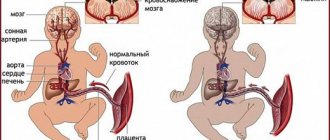
Perinatal lesions of the central nervous system (PPCNS) are a group of pathologies in which the normal functioning of the spinal cord in newborns is disrupted. The process can develop for various reasons, one of them is hypoxia, that is, oxygen starvation. The perinatal period includes the last trimester of pregnancy, childbirth and the first week of the baby's life. During this time, the body experiences stress during the transition to pulmonary breathing, as well as during adaptation to various environmental factors, therefore hypoxic-ischemic damage to the central nervous system is a common diagnosis. 10% of newborns experience oxygen deficiency to varying degrees, especially premature ones. The condition requires urgent medical attention, but in 80% of cases it has a favorable outcome and does not in any way affect the further development of the child.
Why is cerebral hypoxia dangerous?
Even mild hypoxia of the brain is a dangerous condition for health, which leads to pathological changes that affect the entire body as a whole.
The stronger the oxygen starvation, the more severe its consequences. The prognosis depends on the degree of damage to brain tissue and how long the hypoxia lasted. If a person falls into a coma for a short period of time, then the chances of full rehabilitation are quite high. If the patient was not in a coma, he will recover even faster (subject to adequate and timely medical care).
If a person was in a coma for a long time, but came out of it, then such a state cannot remain without consequences. The life expectancy of such patients most often does not exceed one year. At the same time, bedsores form in bedridden patients; they are more susceptible to infectious diseases, the causative agents of which are hospital strains of bacteria. They are characterized by increased resistance to therapy. In immobilized patients, the risk of blood clots forming in the veins increases.
After experiencing clinical death, a person may lose a number of neurological functions.
The forecast could be as follows:
- Full restoration of brain functions and normalization of the condition can occur in several days or months if the brain tissue has not been destroyed. In this case, the patient will experience asthenic syndrome throughout the entire rehabilitation period. Sometimes, after a significant improvement in well-being, a secondary deterioration may occur, and neurological disorders will be persistent.
- Partial restoration of neurological functions is observed when some brain cells die. Rehabilitation and the patient’s return to normal life occurs slowly. Some functions may not be restored at all.
Complete recovery is rare, but if treatment is carried out correctly, stable remission can be achieved.
Brain cells do not recover after hypoxia, however, it is possible to achieve normalization of the body’s condition. The brain has the ability to take over the functions of neighboring cells, but only partially. Therefore, help with hypoxia should be immediate. Otherwise, the complications and consequences of oxygen starvation of the brain will be critical.
Treatment of oxygen starvation of the brain
Before starting treatment for oxygen starvation in adults, it is necessary to establish the exact cause that provoked this condition
Therefore, it is important for the patient to clearly formulate the factors that could lead to this. Most often in an adult it is smoking, alcohol abuse, prolonged stay in a poorly ventilated area
Having assessed the severity of oxygen starvation, the doctor will recommend treatment in a hospital or at home. The patient is prescribed medications that stabilize the normal functioning of the body. It is also necessary to take medications whose action is aimed at restoring normal blood supply to brain tissue.
? Read the detailed article on how to get rid of pain.
Sometimes, to relieve symptoms of mild oxygen starvation, it is enough for an adult to ventilate the room in which he is located or go outside. The situation is different if the cause is some kind of disease or disruption of the body.
If oxygen starvation provokes a disease of the blood, cardiovascular or respiratory system, the patient will require more serious measures to eliminate it.
- For exogenous hypoxia, oxygen equipment (masks, pillows, etc.) is used.
- To treat respiratory hypoxia, analgesics, antihypoxanes and drugs that dilate the bronchi are used. Sometimes artificial ventilation is performed.
Remember that some analgesics have a negative effect on the body and are addictive. It is important to be able to distinguish which of them are narcotic and which are non-narcotic
- Hemic hypoxia requires blood transfusion, which helps normalize blood circulation.
- With a circular form of oxygen starvation, surgical intervention on the heart or blood vessels is necessary.
- To treat the histoxic form, antidote drugs are used.
If the patient sees a doctor in time and is prescribed effective treatment, the prognosis for recovery will be favorable. However, if oxygen deprivation continues for a long period of time, irreversible consequences may develop that cannot be eliminated.
You can learn interesting facts about the disease from pediatrician, family doctor Konstantin Borisovich Zabolotny:
Diagnostics:
It is necessary to conduct an ultrasound examination of the fetus, use cardiotocography (recording of the fetal cardiac activity) and Dopplerometry (study of the blood flow of the vessels of the uterus and umbilical cord of the fetus) with the frequency prescribed by the attending physician. Auscultation (listening) of the fetal heartbeat with a stethoscope is also used. It should be noted that not every pregnancy occurs against the background of the above diseases, complicating intrauterine fetal hypoxia. To prevent the possible occurrence of hypoxia, special attention is paid to its prevention: long walks in the fresh air, mandatory dosed physical activity (gymnastics, exercises, exercises for pregnant women and breathing exercises, swimming, yoga). It is possible to use hyperbaric oxygen therapy (HBO) as prescribed by the attending physician. It must be remembered that treatment must be prescribed by a gynecologist, be comprehensive and take into account an individual approach to each expectant mother.
How does cerebral hypoxia manifest?
Depending on the severity of brain disorders during hypoxia, there are:
- Mild degree. This is manifested by symptoms such as lethargy, stupor, or, on the contrary, a person becomes hyperexcited, he experiences euphoria, blood pressure rises, and the heartbeat quickens. The palpebral fissures become uneven in size as a result of facial nerve paresis. If the pathogenic factor that affects oxygen starvation of the brain is not eliminated, then after a few hours or days it will move to the next stage.
- Average degree. The patient retains paresis of the facial nerve, mucous membrane reflexes and tendon reflexes are most often reduced. From time to time, cramps may occur that begin in the face and then spread to the trunk and limbs. Anxiety and psychomotor agitation are increased. The victim has difficulty oriented in space, his memory and other cognitive abilities deteriorate.
- Severe degree. The patient experiences deep depression of consciousness with loss of voluntary activity, but reflexes are preserved. This condition is called soporous. Sometimes already at this stage a person falls into a severe coma. He develops convulsions of the upper and lower extremities, grasping and sucking reflexes appear, and muscle tone decreases. A persistent increase in temperature, increased sweating and lacrimation are possible.
- Critical degree, which poses a threat to life. This condition is characterized by a deep coma, all structures of the brain are affected. The patient's skin is cold, there is no facial expression, the eyeballs are motionless, the pupils are dilated and do not react to light. The mouth remains half-open, the eyelids are closed, and the skin is cyanotic. The heart works weakly, vascular tone is reduced. As hypoxia progresses, the functions of the cerebral cortex fade away. A person dies if his life is not supported with the help of an artificial respiration apparatus and means for toning cardiovascular activity.
Separately, it is necessary to describe the symptoms of chronic cerebral hypoxia, which include:
- Increased fatigue.
- Excessive irritability.
- Emotional incontinence.
- Decrease in intelligence.
- Violations of the emotional-volitional sphere.
- Deterioration of memory and attention.
- Bad mood.
- Increased tearfulness.
- Apathy.
- Most often, people become indifferent to everything that is happening, less often they are complacent and euphoric.
- Often a person experiences headaches.
- Periodic attacks of nausea are possible.
- Night rest is disrupted, and during the day a person experiences bouts of drowsiness. He falls asleep with difficulty, his sleep is shallow and intermittent. The patient often has nightmares. After a night out, a person feels tired and unrested.
- Chronic hypoxia is characterized by autonomic disorders, including: increased pulsation in the head, the appearance of tinnitus, frequent episodes of darkening of the eyes, a feeling of a rush of heat to the head. The heart rate increases, and heart pain and shortness of breath may occur. Even episodes of loss of consciousness are possible.
Pathophysiology of hypoxic-ischemic brain damage
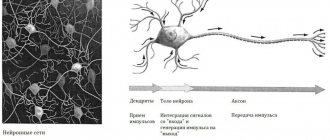
Pathophysiology of hypoxic-ischemic brain injury Pathophysiology of hypoxic-ischemic brain injury (HIP BM). Due to the fact that HIP GM is the most common cause of neonatal seizures (NS), in experimental studies it is posthypoxic seizures that serve as a model for studying various aspects of NS. Nervous tissue, compared to other tissues, is more sensitive to the effects of hypoxia. However, immature brain cells are more resistant to oxygen deprivation than adult nerve cells. This is due to the relatively low energy requirements of the immature brain, as well as a smaller number of the most vulnerable highly differentiated neurons. Some researchers see predominantly cerebrovascular mechanisms as the basis for the pathogenesis of HIP GM. Cellular and molecular mechanisms of excitotoxicity associated with hyperstimulation of excitatory (mainly glutamate) neurotransmitter receptors also play a key role in the development of GM HIP. In the immature neonatal brain, NMDA receptors are expressed, which form channels with a longer opening time and a greater flow of calcium into the cell, which normally provides a high level of trophic stimulation necessary for neonatal neurons, and under conditions of hypoxia-ischemia triggers the process of cell death. In addition, in newborns, the processes of apoptosis following cerebral ischemia are more pronounced due to the insufficient activity of enzymes that suppress apoptosis and the high activity of proapoptotic caspases. Clinical manifestations of excessive excitatory mediation and excitotoxicity are neonatal seizures and abnormalities of bioelectrical activity. The ischemic cascade lasts from several hours to several days, which coincides in time with the duration of attacks in the acute period of GIP GM.
Mechanisms of the damaging effects of seizures on the nervous system. The severity of neurological outcomes in children with NS depends on a number of reasons, and is primarily determined by the influence of the initial nosological factor that causes seizures. In addition, a negative effect of antiepileptic drugs on the immature brain cannot be excluded, which may exceed the negative effect of the seizures themselves. The question of the effect of seizures themselves on the immature brain is currently being discussed. It was previously thought that the developing brain is resistant to the damaging effects of seizures, and this resistance persists until 7-15 days of age. To date, evidence has been obtained that NS can cause disturbances in cerebral organization and neurogenesis, mainly in the hippocampus and border cortical areas of the blood supply. These disorders are clinically manifested by deterioration of memory, learning, behavior, and also predispose to recurrence of seizures at an older age. When comparing functional MRI data in newborns with seizures and newborns with similar structural defects, but without seizures, a significant (more than 3 times) increase in the ratio of lactate to choline was found in children with NS, which correlated with the severity of seizures and did not depend on the degree structural changes in the studied children. At the same time, a final answer to the question of how the damaging effect of seizures on the developing brain is realized has not been obtained.
The theory of excitotoxicity, the theory of brain damage during seizures due to depletion of energy reserves and impaired mitochondrial function, is discussed. Data were also obtained on changes in systemic and cerebral hemodynamics at the time of recording ictal activity, regardless of the presence or absence of a clinical component of a convulsive attack. In addition, to date, an original theory is receiving more and more evidence in animal experiments that the degree of brain damage in NS., and, consequently, the severity of outcomes, is determined by hyperthermia, which accompanies seizures and is associated with the effect of seizures on the hippocampus, and also general cerebral hypermetabolism. Prevention of hyperthermia in newborn rat pups led to a reduction in the functional and morphological consequences of seizures.
Thus, evidence of the damaging effects of seizures on the immature brain supports the need to develop effective and early methods for diagnosing and treating AN.
ECD and the reasons for its high incidence in newborns. Currently, the issue of clinical-electrographic dissociation (ECD) is widely debated; this is the name given to the phenomenon of discrepancy between the clinical and electroencephalographic manifestations of seizures. Two possible mechanisms for the absence of electrographic correlates of seizures in certain types of seizures in newborns have been discussed for a long time. Some researchers suggest that electrical activity in these cases is generated in the subcortical regions and does not reach the cortex, and therefore is missed during EEG studies. According to another point of view, clinical seizures with ECD are non-epileptic in nature, being automatisms associated with the release of brain stem structures from inhibitory cortical influences, the so-called phenomenon of functional decortication. The frequency of such attacks in newborns is significant and ranges from 12-16% to 70%. Clarification of the mechanisms of origin of ECD is essential for developing a strategy for the management of newborns with electro-clinical disconnection (in particular, in determining the need for antiepileptic therapy). The relevance of the study of the mechanisms of ECD is emphasized by the fact that despite the possibly non-epileptic nature of the paroxysms, the prognosis for neuropsychic development in ECD remains as poor as in typical epileptic seizures, mortality is 20%, severe neurological complications develop in 50% of surviving children.
Another variant of the discrepancy between the clinical and electroencephalographic manifestations of seizures in newborns is “occult seizures” or “electographic” seizures), which means the registration of patterns of epileptic seizures in the absence of clinical seizures. The proportion of children with “hidden seizures” relative to all newborns with seizures is very high and ranges from 42-55% to 79-85% according to various authors. In a prolonged EEG study of 40 newborns with EEG seizures, clinical correlates of seizures were found in only 1% of all identified “electographic seizures.” Antiepileptic therapy, which often stops only the clinical component of the seizure, as well as the use of muscle relaxants to synchronize with artificial ventilation are considered as the causes of “hidden” seizures. In other cases, to explain this phenomenon, an original hypothesis is proposed, which is that the clinical picture of the attack is not realized due to the localization of the focus in areas that are clinically silent during the neonatal period. In addition, there is a suspicion that the high frequency of latent seizures is based on an underestimation of clinical ictal activity, in particular, autonomic symptoms (changes in oxygenation, heart rate, pupil size) may be visible. “Occult” seizures can be considered as a harbinger of a bad outcome with a recommendation for the mandatory use of anticonvulsant therapy, or as a symptom that does not have independent prognostic significance at all and does not require drug correction. Some researchers believe that the prognosis of “hidden” seizures depends entirely on the number and frequency of recorded seizures. In particular, the presence of “electrographic” seizures in the recording closely correlated with the future development of microcephaly, epilepsy, and severe forms of cerebral palsy, especially if their identified number exceeded 75. On the other hand, there are no studies that have proven the effectiveness of anticonvulsant therapy in relieving electrographic seizures, and on further neurological prognosis. As a result, the questions of the need to treat latent seizures, the choice of the most appropriate drug and treatment regimen, as well as the criteria for selecting newborns for deciding on the prescription of anticonvulsants remain open. Considering the frequency of “electrographic seizures,” solving this problem is of high relevance today.
Causes of oxygen starvation
The causes of hypoxia can be external (mechanical) or internal, provoked by dysfunction of organs and systems, as well as pathological processes.
Oxygen deficiency is caused by intoxication with substances that inhibit the stimulation of hemoglobin.
Radiation exposure or toxins released during tissue decay also have a negative impact.
For example, due to severe exhaustion of the body due to prolonged fasting or a dangerous infection. Global blood loss, stress, excessive physical exertion, abuse of alcohol, drugs or smoking are factors that can cause oxygen starvation. Let us dwell in more detail on the main causes of hypoxia.
Carbon monoxide poisoning and inhalation
Carbon monoxide is a blood poison of general toxicity, a colorless, odorless substance that can penetrate any obstacles. A concentration of carbon monoxide in the air greater than 1.2% causes death in less than three minutes. What does carbon monoxide poisoning lead to:
- when inhaled, the transport of oxygen to organs and tissues is blocked, resulting in oxygen deficiency;
- the functions of the heart muscle are similarly impaired.
Causes of poisoning:
- inhalation of exhaust gases from vehicles, prolonged stay in a closed garage or a car with the engine running;
- household poisoning - malfunction of heating appliances (fireplaces, stoves, pipes), leakage of propane gas, soot from kerosene lamps, etc.;
- inhalation during fire.
The outcome of poisoning directly depends on the concentration of carbon monoxide, the condition of the patient, physical activity at the time of inhalation, but most importantly - on the duration of oxygen starvation.
Strong pressure on the throat area
Hypoxia can occur both due to mechanical impact on the trachea and due to the development of internal pathologies.
Factors causing oxygen deficiency:
- asphyxia (suffocation);
- swelling of the mucous membrane of the respiratory tract;
- allergic reaction to food, chemicals, odors, flowers or medications, accompanied by angioedema;
- inflammatory processes in the larynx, for example, inflammation of the tonsils or adenoids.
Diseases that impair the functioning of the respiratory muscles
Dysfunction of the spinal cord leads to paralysis of the respiratory muscles. In this condition, brain cells are incapable of maintaining and regulating gas exchange processes in the lungs.
The following pathologies contribute to the development of paralysis of the respiratory muscles:
- damage to peripheral nerve processes or endings;
- destruction of muscle tissue;
- autoimmune processes;
- drug poisoning.
Genetic dysfunctions associated with muscular dystrophy lead to the death of cells and fibers. It is difficult for a patient with this pathology to breathe, which quite often causes death even in young people.
Consequences
Oxygen deficiency affects the functioning of all organs and systems. The consequences depend on the period in which the pathology was eliminated and how long it lasted. If the compensatory mechanisms have not yet been exhausted, and the oxygen deficiency has been eliminated, then no negative consequences will arise. When the pathology appears during the period of decompensation, complications are determined by the duration of oxygen starvation.
The brain suffers more from this condition, because without oxygen it can only withstand 3-4 minutes. The cells may then die. The liver, kidneys and heart are kept for about 30-40 minutes. The main consequences of oxygen deficiency:
- depletion of adaptation reserves;
- weakening of antitumor protection;
- decreased immunity;
- deterioration of memory and reaction speed;
- neuropsychiatric syndrome;
- psychosis;
- dementia;
- parkinsonism (shaking palsy);
- exercise intolerance;
- fatty degeneration of muscle cells, myocardium, and liver.
Consequences for the child
Oxygen deficiency is one of the common causes of not only fetal mortality, but also the appearance of developmental defects. The consequences depend on the trimester of pregnancy and the degree of oxygen deficiency:
- First trimester. During this period, the laying of organs occurs, therefore, due to oxygen deficiency, a slowdown in the development of the embryo and the formation of anomalies are possible.
- Second trimester. At this stage, problems arise with the baby’s adaptation and pathologies of the central nervous system. In the chronic form, the death of the child is possible.
- Third trimester. Lack of oxygen provokes developmental delays during pregnancy. Serious damage to the baby's nervous system is also possible. During childbirth, oxygen deprivation causes asphyxia.
Consequences of fetal hypoxia in a child after birth
Experiencing oxygen deprivation after the birth of a baby seriously affects his health. The child becomes restless, easily excitable, and suffers from high muscle tone. The latter is expressed in frequent twitching of the legs or arms, convulsions, and trembling of the chin. Other symptoms include lethargy, frequent regurgitation and reluctance to latch on to the breast. A list of more serious consequences includes:
- stillbirth;
- death in the early postpartum period;
- impairment or delay of psychomotor and intellectual development;
- damage to blood vessels and heart;
- diseases of the nervous system;
- problems with the urinary organs;
- severe eye diseases.
Signs
The clinical picture of ischemic syndrome is individual for each patient. It manifests itself depending on the degree and duration of hypoxia. It is worth noting that the prognosis in childhood is favorable in most cases. The central nervous system has regenerative properties, so complications develop only in the last stages.
The diagnosis can be made already in the first minutes of life, especially if the disease manifests itself in a severe form
The severity of the patient's condition is assessed using the Apgar scale. It includes a number of indicators, including pulse and respiration, skin condition, and the severity of reflexes. Thus, brain damage of hypoxic origin can be diagnosed immediately after birth. There are 3 main degrees of the disease, the third of which is the most dangerous.
1st degree
With hypoxic damage to the central nervous system of the first degree, the symptoms are mild. The child’s general condition is assessed at 6–7 points (the optimal result is considered to be 7–10 points). The clinical picture includes the following signs:
- pale, bluish skin;
- deterioration of muscle tone, tremor;
- restless sleep;
- activation or deterioration of reflexes.
First degree injuries do not pose a danger to the patient. Already during the first week of life, all indicators return to normal, and then the child develops on par with peers.
2nd degree
The second degree of brain damage most often occurs during hypoxia both during pregnancy and childbirth. According to the Apgar scale, the child's condition can be assessed as 5 points. The pathological process is manifested by the following symptoms:
- lack of reflexes;
- increase or decrease in muscle tone;
- pronounced cyanosis of the skin and mucous membranes;
- increased intracranial pressure - this indicator continues to increase, manifested by bulging fontanelles, sleep disorders, involuntary muscle movements;
- autonomic disorders, including arrhythmias, slow heart rate, apnea (stopping breathing), problems with the functioning of the digestive tract.
IMPORTANT! In the first days of a child’s life, it is important to monitor intracranial pressure indicators. With timely treatment, the condition can improve by the end of the first week of life; if it is not treated, the disease progresses.
3rd degree
Third degree damage to the central nervous system is a consequence of gestosis in the second half of pregnancy. The child's condition is complicated by abnormal birth. A newborn needs resuscitation measures, since he may have no respiratory activity, and pathologies of the cardiovascular system are pronounced. There are no reflexes, including swallowing, so natural feeding is impossible. Often such patients are diagnosed with renal and liver failure, DIC syndrome (blood clotting pathology).
Causes of oxygen starvation
There are many reasons for lack of oxygen. Quite conventionally, they can be divided into two large groups – external and internal. External causes include all factors that disrupt the supply of oxygen to the human body:
- Low oxygen saturation of the air - due to unfavorable ecology (pollution from smoke, gasoline vapors and other chemicals); with prolonged stay in a cramped or crowded and poorly ventilated room; being in high mountain areas (inhaling rarefied air); carbon monoxide poisoning.
- Impossibility or impaired air flow - in case of asphyxia (suffocation) due to a foreign body in the respiratory tract; in case of drowning; due to narrowing of the airway lumen due to allergic edema (Quincke's edema), an overgrown tumor; paralysis of the respiratory muscles (in case of poisoning with narcotic substances, some poisons and toxins).
- Acute and chronic diseases (most often from the bronchopulmonary system - obstructive bronchitis, pneumonia, bronchial asthma), leading to disruption of the breathing process.
Among the internal causes of hypoxia are the following:
- Chronic diseases of the cardiovascular system, in which both the processes of blood oxygenation in the lungs and the processes of oxygen delivery with blood to organs and tissues are disrupted.
- Anemia, in which the amount of hemoglobin, which carries oxygen, decreases.
- Blood loss from injuries and internal bleeding.
- A discrepancy between the need for oxygen and its supply - for example, with significant oxygen consumption during heavy physical work, during an acute infectious disease - cells require a lot of oxygen for adequate work and recovery, but the body is not able to provide it.
- Tissue hypoxia, which develops in cases where tissues cannot absorb the oxygen supplied to them. This is observed when tissue and cellular enzymes are disrupted during poisoning with certain poisons.
Mechanism of development of hypoxia
The central nervous system is the brain and spinal cord. These structures are able to function normally only with a sufficient supply of oxygen, which is carried by the blood. Infants and young children have a significantly higher oxygen requirement than adults, and oxygen deficiency can cause serious delays in physical and mental development. Damage to the central nervous system of ischemic origin is associated with insufficient blood supply to brain tissue, and therefore there is a gradual death of nerve cells.
Hypoxia is a lack of oxygen in tissues. With perinatal damage, this occurs during pregnancy, during childbirth and in the first days of the child’s life. The condition is reversible, since regeneration processes occur faster at a younger age. Over time, the harmful effects of oxygen starvation can be neutralized and nerve conduction restored. Ischemia is a more dangerous condition. This term implies a complete cessation of oxygen supply to cells, which leads to their rapid necrosis.
Causes
A common cause of oxygen starvation may be a lack of oxygen entering the body or a cessation of its absorption by body tissues. This is facilitated either by unfavorable external factors or certain diseases and conditions. If oxygen starvation develops as a result of a lack of oxygen in the inhaled air, then the form of pathology is called exogenous. Its reasons are:
- staying in wells, mines, submarines or other enclosed spaces that have no communication with the outside environment;
- smog in the city, severe gas pollution;
- poor ventilation;
- malfunction of anesthesia-respiratory equipment;
- being in a room where there are many people;
- thin atmosphere at altitude (pilot illness, mountain and altitude sickness).
If the pathology is the result of any disease or condition of the body, then it is called endogenous. The reasons for this type of oxygen starvation are:
- diseases of the respiratory system, such as asbestosis (deposition of asbestos dust in the lungs), pneumothorax, hemothorax (filling of the pleural cavity with air or blood), bronchospasm, bronchitis, pneumonia;
- the presence of foreign bodies in the bronchi, for example, after accidental ingestion;
- acquired or congenital heart defects;
- fractures and displacements of the chest bones;
- diseases or pathologies of the heart, such as heart attack, heart failure, pericardial obliteration, cardiosclerosis (replacement of the heart muscle with connective tissue);
- injuries, tumors and other brain diseases that damage the respiratory center of the central nervous system;
- venous hyperemia (plethora);
- congestion in the system of the superior or inferior vena cava;
- acute blood loss;
- asphyxia (suffocation) of any nature;
- a sharp narrowing of blood vessels in various organs.
Intrauterine fetal hypoxia
For an unborn baby, oxygen deficiency is very dangerous. It causes serious complications: in the early stages of pregnancy - slowdown or pathology of fetal development, in the late stages - damage to the central nervous system. Oxygen starvation of a child can be caused by some systemic diseases of a pregnant woman, including:
- pathologies of the cardiovascular system, which lead to vascular spasms and deterioration of blood supply to the fetus;
- diseases of internal organs, such as pyelonephritis and inflammation of the urinary system;
- iron deficiency anemia, which interferes with the supply of oxygen to tissues;
- chronic diseases of the respiratory organs, for example, bronchial asthma or asthmatic bronchitis;
- disturbances in the functioning of the endocrine system.
Hypoxia during pregnancy is often associated with a woman’s bad habits. A pregnant woman is strictly prohibited from smoking and drinking alcohol. All toxins enter the baby's bloodstream and lead to serious complications. Fetal hypoxia can also be associated with other disorders:
- abnormalities in the development of the placenta or umbilical cord;
- post-term pregnancy;
- increased uterine tone;
- premature placental abruption;
- infection of the fetus;
- incompatibility of fetal blood with maternal blood according to the Rh factor;
- prolonged compression of the head in the birth canal;
- entwining the umbilical cord around the neck;
- entry into the respiratory tract of mucus or amniotic fluid.
Causes of central nervous system damage
The main cause of the disease is ischemic hypoxia, that is, damage to the cells of the nervous system due to their insufficient blood supply. The type of violation depends on a number of factors, including the duration of oxygen starvation. Thus, during acute hypoxia, the stem parts and subcortical structures are damaged, and during prolonged oxygen deficiency, the cerebral cortex is damaged. The process develops during intrauterine development and immediately after birth, and its causes can be the following factors:
We recommend reading the article: Diseases of the blood vessels of the head
- on the maternal side: various circulatory disorders in the uterus, heavy bleeding, various pathologies of placental development;
- during pregnancy: bad habits, systemic use of certain groups of drugs;
- during childbirth: umbilical cord entanglement, massive blood loss in the mother, low blood pressure and low pulse in the child;
- in the first days of life: heart defects and congenital diseases of the respiratory system, DIC syndrome and other pathologies.
Various pathologies of the cardiovascular system are a trigger for the development of hypoxic-ischemic damage to the central nervous system. A deficiency of oxygen in arterial blood causes a lack of oxygen in the nervous tissue. This is how necrosis (death) of some nerve cells or their groups occurs. In this condition, a decrease in blood pressure provokes a worsening of the situation and can lead to chronicity of the process and irreversible changes. Due to a slowdown in metabolism, acidosis (oxidation) of cells occurs, which causes swelling. Ischemic changes often include increased intracranial pressure, as well as pathologies of internal organs (lungs, kidneys, liver).
REFERENCE! Ischemic-hypoxic damage to the central nervous system refers to irreversible changes in brain tissue caused by insufficient blood supply. Less severe disorders are more often classified as hypoxic-ischemic encephalopathy, but the terms can be used interchangeably.
General manifestations of the disease
When drawing up a clinical picture, the symptoms of oxygen starvation of the brain are accurately determined by the attending physician. This condition is characterized by:
Stage of increased excitability . During diagnosis, slight changes in brain structures are observed, which cause a state of euphoria and uncontrolled behavior. The patient is restlessly agitated and cannot control himself.
Stage of external changes . The patient's skin turns pale, bluish swelling or severe redness appears. At this stage, the brain tries to restore blood circulation, resulting in perspiration on the forehead and cold sweat throughout the body.
Inhibition of the nervous system . Oxygen starvation of the brain is accompanied by severe disturbances in the functioning of the central nervous system. At this stage, the brain structures are significantly damaged, resulting in: severe vomiting, dizziness, and nausea. Vision deteriorates, its clarity is impaired, in some cases, attacks of darkening occur in the eyes, and patients lose consciousness.
Perinatal damage at a severe stage . Brain swelling develops, which leads to a vegetative state: the patient loses all reflexes and may fall into a coma. The sensitivity of the skin and the functioning of all internal organs are impaired.
At all stages except the initial stage, the patient is accompanied by severe weakness and drowsiness.
Chronic oxygen deprivation of the brain leads to frequent headaches and tinnitus
The patient experiences fatigue, morning sickness, problems with concentration and attention, and memory impairment. During diagnosis, disturbances in the functioning of various organs are detected
Symptoms of the hypoxic form
Hypoxic hypoxia of the brain develops with low oxygen supply for a long time without the influence of pathological processes.
This form of pathology appears in people who spend a lot of time in enclosed spaces without access to natural air (bunkers, tanks, submarines). It can be observed in those who spend a long time in high mountains. The condition is often recorded in people who frequently and quickly ascend on airplanes and spacecraft.
Symptoms of hypoxia
Signs of oxygen starvation vary depending on the form of the pathology. During acute hypoxia, patients experience motor and psychoemotional agitation, heartbeat and breathing become more frequent, the skin turns pale, sweating increases, and midges “flash” before the eyes. Gradually the condition changes, the patient calms down, becomes lethargic, sleepy, his eyes darken, and tinnitus appears.
At the next stage, the person loses consciousness, clonic convulsions and chaotic muscle contractions may occur. Movement disorders are accompanied by spastic paralysis, an increase and then a decrease in muscle reflexes. The attack develops very quickly, coma may occur within 1–2 minutes, so the patient needs urgent medical attention.
Chronic brain hypoxia occurs slowly. Characterized by constant fatigue, dizziness, apathy, and depression. Hearing and vision often deteriorate and performance decreases.
Depression is characteristic of brain hypoxia
Neurological signs of hypoxia in adults:
- With diffuse organic damage to the brain, posthypoxic encephalopathy develops, accompanied by visual and speech disorders, impaired coordination of movements, tremor of the limbs, twitching of the eyeballs, etc.
- With partial impairment of consciousness, the symptoms of hypoxia manifest themselves as lethargy, numbness, and stupor. A person is in a depressed state, from which he can be brought out with persistent treatment. Patients retain protective reflexes.
- Asthenic state: increased fatigue, exhaustion, deterioration of intellectual abilities, motor restlessness, low performance.
Brain hypoxia can be fulminant, acute or chronic. In the acute stage, signs of oxygen deficiency develop rapidly, and the chronic disease proceeds, gradually progressing, with less pronounced signs of malaise.
Acute hypoxia is accompanied by cerebral edema and dystrophic changes in neurons. Even after normalization of oxygen delivery to brain cells, degenerative processes persist and progress, leading to the formation of softened lesions. Chronic hypoxia of brain tissue does not cause pronounced changes in nerve cells, therefore, when the causes of the pathology are eliminated, patients recover completely.
Kinds
Brain hypoxia is divided into types according to etiology, time of development and localization.
By etiology
If we take into account external factors, cerebral hypoxia can be divided into the following types:
- Hypoxic, when there is a lack of oxygen directly in the air. Most often this occurs due to poor ventilation of the premises, lack of ventilation in completely enclosed rooms. Climbers experience symptoms of brain hypoxia, because the higher you go, the less oxygen in the air.
- Respiratory, when there is a malfunction of the respiratory system due to diseases or dysfunctions of the respiratory center.
- Cardiovascular, caused by changes in the composition of the blood, which interferes with its normal flow: heart failure, narrowed working channels due to thrombosis, atherosclerosis. Such hypoxia can lead to ischemic stroke of the brain.
- Hemic, associated with changes in the composition of the blood. Oxygen is transported throughout the body by hemoglobin molecules. And if there is a deficiency in it, then oxygen will remain unbound and will not be able to enter the cells.
- Tissue, when the body cannot utilize carbon dioxide from cells. Most often it occurs due to blockage of a fragment of the mitochondrial respiratory chain, provoked by poison or a number of drugs.
- Overload, which is a temporary phenomenon due to excessive load on muscle, nervous tissue or the organ itself.
- Man-made, caused by harmful substances in production, etc.
- Mixed, any hypoxia that led to a tissue type of pathology.
By exposure time
Due to the fact that hypoxia is not a disease, but a condition, the speed of its development is extremely important. There are 3 types of it:
- Lightning fast, developing rapidly, for example, with injury or hemorrhage in the respiratory center. It doesn’t matter whether it happened to an adult or a child, without urgent medical attention the patient will die.
- Acute when it takes a couple of hours to develop, which often happens with cyanide poisoning, which blocks enzymes of the respiratory chain. The time it takes to provide emergency care is in minutes, because the faster it happens, the higher the chance of preserving the health and life of the patient.
- Chronic, not threatening the patient’s life, but significantly worsening its quality. The body uses all mechanisms to independently saturate the brain with oxygen, only to maintain its vital functions, but there will be no full restoration of functions.
By localization
Doctors divide the localization of brain hypoxia into 4 main types:
- Dissipated, when there is a general lack of oxygen in the blood, which leads to disorders of low and moderate severity. At the same time, it has the most favorable prognosis for the patient.
- Central, cerebral, ischemic attack, when the blood supply to a separate area of the brain is disrupted due to thrombosis due to a more extensive pathology.
- A global, cerebral, ischemic attack in which blood does not completely flow to the brain.
- Ischemic stroke, caused by rapid narrowing and/or obstruction of blood flow. With it, several areas will be affected at once.