Definition and Features
It is necessary to distinguish between true dizziness, in which there is a feeling of objects moving in space. Such symptoms may be normal if they occur after prolonged rotation around its axis (on a carousel), but in other cases they indicate a malfunction of the vestibular apparatus. The difficulty in diagnosing this condition is that the doctor has to rely only on the patient’s testimony. Many people also mean other symptoms by this term: impaired visual acuity, headaches and others. In reality, dizziness should be understood as a feeling of movement of environmental objects in relation to a person, while the body position is felt as stable. Most often these are circular movements (objects rotate around a person’s axis), but they can also be linear (a feeling of falling or rising in height, various shocks).
Anatomy and mechanism of development of pathology
With dizziness, there is a growing lack of coordination of movements and balance. To find out its cause, one must understand how the transmission of nerve impulses that play a role in proprioception occurs. This term refers to a person’s ability to identify and sense the position of parts of his own body relative to each other and objects in the environment. Information is perceived by proprioceptor organs, including muscle tissue, and then moves along peripheral nerves to the spinal cord, from where it enters the brain. The necessary picture is formed in the parietal lobe of the brain after nerve impulses pass through the thalamus.
The inner ear is an organ that is responsible for a person's ability to maintain balance. It has a complex structure and consists of several sections: the vestibule, 3 semicircular canals and the cochlea. The inner ear is protected by bone tissue that forms the temporal lobe of the skull. It is filled with aqueous fluid - it moves when a person tilts and turns his head, and this information is perceived by sensitive cells to identify the position of the body in space.
The nervous system collects information that comes from the visual apparatus, tactile receptors and other sensory organs, as well as from the inner ear, and then analyzes it. The center of balance is located in the cerebral cortex, namely in its temporal region. Along the nerves, impulses reach the vestibular nuclei - clusters of nerve cells capable of perceiving, analyzing and coordinating information received from different areas.
Dizziness is a disturbance in the sense of balance. Anatomically, it can occur at several levels:
- peripheral - in case of disturbance of impulse conduction at the level of the vestibular nerve or inner ear (organ of balance);
- intermediate - the pathological process is localized at the stage of transmitting information from the inner ear to the central nervous system;
- central - associated with diseases of the brain, in which it is unable to analyze the information received.
Clinical signs of dizziness of different origins do not differ. The patient experiences a feeling of disorientation in space and abnormal movement of environmental objects. However, short-term loss of balance cannot be a consequence of serious diseases of the cerebral cortex. Such dizziness is accompanied by a number of additional symptoms and occurs after injury or certain diseases. To diagnose the cause and mechanism of development of this symptom, doctors at the Clinical Institute of the Brain carry out a comprehensive examination to determine accompanying symptoms.
Forms of dizziness
To more accurately determine the cause of dizziness, there are several classifications of this symptom. This distribution is necessary to understand the danger of the disease and to prescribe an effective treatment regimen. Various types of therapy can be carried out by doctors of different specialties. Thus, the first classification distinguishes two types of dizziness: systemic and non-systemic.
- Systemic dizziness is a more dangerous type, which in any case indicates pathology. It is associated with a violation of nerve conduction at the level of the vestibular apparatus (inner ear, vestibular nerve, parts of the cerebral cortex). Systemic dizziness can be central, intermediate or peripheral, depending on the location of the pathological process.
- Non-systemic dizziness is also called physiological. It manifests itself in the absence of pathological changes in the vestibular apparatus, but may be a consequence of its excessive irritation. Thus, non-systemic dizziness is one of the clinical signs of motion sickness syndrome, and also occurs after a long and monotonous rotation around its axis.
Symptoms of dizziness may vary. In this regard, it is also customary to distinguish several of its varieties:
- tactile - the patient experiences a sensation of loss of support under his feet, instability, as on a ship;
- proprioceptive - associated with a change in the identification of the body in space, with a feeling that the body is rotating around an axis, and the surrounding objects remain in their places;
- visual - visually the human body remains motionless, and the environment begins to move in different projections.
It is worth understanding that systemic dizziness manifests itself in a more vivid clinical picture. It is associated with damage to neural connections, so symptoms appear and remain even without an apparent reason. In addition, loss of balance is accompanied by other characteristic manifestations of damage to the nervous system or analyzer systems. Non-systemic dizziness is temporary and can go away spontaneously as soon as the vestibular system adapts to environmental changes. The second case does not pose a danger to humans.
Forms of vestibulopathy
There are several classifications that characterize this disease from different points of view.
- According to the course: acute, episodic, chronic vestibulopathy.
- By duration: vestibulopathy lasting seconds, minutes, hours, days, weeks or months.
- By localization: peripheral or central damage to the vestibular apparatus, as well as mixed.
- ICD-10: internal dizziness, disturbance of spatial orientation, vestibulovisual symptoms, postural symptoms.
Let's take a closer look at each type.
With the flow
The course of the disease plays a huge role in making a diagnosis and choosing further treatment.
- Acute vestibulopathy. Characteristic is the onset of symptoms spontaneously and once, which fades away within a few days or weeks. With this course, doctors suspect vestibular neuronitis, acute labyrinthitis, stroke in the vertebrobasilar region (VBB), traumatic vestibulopathy, multiple sclerosis.
- Episodic. Systemic attacks of vestibulopathy that recur. Duration ranges from a few seconds to several hours. Characteristic for: BPPV, Meniere's disease, transient ischemic attacks (TIA), panic attacks, vestibular migraine.
- Chronic. We are talking about symptoms that last for months or even years, progress, and concomitant disorders are added. Causes: tumors of the posterior cranial fossa, cerebellar degenerations, dyscirculatory encephalopathy (DE), chronic mental and behavioral disorders.
The most favorable therapy is acute, while for chronic it remains to rely on symptomatic treatment or surgery.
By duration
| Seconds | minutes | Watch | Days | Weeks, months |
| BPPV, perilymphatic fistula, vestibular paroxysm | BPPV, transient ischemic attack | vestibular neuronitis, Meniere's disease, vestibular migraine, perilymphatic fistula. | vestibular neuronitis, labyrinthitis, stroke, multiple sclerosis | psychogenic dizziness, dyscirculatory encephalopathy, neurodegenerative diseases of the brain |
By localization
Depending on the location of the lesion, symptoms will vary:
- Peripheral. In this case, we are talking about damage to the peripheral part of the analyzer, namely: the semicircular canals of the labyrinth, the vestibular ganglion, the vestibular nerve. Among the symptoms, peripheral genesis is indicated by: paroxysmal dizziness, rotational dizziness, change in the intensity of vertigo with a change in body position in space, nystagmus, change in body position in space. Peripheral lesions are characterized by a sudden onset with a rapid increase in symptoms. Most typical for diseases: BPPV, vestibular neuronitis, Meniere's disease or syndrome, labyrinthitis, perilymphatic fistula, neuroma of the cochleovestibular (VIII) cranial nerve.
- Central. In this case, the nuclei of the corresponding nerves in the brain are affected. Typically, this form of vestibulopathy occurs against the background of circulatory disorders in the brain, transient ischemic attacks, brain injuries, neoplasms, brain infections, and so on. Characterized by a slow progression of symptoms against the background of the presence of other symptoms of brain damage.
- Mixed. A difficult situation in which both the peripheral and central areas of the analyzer are affected. Occurs with serious circulatory disorders, skull injuries, intoxication, encephalopathy, and so on.
ICD-10 classification
The International Classification of Diseases offers the following variations of vestibulopathy:
- Internal dizziness. It is characterized by the appearance of a sensation of imaginary movement against the background of dizziness at rest, which intensifies when turning the head.
- Violation of spatial orientation. In this case, patients do not feel imaginary movement, but are poorly oriented in space.
- Vestibulovisual symptoms. Against the background of dizziness, a change in the perception of surrounding objects appears.
- Postural symptoms. When in a vertical position, an imbalance occurs: unsteadiness, a completed or incomplete fall, directional pulsation.
ICD-10 is most suitable for medical documentation, but is less popular in real clinical practice.
Main causes of the symptom
Dizziness can be a symptom of a number of diseases and pathological conditions that lead to disruption of the vestibular apparatus. These are congenital or acquired disorders of varying severity, with different mechanisms of development and characteristics of clinical manifestations. Among the most common groups of causes of this symptom are the following:
- inflammatory diseases of the inner ear and vestibular nerve - can be of infectious or non-infectious origin;
- intoxication and poisoning, which lead to disruption of the vestibular apparatus;
- traumatic brain injuries - when certain areas of the cerebral cortex are damaged, dizziness may appear after a long time;
- metabolic disorders, including diabetes.
Impaired balance and coordination of movements in space can also be a variant of the norm. In some cases, intense irritation of the vestibular apparatus occurs (on a carousel, during a long stay on a ship or on another unstable support), after which the nervous system needs time to recover. It is impossible to determine the cause of dizziness at home, especially if it is a consequence of organic lesions of the central nervous system.
Classification
In medicine, vestibular syndrome is divided into forms, depending on the causes of its appearance:
- Vertebrogenic vestibulopathy. Appears in pathological processes of the cervical spine, which arise due to the development of diseases in this area. For example, vestibulopathy develops with cervical osteochondrosis and osteoporosis. There is also vestibulopathy syndrome due to instability of the vertebrae - due to compression of arteries, nerve endings, or due to a hernia.
- Acute peripheral. Peripheral vestibular sudden syndrome will appear when an inflammatory process occurs in the inner ear. Such a disorder of the vestibular system can occur in any person, regardless of age and gender. Occurs due to viral or infectious-allergic pathologies occurring in the body.
- Post-traumatic. Development is influenced by several factors: concussion, disruption of membrane integrity, which leads to damage to the eardrum and hemorrhages in the middle ear. May appear due to decompression.
Particular discomfort is caused by salt deposits in the cervical spine, one of the most unpleasant symptoms of which is dizziness. In the medical record, the doctor may diagnose “vestibulopathy developing against the background of cervical osteochondrosis.”
Clinical picture of different types of dizziness
The main clinical manifestation of dizziness is a feeling of loss of balance and imaginary movement of the body in space. However, this symptom may indicate a number of different disorders, the symptoms of which will differ. At the Clinical Brain Institute, you can undergo a full examination using laboratory and instrumental techniques that will allow you to detect all possible diseases that cause dizziness. However, even an initial examination and medical history will clarify the picture and make a preliminary diagnosis. Systemic dizziness, as a manifestation of functional disorders of the vestibular apparatus, should be considered separately from non-systemic dizziness, which does not pose a danger and can even be considered a variant of the norm.
Systemic dizziness
Systemic dizziness includes a number of diseases associated with various disorders of the conduction of nerve impulses to the cerebral cortex. The pathological process can be located at any level, and therefore the symptoms will differ. Thus, each pathology that may underlie the mechanism of development of dizziness should be considered separately. Systemic types occur in no more than a third of patients and require more detailed examination.
- Benign paroxysmal positional vertigo (BPPV) is the main cause of systemic varieties. The process is associated with the formation and deposition of crystals of calcium carbonate salts on the tissues of the semicircular canals of the inner ear. This is an acquired chronic disease, the leading clinical sign of which is short-term dizziness and loss of orientation in space. The attacks last no more than 1 minute, with no additional symptoms (headache, tinnitus).
- Inflammation of the vestibular nerve (vestibular neuronitis) is a dangerous condition that often develops against the background of a bacterial or viral infection. Its reproduction with damage to the nervous system causes a characteristic set of symptoms, which includes dizziness. The duration of their manifestation ranges from several hours to several days, and their intensity remains high or even intensifies. Hearing is preserved in vetibular neuritis.
- Post-traumatic dizziness is complete or partial disorientation that develops immediately after a traumatic brain injury. The process is associated with damage to areas of the cerebral cortex responsible for transmitting information about the position of the human body in space. Clinical signs may vary in intensity and persist until the tissue has completely healed, and in some cases they appear several days after the injury.
- Intoxication is another cause of dysfunction of the vestibular apparatus. Toxins, including aminoglycosides, can accumulate in peri- and endolymph, the fluid that fills the structures of the inner ear.
- Meniere's disease is a disease in which there is an increase in the amount of endolymph (hydrops). The fluid is located in the lumen of the labyrinth of the inner ear, and an increase in its volume leads to excess pressure on its walls. The disease occurs in attacks, the interval between which can range from several days to several months. The duration of one attack is from several hours to a day, and the symptoms are very pronounced. The patient experiences acute disorientation in space, dizziness and headaches. The disease progresses and causes gradual deterioration of hearing (usually a unilateral phenomenon), but complete loss does not occur.
- Temporal lobe epilepsy is a pathological condition that is manifested by a periodically manifested complex of autonomic disorders (dizziness, headache, low blood pressure, and others). The patient's condition deteriorates suddenly, for no apparent reason, and the attack may be accompanied by deterioration of vision.
- Lipotymic conditions are a set of symptoms that precede fainting. The patient experiences severe dizziness, weakness, his skin and mucous membranes turn pale, and his heartbeat becomes less frequent. An attack can occur for many reasons, including diseases of the cardiovascular system, a decrease in blood glucose concentration, an increase or decrease in blood pressure.
Systemic dizziness most often occurs in old age, but can also occur in young people. The development of the disease should be monitored over time, taking into account the frequency and intensity of attacks. It is also important to monitor the occurrence of additional signs: hearing and vision impairment, fainting, nausea, migraines. These data will make it possible to determine the severity of violations even before specific analyzes are carried out.
Non-system varieties
One of the most characteristic signs of non-systemic dizziness is that its clinical manifestations intensify if you close your eyes. The causes of this condition may be various dysfunctions of the cerebellum and other structures that regulate motor activity and coordination of movements. Additional clinical signs include general weakness and drowsiness, decreased visual acuity, deterioration of memory and attention. Similar symptoms may occur with systemic use of certain groups of drugs (benzodiazepines). The patient's condition in such cases improves by adjusting the dosage of medications.
Dizziness: central and peripheral.
And so: what is dizziness?
Dizziness is a feeling of uncertainty in determining one’s position in space, apparent rotation of surrounding objects or one’s own body, a feeling of instability, loss of balance, the ground moving away from under one’s feet.
This is one of the most common reasons for visiting doctors of various specialties. Thus, in a survey of more than 20 thousand people aged 18 to 64 years, it turned out that more than 20% experienced dizziness in a month, of which more than 30% suffered from dizziness for more than 5 years. On average, about a quarter of the world's population suffers from vertigo.
The reasons for these sensations are different. At the same time, the scheme of differential diagnostic measures should cover a wide range of conditions, sometimes requiring the differentiation of such life-threatening conditions as acute cerebrovascular accident, cardiac arrhythmia and more common diseases of the inner ear, as well as dizziness of non-localized origin.
Various etiological factors include:
- diseases of the middle and inner ear of an inflammatory and non-inflammatory nature;
- diseases of the central nervous system;
- lesions of the neck organs, including degenerative-dystrophic changes in the cervical spine;
- metabolic and hematological causes;
- drug-induced disorders;
- infectious lesions;
- cardiogenic disorders;
- psychogenic disorders
- other reasons.
Classification of dizziness by etiology and clinical manifestations:
1.Vestibular or systemic:
— Peripheral:
- With hearing impairments;
- No hearing impairment.
-Central;
- Non-vestibular or non-systemic;
Most often, vestibular (systemic) spinning in the head occurs against the background of pathologies of the vestibular, visual apparatus or musculoskeletal system.
Peripheral vestibular vertigo occurs when the sensory elements of the ampullary apparatus and vestibule, vestibular ganglion and nerve conductors of the brain stem are damaged and is characterized by a paroxysmal course, variable intensity, accompanied by ataxia and autonomic manifestations. With an acute onset, patients feel the movement of objects towards a more actively working labyrinth; nystagmus is also directed in the same direction - spontaneous regular, clonic, horizontal or horizontal-rotatory nystagmus, of varying intensity and degree, associated with a harmonious deviation of the torso and arms towards the slow component . There is a positive effect of changing the position of the head (towards the slow component of nystagmus). As a rule, peripheral vestibular vertigo is a one-sided process and is accompanied by impaired auditory function on the affected side, however, in a number of diseases that most clearly reflect the true clinical picture of peripheral vestibular syndrome (benign paroxysmal positional vertigo, vestibular neuronitis and, for the first time, in the vestibular form of Meniere's disease) , hearing remains intact.
- Benign paroxysmal positional vertigo (BPPV) is the most common type of otogenic vertigo, occurring in approximately 20% of all cases of vertigo and 50% of cases of otogenic vertigo. The clinical picture of BPPV is characterized by short episodes of dizziness, provoked by changes in head position. BPPV is caused by otolith debris in the posterior canal of the inner ear. dizziness in a patient
- Vestibular neuritis is characterized by dizziness, nausea, ataxia and nystagmus. The clinical picture of labyrinthitis is represented by the same symptom complex in combination with tinnitus and/or hearing loss. Vestibular neuritis and labyrinthitis are the causes of dizziness of otogenic origin in 15% of cases.
- The clinical picture of Meniere's disease is characterized by periodic dizziness, accompanied by hearing impairment. In Meniere's disease, expansion and periodic rupture of the endolymphatic receptacle of the inner ear is observed. Meniere's disease affects approximately 15% of patients with otogenic vertigo.
- Bilateral vestibular paresis is manifested by oscillopsia and ataxia. It is usually caused by a decrease in the number of vestibular hair cells. Typically, previous use of ototoxic antibiotics (intravenous or intraperitoneal) for several weeks, most often gentamicin. Bilateral vestibular loss is uncommon.
- Perilymphatic fistula (PS) is manifested by sensitivity to changes in pressure or hydrops symptom complex, or ataxia caused by physical activity. In PS, there is communication between the fluid-filled inner ear and the air-filled middle ear. Barotrauma, such as from scuba diving, is the most common mechanism of PS. Another common cause of PS is surgery to treat otosclerosis or cholesteatoma. PS is extremely rare.
- The clinical picture of tumors compressing the eighth cranial nerve is characterized by asymmetric hearing impairment, accompanied by moderate ataxia. Among patients suffering from vertigo, tumors of the eighth cranial nerve are rare; they are more often observed in cases of unilateral hearing loss.
Central vestibular vertigo
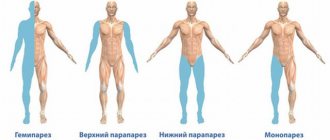
Its cause is dysfunction of the central structures that ensure the conduction of sensitive impulses from the inner ear, their connection with the vestibular nuclei in the brain stem, with the cerebellum, with the oculomotor nuclei, as well as communication with the cerebral cortex. This type of lesion is characterized by a sensation of pushing forward, backward, to the sides, and the presence of other signs of central nervous system damage: diplopia, dysarthria, loss of sensitivity, paresis.
The most common signs of central damage to the vestibular system are
- vertical nystagmus;
- nystagmus changing direction;
- atypical nystagmus (especially downward nystagmus) in the head shake test;
- asymmetric oculomotor dysfunction;
- severe postural instability with falls.
In most cases, central vertigo is caused by vascular disorders (stroke, transient ischemic attack, vertebrobasilar migraine), which accounts for 60% of calls.
- Stroke and transient ischemic attack (TIA), in which pathological changes occur in the brain stem or cerebellum, cause central vertigo in approximately 1/3 of cases. Isolated dizziness can sometimes be the only symptom preceding a stroke localized in the structures of the posterior cranial fossa. Almost always, symptoms of dizziness are accompanied by other focal signs of central nervous system damage.
- Vertebrobasilar migraine most often presents with dizziness and headache, but may present as dizziness alone. Migraine causes about 15% of all cases of central vertigo. Migraines are especially common in women between the ages of 30 and 40. The attacks are stereotypical, often accompanied by photophobia, soundphobia, visual or other aura.
- Epileptic seizures are characterized by dizziness combined with confusion, motor symptoms, or, more commonly, a spinning sensation. About 5% of cases of central vertigo are associated with epileptic seizures.
- In multiple sclerosis (MS), dizziness is combined with other signs of central nervous system damage, for example, cerebellar dysfunction. MS is not a common cause of dizziness, although many patients consider this disease to be the cause of such symptoms. The share of PC in the structure of all cases of central vertigo is 2%.
- Arnold-Chiari malformation is a developmental anomaly in which there is a hernial protrusion of the cerebellar tonsils 5 mm or more below the level of the foramen magnum. Patients complain of dizziness, ataxia and headaches in the occipital region; they often experience vertical nystagmus. Symptoms are triggered by straining and coughing. Occurrence: 1% of all cases of central vertigo.
Non-vestibular (non-systemic) dizziness is a feeling of lightheadedness, loss of stability, loss of balance, “loss of ground under your feet,” “darkening in the eyes,” and ringing in the ears. Often, these conditions precede the development of fainting (lipothymia), although complete loss of consciousness may not occur. Characteristic of states of non-systemic dizziness are pronounced emotional disorders - a feeling of restlessness, anxiety, fear or, conversely, depression, powerlessness, a sharp loss of strength. A number of patients experience a combination of manifestations of both systemic and non-systemic dizziness. Especially often, a similar picture occurs in elderly and senile patients, against the background of a combination of several predisposing factors.
Causes of mixed and non-systemic dizziness of non-cerebral origin include fluctuations in blood pressure, low blood sugar and/or metabolic disorders associated with medications or systemic infection. In most cases, these conditions require emergency care and are observed in 33% of patients with attacks of dizziness. Such conditions are rare when seen by specialists (2-5%). Basically, these are conditions that a doctor may encounter during emergency care.
- Postural hypotension may cause lightheadedness, weakness, blurred vision, or fainting. This condition is observed only when the patient is in an upright position.
- The clinical picture of cardiac arrhythmia is characterized by fainting or a sudden fall. As with postural hypotension, clinical symptoms develop only when the patient is in an upright position.
- Hypoglycemia and metabolic disorders are manifested by weakness, lightheadedness, dizziness, and darkening of the eyes. Taken together, they account for about 5% of cases among patients with non-systemic dizziness of non-cerebral origin.
- When exposed to drugs or other substances, weakness, lightheadedness, and darkening of the eyes usually occur, but true dizziness can also develop. This condition is diagnosed in 16% of patients with all types of dizziness during emergency care, but is rare outside the emergency department. Most often, such disorders are caused by antihypertensive drugs, especially alpha-adrenergic blockers, for example, terazosin, calcium channel blockers with a pronounced vasodilating effect, for example, nifedipine, and sedatives. Some commonly prescribed benzodiazepines, such as Xanax, cause dizziness, which is part of the drug's withdrawal symptoms. Drugs that suppress vestibular dysfunction, such as meclizine and scopolamine, may cause these sensations by acting directly on the central vestibular pathways.
- Viral infections that are not accompanied by ear damage, according to the literature, can cause a symptom complex of dizziness in 4-40% of patients who seek emergency help for this reason. Clinical manifestations of viral infections may include, for example, gastroenteritis and flu-like symptoms.
- Psychogenic dizziness is obligately accompanied by severe fear and anxiety, as well as autonomic disorders - cardiovascular and respiratory. Most often, dizziness is observed against the background of hyperventilation syndrome; rapid and shallow breathing leads to metabolic disorders, increased neuromuscular excitability, etc. In this case, patients define their sensations as lightheadedness, lightness of the head, and often the symptoms of dizziness are combined with noise and ringing in the ears, increased sensitivity to sound stimuli, instability when walking. Psychogenic dizziness often occurs during a panic attack . Symptoms of fear, shortness of breath, palpitations, and nausea may occur simultaneously with symptoms of lightheadedness, lightheadedness, fear of falling, and loss of balance.
There are more than 80 diseases, one of the symptoms of which is dizziness. To understand which of them caused systemic dizziness, you should consult a therapist. After a thorough examination, questioning and history taking, he can make a diagnosis. If the cause cannot be identified, additional diagnostic methods are prescribed: CBC, LBC, CT/MRI of the brain, cervical spine, EEG, LA, ultrasound of the central nervous system, ECG/Holter ECG, examinations by various specialists: ENT doctor, neurologist, cardiologist and etc. as needed.
The specialist doctor performs simple diagnostic techniques that do not require special equipment, allowing for a differential diagnosis of dizziness: the de Klein test, the Dix-Hallpike test, the Halmage test (head rotation test) and the head shaking test and other techniques.
Treatment : the main groups of basic therapy drugs used in the treatment of dizziness:
- Antihistamines (Clemastine, meclozine (25-100 mg/day in the form of chewable tablets) improve the general condition of the patient in the first 2-3 days of the disease.
- Angioprotector-vertigolytic betahistine 24 mg 2 times a day (48 mg per day) helps restore balance for 2-3 months or more
- Vasoregulatory drugs (Vinpocetine, Nicergoline).
- Nootropics (Piracetam, Nootropil, Phenibut, choline alfoscerate, etc.).
- Tranquilizers (diazepam 10 mg (2.0) IM and others). They are able to eliminate anxiety and panic attacks. The use of drugs that have a sedative effect is possible in the first 2-3 days of acute dizziness
- Eufillin and Metoclopramide will help with nausea and vomiting. The use of dimenhydrinate (50-100 mg 2-3 times a day), diphenhydramine (25-50 mg orally 3-4 times a day or 10-50 mg intramuscularly) is also recommended.
- Vestibular gymnastics.
Depending on the immediate cause of the disease, additional etiotropic, pathogenetic, metabolic and prophylactic drugs are used.
Relief of acute vestibular syndrome involves the use of antiemetics (antiemetics) and vestibular suppressants. The duration of use of vestibular suppressants and antiemetics is limited by their ability to slow down vestibular compensation and should not exceed 2-3 days.
In case of vestibular neuronitis and labyrinthitis, intramuscular administration of vestibular suppressants and antiemetics is indicated in the first 2–3 days to relieve the manifestations of acute vestibular crisis. After nausea has stopped for 1–3 months, betahistine is prescribed orally at a daily dose of 48 mg. During the same period, a course of vestibular rehabilitation (gymnastics) should begin according to an individual program. Depending on the characteristics of the pathogenesis of vestibular neuronitis and labyrinthitis, appropriate drug treatment is prescribed. Thus, for vestibular neuronitis, relatively high doses of glucocorticosteroids are used, for example, methylprednisolone at an initial dose of 100 mg, followed by a dose reduction of 20 mg every 3 days. Treatment of labyrinthitis may require antibacterial or antiviral drugs, depending on the pathogen. In addition, for labyrinthitis, in some cases surgical treatment is resorted to. With labyrinthitis, unlike vestibular neuronitis, patients often require subsequent auditory rehabilitation.
The use of drug treatment for BPPV . The Semont and Eple maneuvers (methods) and the Brandt-Daroff exercises are considered preferable and most popular for the treatment of BPPV in cases of damage to the posterior canal.
For an acute fistula, conservative treatment is quite effective with mandatory bed rest for a week (the head should be elevated) and the exclusion of physical activity for another 1.5–2 months.
For Meniere's disease, in the interictal period, complex treatment (maintenance therapy) is indicated to prevent the development or reduce endolymphatic hydrops: diuretics, vasodilators (histamine analogue-betagistine in a daily dose of 48 mg for 2-3 months or more), corticosteroids.
Planned (preventive) treatment of vestibular migraine is carried out in accordance with the classical principles of migraine treatment using beta blockers, anticonvulsants, tricyclic antidepressants and selective serotonin and norepinephrine uptake inhibitors.
Treatment of central vertigo associated with stroke at VBB is carried out according to the principles of stroke therapy in a neurological hospital for stroke patients.
Surgical treatment of vertigo is applicable to space-occupying lesions and abnormalities.
In some particularly severe cases, surgical treatment for peripheral vertigo is possible. In case of BPPV, filling of the affected semicircular canal with bone chips is indicated in case of ineffectiveness of therapeutic maneuvers (0.5-2% of BPPV cases).
If conservative treatment is ineffective for other causes of peripheral vestibular vertigo, the following may be performed:
- Selective neurectomy of the vestibular nerves;
- Labyrinthectomies;
- Laser destruction of the labyrinth.
It is recommended to carry out vestibular rehabilitation . Correction of the patient's anxiety, feelings of uncertainty and fear is mandatory. Preference should be given to vestibular rehabilitation using special installations - postulographic and stabilographic complexes, which allow simultaneous assessment of the effectiveness of treatment. An active rehabilitation strategy with early activation of the patient is necessary.
specific prevention of peripheral dizziness.
Department of Neurology, 10th City Clinical Hospital
neurologist Drik O.N.
Diagnostic methods
The Clinical Brain Institute has all the conditions for a full diagnosis of dizziness. The process is carried out by analyzing the work of the vestibular apparatus and the brain, after which the localization of the pathological process and its stage can be detected. During the initial examination, it is important to conduct a detailed interview with the patient and obtain a detailed description of the complaints. At this stage, it is possible to differentiate true dizziness from other conditions that are also often called by this term. Next, specialists will select an individual diagnostic scheme, which may include the following steps:
- examination of the spinal column (analysis of X-rays, CT or MRI) to identify osteochondrosis, vertebral displacements and other pathologies that cause impaired blood supply to parts of the brain;
- examination by a neurologist, which includes determination of nystagmus, various tests and assessment of the ability to coordinate movements;
- examination of the state of the brain using MRI or CT - carried out to exclude tumors and other diseases leading to demyelination of nerve fibers;
- electroencephalography is a way of assessing brain activity by capturing the signals it produces;
- study of the functioning of the vestibular apparatus - may include rotational tests, vestibulometry and other tests.
Instrumental techniques are prescribed after a general examination. Based on the data obtained, the doctor can determine what examinations need to be performed in order to conduct a differential diagnosis and exclude possible causes of dizziness. Thus, if Meniere's disease is suspected, patients are offered a test to detect low-frequency sound signals.
Treatment and prognosis
Specialists at the Clinical Brain Institute will select the most effective treatment regimen, depending on the diagnostic results. In most cases, dizziness does not pose a threat to the life and health of the patient and is easily corrected with general measures and medication. Thus, the following methods of treating the causes and clinical signs of this condition may be recommended:
- constant monitoring of blood pressure indicators, if necessary, taking antihypertensive drugs;
- preventing the appearance of edema - limiting salt intake, prescribing diuretics (diuretics);
- taking vestibulics - drugs to eliminate the symptoms of dizziness;
- if necessary - antihistamines, anti-epileptic drugs;
- restoration of movement coordination with special exercises.
Dizziness is not a disease, but one of the symptoms of a dysfunction of the vestibular apparatus. It is impossible to determine its cause at home, so if it occurs, it is worth undergoing a comprehensive diagnosis at the Clinical Brain Institute. It employs broad and specialized specialists who regularly examine and treat patients with similar symptoms. The medical center also has the opportunity to undergo complex examinations using high-quality equipment necessary to make a diagnosis. Despite the fact that dizziness alone is not a dangerous symptom and cannot threaten the patient’s life, it can indicate serious problems with the vestibular system and organic lesions of the central nervous system in the early stages. It is impossible to cure these pathologies on your own, but an integrated and competent approach in a hospital setting will eliminate both the causes and manifestations of dizziness.
Clinical Brain Institute Rating: 4/5 — 6 votes
Share article on social networks
Treatment
Only a qualified specialist can prescribe treatment for developing vestibulopathy after diagnosing and making a correct diagnosis.
It is necessary to treat vestibular syndrome, taking into account the reasons for its occurrence, the general condition of the patient, the symptoms displayed, and the individual characteristics of the patient.
The general purposes are:
- the use of drugs that inhibit the activity of vestibular receptors and ascending conduction systems;
- antibiotics if vestibular apparatus disorders occur due to infectious pathologies of the middle or inner ear;
- medicines for blood vessels that will help improve and restore blood supply to the brain.
When the disease is in remission, it is recommended:
- acupuncture - unless it provokes peripheral vestibular sudden syndrome;
- therapeutic massage course;
- treatment with leeches;
- reflexology;
- physiotherapeutic procedures;
- magnetic therapy;
- exercises on electric exercise machines;
- physical therapy classes.
Therapeutic exercises can be done if vestibulopathy is in stable remission.
With your doctor's permission, you can use various traditional medicines to reduce the occurrence of dizziness. However, they must be used in combination with prescribed medications - this is the only way to achieve a positive result.
Vestibulo-atactic syndrome responds very well to surgical treatment. The operation is prescribed extremely rarely. Indications may include traumatic membrane damage, labyrinthine infarction, or hemorrhage. These situations are very dangerous for human life. The operation is performed for vascular pathologies that can provoke spasm.
During surgery, vasomotor fibers will be restored and blood flow in the affected areas will improve.