because “he who diagnoses cures.”
Vascular dementia - symptoms and treatment
According to the International Classification of Diseases, 10th revision (ICD-10), there are the following types of vascular dementia:
- Acutely developed dementia. When a heart attack or hemorrhage is localized in a functionally significant area.
- Multi-infarct dementia.
- Subcortical dementia. The most characteristic of subcortical arteriosclerotic encephalopathy is Binswanger's disease (progressive damage to the white matter of the brain).
- Mixed subcortical-cortical dementia.
- Other forms of dementia, including dementia with hemorrhage, with global ischemia resulting from severe hypotension or cardiac arrest.
- Vascular dementia, unspecified [6].
Stages of development of vascular dementia:
Stage 1. There are no cognitive impairments. There is no apparent memory deficit on clinical interview, but very mild cognitive impairment develops.
Stage 2. Subjective complaints of memory loss arise, most often expressed as follows:
- Patients forget where they leave familiar objects.
- They forget the names of acquaintances whom they knew well in the past. However, there is no evidence of memory deficit at the clinical interview. There are no objective violations of social and professional adaptation. Criticism of one's condition is preserved.
3. stage. It is possible to see obvious cognitive impairment. Manifestations are observed in more than one of the following areas:
- The patient may get lost when traveling to an unfamiliar place.
- the patient may read a passage or book and remember nothing of what he read.
- The patient may show decreased ability to remember names after meeting new people.
- The patient may have lost or is losing motivation to perform activities.
- Concentration deficits will be noticeable on clinical testing. Objective evidence of memory deficits can only be obtained through intensive interviews. Decreased productivity at work and in social settings. Criticism of one’s condition begins to decline.
Stage 4. Accompanied by symptoms of mild cognitive decline (mild dementia): clear deficits on a thorough clinical interview that are evident in the following areas:
- Decreased knowledge of current and recent events.
- Deterioration of memory of one's past.
- Lack of concentration that occurs when reading text sequentially.
- Decreased ability to travel, manage finances, etc.
At the same time, there may not be a shortage in the following areas:
- Orientation in time and place.
- Recognizing familiar faces.
- Opportunity to travel to familiar places.
Patients at this stage are unable to perform complex tasks. Lack of criticism of one's condition is the dominant psychological defense mechanism for patients with vascular dementia.
Stage 5. Moderately severe cognitive impairment (moderate dementia): the patient already needs help for everyday life. The patient is unable, during a clinical interview, to recall any important aspect of his current life, such as an address or telephone number that he has known for many years, the names of close family members (for example, grandchildren), or the name of the school or college from which he graduated. There is often some disturbance in time orientation (date, day of the week, season, etc.).
An educated person may have difficulties with the “Counting according to Kraepelin” test (it is proposed to subtract 7 from 100 in sequence). But patients at this stage still retain knowledge of many important facts about themselves and others. They always know their names and, as a rule, the names of their spouses and children. They do not need assistance with grooming or nutrition, but may have some difficulty choosing appropriate clothing.
Stage 6. Severe cognitive decline (moderately severe dementia): Sometimes a patient at this stage may forget the name of the spouse on whom he is completely dependent as a caregiver. Patients, as a rule, do not remember many recent events and experiences in their lives. They retain some knowledge about their past life, but it is very superficial. Typically, patients do not know their exact location, year, season, etc. There may be difficulties in counting prime numbers up to 10 and back. Some assistance is required with activities of daily living. The daily rhythm is often disrupted. Patients almost always remember their name. They are often still able to differentiate between familiar and unfamiliar people in their environment.
Personal and emotional changes occur. These changes are quite varied and include:
- Psychotic symptoms. For example, patients may complain about a spouse who is allegedly an impostor, talk to imaginary figures, or refer to their own reflection in the mirror.
- Obsessive, repetitive actions.
- Symptoms of anxiety, agitation, and even previously unusual aggressive behavior may occur.
- Decreased volitional sphere. A person cannot think long enough to make a purposeful decision to take an action.
Stage 7. Very severe cognitive decline (severe dementia): all verbal abilities are lost. Often there is no speech at all, only incomprehensible statements and the rare appearance of seemingly forgotten words and phrases (incoherent thinking). Patients require assistance with personal care and feeding. Basic psychomotor skills, such as the ability to walk, are lost as this stage progresses. The brain can no longer tell the body what to do. An increase in muscle tone is often present and pathological neurological reflexes develop, for example the Babinski reflex (pathological extension of the big toe when the edge of the sole is irritated)[10].
Vascular and atrophic dementia
Brain lesions, it was agreed, may have a vascular origin, or may be associated with a pathological process in the brain itself, as, for example, in Alzheimer's disease. Therefore, the entire variety of lesions, which often intersect in everyday life, are conventionally classified into vascular and atrophic. As if vascular lesions do not lead to atrophic changes in the brain. In accordance with this, dementia is also classified into vascular and atrophic. Differentiation is carried out using the Khachinsky scale.
To do this, the patient is determined for signs of dementia and the total number of points is calculated in accordance with the scale. The criterion for atrophic dementia is the sum of points does not exceed 4, vascular - more than 7. The scale is a scale, but vascular dementia, like atrophic dementia, must also be confirmed by computer X-ray (CT) or magnetic resonance imaging (MRI).
Causes of vascular dementia
Before starting treatment for a disease, it is necessary to understand the causes and mechanism of its origin. Vascular dementia occurs as a result of the death of cells in the central nervous system, as they no longer receive nutrients and oxygen. Violation of the blood supply to a certain area is caused by acute and chronic processes, most often the cause is:
- stroke;
- cerebral infarction;
- traumatic brain injury;
- internal intoxication;
- dismetabolic processes;
- brain tumors;
- vasculitis;
- atherosclerosis of cerebral vessels;
- heart disease;
- abnormalities in the structure of arterial walls.
Hemorrhagic stroke, which provokes the appearance of vascular dementia, occurs as a result of hypertension, acute intoxication, and inflammation. Blood pours out from the affected wall and permeates the brain tissue. This process occurs quickly and is accompanied by severe symptoms. If cell death occurs simultaneously, the result is vascular dementia with typical intellectual impairments.
Heredity also plays a role. The likelihood of developing vascular dementia is higher in people whose close relatives suffer from atherosclerosis, coronary artery disease and other pathologies that cause impaired blood flow. It has already been proven that the tendency to lipid metabolism disorders with the formation of sclerotic plaques and coronary heart disease are transmitted genetically. If there are also a number of predisposing factors to the development of vascular dementia:
- alcoholism, smoking, drug use;
- low physical activity;
- diabetes;
- history of mental disorders.
As practice shows, the disease is often multifactorial in origin. Many patients at the time of its manifestation or in history have bad habits, a sedentary lifestyle, and the deposition of atherosclerotic plaques on the inner walls of the arteries.
The scourge of the elderly
Dementia is the scourge of the elderly. After 55 years, its incidence reaches 8%, and after 80 years - already 45%. The main causes of it at this age: Alzheimer's disease, dementia with Lewy bodies, vascular dementia. I would like to note on my own behalf that even if Alzheimer’s disease and dementia with Lewy bodies are present, it must be against the background of atherosclerotic encephalopathy. Simply because by this age, atherosclerosis cannot be avoided, for sure, by no one.
Alzheimer's disease is based on the accumulation of insoluble pathological amyloid in the brain parenchyma and perivascular spaces with a neurotoxic effect, the final result of which is the death of brain neurons. The most pronounced degenerative changes are determined in the mediobasal regions of the frontal lobes, the hippocampus, and the association zones of the temporal and parietal lobes of the brain. Dementia with Lewy bodies is genetically, neurochemically and pathomorphologically almost Alzheimer's disease. It is distinguished only by the presence of symptoms of parkinsonism and the early development of neuropsychiatric disorders with repeated visual hallucinations. Diagnosis of Alzheimer's disease and dementia with Lewy bodies, as well as vascular encephalopathies, is based on confirmation of dementia with verification by tomographic methods of the absence of signs of focal brain damage.
Caring for people with dementia is associated with significant financial costs. It places a heavy social, economic and emotional burden on both the patient and society. And the earlier it is diagnosed and more effectively treated, the less this burden.
Treatment
The therapy is complex, medicinal. A large group of drugs is used.
- Cerebrovascular. Allows you to restore normal blood flow in the brain. As far as this is possible without radically affecting the root cause. Piracetam, Actovegin (has another useful property - it reduces the need for oxygen in nervous tissues).
- Nootropics. Accelerate metabolic processes in the central nervous system, slow down the progression of the disease. The main one is Glycine. It is possible to use Phenibut.
- Antiplatelet agents as needed. To prevent blood clots and stroke. Aspirin-based products (Thrombo Ass, others), Clopidogrel and others. Less often, more powerful variations belonging to a different pharmacological group are prescribed. Heparin-based anticoagulants. It is possible to use Pentoxifylline for the same purposes.
- Statins. As part of eliminating excess cholesterol. Atoris, Atorvastatin.
- Antihypertensive. If high blood pressure is present. There are many names and types. Assigned according to the situation.
- Neuroleptics, tranquilizers. As behavior correctors at irreversible, pronounced stages. Aminazine, Diazepam and others.
Drug therapy is not always advisable in isolation from surgical treatment. For example, in cases of severe atherosclerosis, plaque calcification, congenital and acquired vascular defects, and some other situations, radical intervention cannot be avoided.
The best solution would be a combination of surgical techniques and medications. The task is more than creative; it requires a highly qualified doctor.
Giving up bad habits: smoking, drinking alcohol will be a great help in the future. Therefore, you should not neglect non-medicinal methods.
Treatment of vascular dementia is carried out on an outpatient basis (at home).
Treat the patient, not the disease
This advice was given to us by the father of medicine, Hippocrates, so we don’t do anything differently. In recommendations to the patient and medical interventions, the first ones are always measures to harmonize lifestyle with a possible increase in physical activity, planning work and rest, giving up bad habits, and a diet balanced in terms of quality and caloric content of food products. In particular, with regard to restrictions on table salt, refined carbohydrates and animal fats. An important place belongs to sanatorium-resort treatment. Statins are recommended for patients with atherosclerosis. For arterial hypertension, angiotensin-converting enzyme inhibitors, beta-adrenergic receptor blockers, retard forms of calcium channel blockers, diuretics, and other drugs are prescribed. In case of atherosclerosis, it is important to achieve the recommended levels of blood lipids, and in case of arterial hypertension, normal blood pressure numbers with the restoration of its daily frequency. At a high risk of thromboembolic complications (atrial fibrillation, etc.), acetylsalicylic acid, thienopyridines, low molecular weight dextrans and anticoagulants are used.
For vascular encephalopathy and Alzheimer's disease, this therapy is supplemented with antioxidants, choline alfascerate - a donor for the biosynthesis of acetylcholine in the presynaptic membranes of cholinergic neurons involved in cognitive functions, analogues of the ACTH fragment without hormonal properties, but with a neuroprotective effect, and other drugs that improve cerebral circulation.
If vascular disorders are based on anatomical causes associated with atherosclerotic plaque, stenosis, or other formations, surgical interventions are recommended. However, medical interventions are not limited to this. Because the most important thing is not said - the indispensable need, if not restoration, then improvement of the cognitive functions of the brain. Whenever cognitive impairment is diagnosed, nootropic drugs (nootropics) are used. Nootropics increase the energy metabolism of the brain, have neurotrophic, neuroprotective and neurotransmitter effects, improve memory, attention and learning ability.
The multicomponent action of these drugs, which regulate many metabolic, neurotransmitter and other changes in the body, expands compensatory capabilities and increases the brain’s resistance to harmful influences. Recently, new generations of drugs with combined nootropic, vasoactive, polyneurotransmitter, neuroprotective, antioxidant and other positive effects have appeared on the pharmaceutical market. With their use, it is possible to achieve not only an improvement in cognitive functions, but also a significant increase in the duration and quality of life of patients.
These drugs are especially indicated for transient ischemic attacks, for prevention and in the recovery period after acute cerebrovascular accident, cerebral stroke, and in all cases of diabetic angioencephalopathy. They are used for toxic, post-traumatic, post-radiation, dysmetabolic and other forms of encephalopathies.
They are indicated for Parkinson's disease, all forms of dementia, migraine, vestibular disorders, hearing impairment of vascular origin, ischemic damage to the optic nerve, and many other similar conditions. They are used to correct mental retardation in children and to enhance mental activity in old age.
Such drugs with combined nootropic, vasoactive and other positive effects are used for urgent and planned inpatient and outpatient therapy in pediatric, adult and geriatric clinics. Equally, neurological, psychiatric and therapeutic. They, and this is important to remember, are excellent helpers for chronic fatigue syndromes and emotional burnout, in general in all cases of mental stress, when there is a need to improve memory, attention and concentration.
Diagnostics
The examination is carried out by a neurologist. If there is such a need, consultation with a vascular surgeon is indicated.
The events are always approximately the same:
- Collection of clinical data. Health complaints. To understand what symptomatic complex the specialist is dealing with.
- Anamnesis collection. The moment of development of the disease (as assumed by the patient or his relatives), previous deviations, current diagnoses.
An assessment of family history of diseases, bad habits, and lifestyle may also be required. All this is important for drawing up a complete picture, a portrait of the patient, and determining the vector of subsequent diagnosis.
- Measurement of blood pressure and heart rate.
- Dopplerography and duplex scanning of the vessels of the neck and brain. Necessary technique. Aimed at identifying the speed and quality of blood flow. Shows the smallest functional deviations.
- Electrocardiography and ECHO-CG. Methods for examining the heart.
- Blood analysis. General. And also biochemical with an expanded assessment of the lipid profile. Cholesterol, atherogenic index. Suitable for detecting atherosclerosis.
- If necessary, an MRI of the brain is prescribed. It shows changes in statics. That is, the structure itself.
These methods provide information about the condition of the main organs and systems. As necessary, doctors prescribe additional techniques.
Most important function
The most important human function is cognitive. It is not for nothing that he is called Homo sapiens - a reasonable person. This function tends to be developed, maintained and, of course, restored in a timely manner or, at least, improved if it is not possible to restore completely. The only correct approach here is a systematic approach, in which drugs with nootropic, vasoactive, polyneurotransmitter, neuroprotective, and antioxidant effects are required. It is especially pleasant when the entire range of these effects can be achieved by taking one drug, and not a whole mountain of tablets. And not only in illness, but, when necessary, in health too.
Help from a psychologist for vascular dementia
Help from a psychologist for vascular dementia is a necessary component of effective therapy. Our specialists also work with people who are forced to care for such patients, as they are constantly under adverse influences and experience distress.
There is no such practice in public hospitals, since most often elderly people who have no social significance suffer from dementia. Therefore, municipal institutions are designed primarily to maintain the vital functions of the patient’s body and care, which also leaves much to be desired.
Scientists have proven in numerous studies that in the early stages of the disease, working with a psychologist can effectively maintain a satisfactory state. Typically, the following psychotherapy techniques are best suited for this purpose:
- cognitive-behavioural;
- interpersonal;
- analytical;
- psychodynamic.
Such assistance for vascular dementia is necessary for quality treatment. Many people with this disease are capable of active communication with a specialist at an early stage; they want to preserve their identity and understand what is happening to them. Supportive conversations allow them to adapt to their condition and accept it without unnecessary fear and anxiety, which further aggravate the situation. Some experts consider it inappropriate to inform a person about the diagnosis. But according to surveys and studies, most patients would like to have a more complete understanding of their problem and how to solve it.
The use of supportive psychotherapy, as practice shows, has a very positive effect on the quality of life of a person with vascular dementia. Essentially, this technique involves the psychologist providing attention, support and encouragement to the patient. At the same time, methods are used to stimulate brain function and normalize emotional manifestations. The specialist gives advice, convinces, encourages, and, if necessary, retrains the person. The emphasis of the work is on caring and understanding rather than suppression. After proper psychotherapy, you can get the following results:
- partial restoration of lost skills and functions;
- social and psychological adaptation of the patient;
- restoration of the ability to cope with difficulties;
- increasing self-esteem and self-confidence;
- knowledge of who to turn to for help in difficult times.
Psychological assistance is also necessary for the patient’s relatives who are nearby and care for him. A psychotherapist and psychiatrist explain the nature of the disease and provide basic knowledge about it, so as not to confuse manifestations of bad character with pathological disorders. Many find it difficult to come to terms with the fact that their mother, father, grandmother or grandfather becomes capricious, aggressive, and begins to say unpleasant things to them. The doctor’s task is to help survive such stress and give strength for care and optimal communication with the patient.
To prevent a nervous breakdown, the patient’s relatives need to:
- alternate between caring for a loved one and proper rest;
- periodically change the environment (mind your own business, go out into nature, communicate with friends);
- learn to completely switch your attention from the patient’s problems to positive things (communication with other family members, watching entertaining TV shows, reading books, physical exercise).
The behavior of loved ones is very important for a person with vascular dementia; the duration of the patient’s active life depends on their attitude. Psychological assistance from relatives includes the following:
- constantly explain and give advice;
- empathize and sympathize;
- encourage, teach, give incentive to action;
- constantly praise;
- increase the patient's self-esteem;
- inspire positive thoughts and hope for recovery;
- help solve problems;
- create a friendly atmosphere in the house.
It is important that relatives of a patient suffering from vascular dementia treat him with understanding. They should see a person in front of them, not a problem. If this principle is followed, then such an attitude will help him strengthen his strength, improve his skills and overcome difficulties, which, in turn, will make the task of his loved ones easier.