Ependymoma is a tumor of the central nervous system. Since such neoplasms form directly in the central nervous system, they are also called primary tumors. Ependymomas are more often benign than malignant and are formed due to mutations of ependymal cells. Ependymal cells (ependyma) are thin membrane epithelial cells that line the central canal of the spinal cord and the walls of the ventricles of the brain.
Ependymoma is a fairly rare type of tumor of the brain or spinal cord. Cancerous ependymomas come in different levels of malignancy, and therefore some tumors grow slowly, while others, on the contrary, develop rapidly. As the tumor grows, vital areas of the brain are compressed, and in this case the tumor can threaten the patient’s life. But most often, ependymomas are isolated from the medulla, are characterized by very slow growth and cause the appearance of intracranial hypertension (increased intracranial pressure). With intracranial hypertension, hemorrhage into the ventricles of the brain can occur - ventricular hemotamponade. According to statistics, of all cases of tumor formation in the brain, ependymomas occur in almost 10% of cases.
ICD-10 code:
D-33 – benign neoplasm of the brain and other parts of the central nervous system;
D-43 – neoplasm of uncertain or unknown nature of the brain and central nervous system.
Important! Even a benign tumor can be life-threatening if it compresses areas of the brain that regulate vital body functions. Therefore, if suspicious symptoms appear, you should immediately consult a doctor.
Table of contents
- What are ependymomas?
- Where do ependymomas grow and how do they spread throughout the central nervous system?
- How common are ependymomas in children?
- What are the histological types of ependymomas?
- Why do children get ependymoma?
- What are the symptoms of the disease?
- How is ependymoma diagnosed?
- How is a treatment plan made?
- How is ependymoma treated?
- What protocols and registries are used to treat children?
- What are the chances of being cured from ependymoma?
- Additional Information
Course of therapy
The course of treatment includes two points, namely surgery and radiation therapy. The type of surgery and further course of recovery will depend on the following factors:
- Localization of formation and its size;
- The presence of metastases or damage to neighboring tissues;
- Age of the patient;
- Type of tumor.
Chemotherapy is usually not prescribed for ependymoma, as it does not provide significant results. In rare cases, it is used for relapse.
What are ependymomas?
Ependymomas are tumors of the central nervous system (CNS). They belong to solid tumors [solid tumor] and appear due to mutation of cells [cell] of the brain [brain] or spinal cord [spinal cord]. Because these tumors grow in the central nervous system, they are also called primary CNS tumors. That is, these are not metastases from other malignant tumors that grew in other organs and their cancer cells penetrated into the central nervous system.
Ependymomas come in varying degrees of malignancy. This is why some tumors grow more slowly while others grow quickly. But the outside of the human skull is bordered by bones, and inside there is little room for tissue that continues to grow and which can sometimes put pressure on vital areas of the brain. Therefore, even if ependymoma grows slowly, it can still threaten the child’s life.
Ependymoma of the brain
Experts have discovered the SV40 virus, which is localized in ependymoma cells that are in an active state. But the role of this virus in tumor development is still unclear today.
There are suggestions that anaplastic ependymoma of the brain is caused by exposure to oncogenic factors that are common to other types of tumors. This includes radioactive radiation, chemical carcinogens, oncogenic viruses, etc. The involvement of a genetic factor cannot be ruled out.
Where do ependymomas grow and how do they spread throughout the central nervous system?
Ependymomas arise from mutated ependymal cells. Ependymal cells or ependymocytes are the cells that line the inside of the ventricles of the brain and the spinal canal. That is why this type of tumor grows inside the ventricular system of the brain and in the spinal canal.
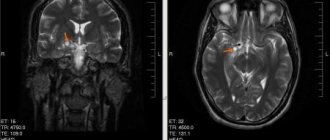
Most often (about 60%), doctors find ependymomas in the fourth ventricle in the posterior cranial fossa [posterior cranial fossa]. From there they often grow into the cerebellum, the brain stem, and the upper cervical spinal cord. Experts call this tumor growth infratentorial.
About 30% of ependymomas are located in the region of the lateral ventricles of the cerebrum [cerebrum] and in the region of the third ventricle in the diencephalon [diencephalon]. Experts call this tumor growth supratentorial. 10% of ependymomas grow in the spinal canal. Experts call this type of tumor growth intraspinal.
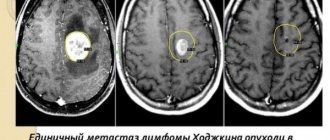
In less than 5% of children with ependymoma in the cerebral region or in the posterior cranial fossa (WHO classification of II and III degrees of malignancy), at the time of diagnosis, specialists find metastases in the central nervous system. And metastasis outside the central nervous system, for example, in the lungs and/or lymph nodes [lymph nodes], is extremely rare.
Treatment of ependymoma
Treatment of this tumor can be complex, surgical and radiation. The most optimal treatment option is its total destruction. When the tumor is located in the posterior cranial fossa, this causes certain difficulties for the neurosurgeon, which are associated with convenient access. If it is not possible to completely remove the tumor, then the operation is palliative.
In this case, shunt surgery can be used to improve the outflow of cerebrospinal fluid. To keep the recurrence rate of ependymoma to a minimum, after surgery the patient undergoes radiation therapy. If we are talking about surgery in young children, when the brain is still very vulnerable to radioactive radiation, radiation therapy should be greatly reduced or completely replaced with chemotherapy. The use of cytostatics is possible either instead of radiation therapy, or after it. The volume directly depends on the nature of the tumor, as well as its prevalence.
To destroy a tumor in an adult patient, stereotactic radiosurgery can be used. As practice shows, greater efficiency is ensured by the “Cyber Knife” installation, which, with the help of numerous beams that emanate from different points of the device, strongly irradiates the ependymoma and destroys it. This method is not recommended for use on children under 14 years of age, since the radiation exposure is quite high.
Subepindymoma or myxopapillary ependymoma after radical removal generally has a favorable prognosis. It is in this case that ependymoma is observed without relapse. As for the classic type, it is not always possible to completely remove it. Recurrence usually occurs at the site where the tumor originally appeared. If the removal was successful, the 5-year survival rate is estimated at up to 80%.
Is there a cure for a brain tumor?
The most unfavorable prognosis is observed in the situation with anaplastic ependymoma, which is associated with its very rapid spread along the cerebrospinal fluid pathways. It is worth noting that if the ependymoma has been completely removed, cured people may complain of neurological symptoms, which are expressed by deterioration of vision and hearing. In the case of children, they are at high risk of exhibiting mental retardation.
How common are ependymomas in children?
Ependymomas are very rare tumors. In the group of diseases that experts call “primary tumors of the central nervous system,” they make up only about 10%. Children can get this type of cancer at any age. But most often this type of tumor occurs in children under the age of 3-4 years. The average age of children when they are diagnosed with ependymoma is about 6 years.
In Germany, between 35 and 45 new cases of ependymoma in children and adolescents are reported annually. In other words, out of 1,000,000 children, approximately 3 people get sick. Boys get sick slightly more often than girls (ratio: 1.2:1).
Causes of occurrence and development
The causes and development of ependyoma are not fully known. Every body contains cancer cells. If a person is completely healthy and his immune system is in perfect order, then the cells are in a dormant state.
Stress or nervous strain in adults can lead to awakening and provoke the development of a tumor. Most often, ependyoma occurs in young children and the cause may be heredity or improper functioning of the immune system - an endogenous factor.
What are the histological types of ependymomas?
The properties of tumor tissue in ependymomas are very diverse. That is, ependymomas within themselves differ in the structure of the tumor tissue (experts talk about the histological variant of the tissue). There are low-grade ependymomas. This means that their cells divide slowly, and the tumor itself grows slowly. Cells of ependymomas of higher degrees of malignancy divide very quickly, the tumors themselves have different qualities and they grow aggressively.
The World Health Organization (WHO) divides ependymomas according to their histological tissue structure into the following types (WHO classification):
- Subependymomas, WHO grade I: low-grade tumors that grow slowly.
- Myxopapillary ependymomas, WHO grade I: tumors of low malignancy, grow slowly, most often appear in the spinal canal.
- WHO grade II ependymomas: usually grow slowly, with a slight tendency to grow aggressively. Depending on how most cancer cells look under a microscope, they will be divided into several variants within the group.
- Anaplastic ependymomas of WHO grade III: these are tumors that have all the signs of aggressive growth.
It is impossible to draw an exact boundary between grade II and grade III ependymomas based solely on histological analysis of the tumor tissue. Therefore, it is impossible to say in advance whether the tumor is grade II or grade III. Only by observing how the tumor actually grows can we talk about its degree of malignancy.
What diseases have symptoms similar to cerebral ependymoma?
Medulloblastoma:
- Originates in the cerebellum
— Differential diagnosis can be difficult, since medulloblastomas vary in the degree of accumulation of CS and give multiple small metastases in the CSF
Glioblastoma:
— As a rule, pronounced perifocal edema
-Acute onset, usually with a seizure
-Increased ORC, 2-3 times higher than normal
Pilocytic astrocytoma:
— Usually one-sided asymmetrical ring with visible contrast enhancement
- Not adjacent to the ventricular system
Epidermoid cyst:
— Hypointense on T1-WI
— Does not accumulate CS
— Marked restriction of diffusion
What are the symptoms of the disease?
Just like other brain tumors, the symptoms of ependymoma depend primarily on the age of the child, where exactly in the central nervous system [CNS] the tumor grew and how far it has already spread throughout the body. At the same time, experts talk about general symptoms (nonspecific) and local symptoms of the disease (specific).
Nonspecific general symptoms appear regardless of where exactly the tumor has grown. In general, these symptoms also appear in other diseases that are not related to CNS tumors. For example, a child has a headache and/or back pain, dizziness, loss of appetite, vomiting on an empty stomach in the morning, the child loses weight, begins to get tired faster, his performance decreases, concentration is lost, the child’s personal characteristics change, his behavior changes, there are delays in development.
These symptoms appear when pressure gradually builds up inside the skull and puts pressure on the brain structures. The tumor itself, which is growing, can compress, and/or due to the tumor (as, for example, with medulloblastoma), the circulation and outflow of cerebrospinal fluid (CSF, cerebrospinal fluid) is disrupted. Due to a violation of the outflow of cerebrospinal fluid, the child may develop water on the brain (hydrocephalus). If dropsy appears in infants and young children, when the fontanelles have not yet closed, then their head greatly increases in volume (macrocephaly).
Specific symptoms may indicate where exactly the tumor has grown in the central nervous system and which control centers it is disrupting. For example, if an ependymoma has grown in the cerebellum area, the child’s gait and balance may be impaired. If a tumor grows in the cerebrum, then the child experiences seizures, and if it grows in the spinal cord, then some part of the body is paralyzed in children. If a child has problems with vision, consciousness, or sleep, this may also indicate where the tumor has grown (although these symptoms are often less informative).
Signs of the disease
When the tumor expands, the following symptoms appear:
- progressive pain in the head;
- feeling of pressure on the eyes;
- nausea and vomiting, independent of food intake;
- irritability, behavioral changes;
- loss of coordination control, unsteadiness of gait;
- violations of fine motor skills (the patient loses the ability to write accurately and quickly);
- decreased level of memorability;
- impairment of auditory (hearing loss) and visual perception (double vision).
With subsequent growth of ependymoma, the cerebrospinal fluid channels may become blocked, hydrocephalus develops, internal pressure increases, and the described symptoms tend to worsen. The pain syndrome increases in intensity and is not relieved even by strong analgesics; vomiting does not stop and does not bring relief. Systematic seizures are often found in the pediatric clinical picture.
How is ependymoma diagnosed?
If the child’s medical history (history) and the results of an external examination [external examination] give the pediatrician a suspicion of a malignant tumor in the central nervous system, then the doctor refers him to a clinic that specializes in pediatric and adolescent oncology (clinic of pediatric oncology and hematology).
Because if such a tumor is suspected, then a full examination is carried out by specialists of various profiles. First, they must confirm the diagnosis of whether the child actually has a malignant tumor of the central nervous system [CNS tumors]. Secondly, if the diagnosis is confirmed, they must say what specific type of tumor the child has and how far the disease has spread throughout the body. Only by answering these questions can we optimally plan treatment tactics and give a prognosis.
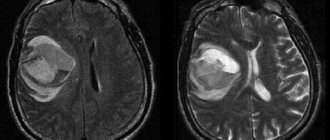
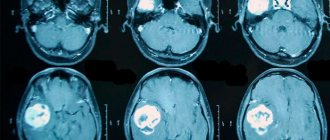
To make an accurate diagnosis of whether a child has ependymoma, they carefully study the medical history again, conduct an external examination and a neurological [neurological] examination. Then, imaging studies such as magnetic resonance imaging (MRI) and, less commonly, computed tomography are prescribed. Using these methods, you can accurately say whether a child has a tumor, or perhaps metastases in the brain and spinal canal. In the pictures you can see exactly where the tumor has grown, what size it is, where the borders of the tumor with neighboring structures are. They can also be used to accurately see whether the child has hydrocele.
To definitively confirm the diagnosis, a sample of tumor tissue is taken (biopsy) and examined under a microscope. Depending on the type of cancer and the patient's specific situation, additional examinations may be prescribed.
In recent years, the number of histological studies has increased sharply. The information obtained from their results allows for a more accurate diagnosis. Some specific characteristics of the tumor that specialists see can predict the likely course of the disease (for example, how the tumor will grow). In the future, these histological features are expected to have implications for treatment decisions.
Depending on the specific form of the disease and the individual situation of the patient, additional studies and tests may be prescribed.
Diagnostics
To diagnose ependymoma, you first need to consult a neurologist. The anamnesis is studied in detail, a comprehensive examination is carried out and reflexes are checked. After this, tests and studies are prescribed, such as:
- MRI is especially informative when examining the brain. The images help clarify the size, structure and shape of the tumor and determine the condition of the blood vessels. MRI is safe for children due to the absence of radiation;
- CT scan – identifies the focus of pathology and examines other organs for the presence of metastases;
- electroencephalography – examines the functional state of the brain;
- ophthalmoscopy - the fundus of the eye is examined, the condition of the optic nerve, retina, and choroid is assessed;
- neurosonography - ultrasound examination of the brain in newborns, carried out through the large fontanelle if brain pathology is suspected;
- angiography - examination of blood vessels using a contrast agent;
- lumbar puncture - a study by puncturing the lower back to collect cerebrospinal fluid;
- Ultrasound – helps determine symptoms of displacement of the midline structures of the brain;
- stereotactic biopsy is a surgical intervention to obtain fragments of tumor tissue for histological examination.
When diagnosing, ependymoma must be differentiated from subependymal astrocytoma (the most common tumor in the brain, a type of glioma) and neuroma (a benign tumor localized in the cauda equina region).
Don't waste your time searching for inaccurate cancer treatment prices
*Only upon receipt of information about the patient’s disease, a representative of the clinic will be able to calculate the exact price for treatment.
How is a treatment plan made?
After the final diagnosis, a treatment plan is drawn up. In order to create the most individualized treatment program specifically tailored for a specific patient (risk-adapted therapy), the treating team must take into account certain factors that affect the patient’s prognosis (so-called prognostic factors or risk factors).
Important prognostic factors in children with ependymoma are the specific type of tumor, where exactly it grew, how far it has spread, and whether it has metastasized. Doctors receive this information after a complete diagnosis, which we discussed above. In addition, the age of the child and the general state of his health matter. When drawing up an individual treatment plan, specialists take into account all these factors in order to obtain the most effective treatment result.
Diagnosis of the disease
When a patient experiences severe liquor-hypertensive syndrome or an epileptic seizure that occurs for the first time, he is immediately sent for an MRI or CT scan of the brain. The first option is more effective, as it allows the specialist to obtain more detailed information and also eliminate radiation exposure to the patient, especially if we are talking about a child.
If we are talking about the primary diagnosis of a child under one year old, then the preferred option is neurosonography, which is carried out through a fontanel that has not yet closed.
The patient may additionally be referred for electroencephalography, and also undergoes a consultation with an ophthalmologist, who will refer for direct ophthalmoscopy. To determine the extent of the tumor development process, a lumbar puncture is used, and cerebrospinal fluid is also examined. A complete diagnosis can only be obtained after a morphological study of the ependymoma material, which is obtained by stereotactic biopsy.
In addition to the options listed, the following studies may be required:
- Ultrasound;
- Vision assessment;
- Skin sensitivity;
- Diagnosis of reflex function;
- Neurological tests.
How is ependymoma treated?
Children with ependymoma should only be treated by doctors from children's clinics specializing in pediatric oncology. It is there that highly qualified specialists (doctors, nurses) with a specialization in pediatric oncology work and are proficient in modern therapy programs.
In these hospitals, doctors of different specialties belong to different working groups, which are constantly in close contact with each other. Together they create treatment plans, discuss and manage their patients. Therapy programs are regularly improved. Their goal is to treat the child as gently as possible, that is, with minimal side complications and long-term consequences.
Treatment for children and adolescents with ependymoma consists of surgery (to remove the tumor itself), radiation therapy , and most children also receive courses of chemotherapy . For younger children, chemotherapy is given before radiation to buy more time before radiation therapy sessions begin.
Operation
In the treatment of children with ependymoma, surgery (surgery to remove the tumor) is most important. As practice shows, the result of the operation has a direct impact on the further course of the disease. If it was possible to remove the tumor completely, then children, as a rule, have a more favorable prognosis for the disease than those children in whom the tumor could not be completely removed (by the time of the operation the ependymoma had already grown).
If during the initial operation it was impossible to remove the tumor completely, then doctors try to perform a second operation (sometimes before the start of treatment, sometimes during treatment). But repeated surgery is possible only if the negative consequences of the operation and the risks of complications from it are acceptable.
Some types of ependymomas cannot be completely removed due to the fact that they are located in a very difficult to reach place. This is especially true for those tumors that have grown in the fourth ventricle [ventricles of the brain] and in the cerebellopontine angle [cerebellopontine angle]. Very often these ependymomas cannot be completely removed. If specialists were to completely remove them, the risks would increase enormously that healthy brain tissue, which is responsible for vital processes, would be damaged during the operation.
How to treat after surgery
After surgery, most children receive radiation therapy [radiotherapy] and courses of chemotherapy [chemotherapy]. How exactly the child will be treated further depends, first of all, on what type of ependymoma he has, and what part of the tumor was removed during surgery.
Bei der Chemotherapie werden zellwachstumshemmenden Medikamenten (Zytostatika) verabreicht, die darauf abzielen, Krebszellen in ihrem Wachstum zu stoppen oder zu vernichten. Eine Strahlentherapie erfolgt mit energiereichen, elektromagnetischen Strahlen, die von außen durch die Haut auf die betroffene Region eingestrahlt werden. Sie verursachen Schäden im Erbgut der Tumorzellen und führen dadurch zu deren Absterben.
Ependymomas of grade I malignancy
Children with grade I ependymoma, in whom the neurosurgeon has completely removed the tumor, are usually not treated further. But the attending physicians draw up a plan for when the child should come for a follow-up examination. At regular intervals, specialists examine the body and take control photographs.
Ependymomas of II and III degrees of malignancy:
For tumors of such grades of malignancy, such as ependymoma grade II (WHO classification) or anaplastic ependymoma grade III, treating only the visible tumor is not enough.
That is, even if these types of tumors were completely removed during surgery, doctors always assume that tiny remnants of ependymoma remain in the body. This is why in children with these types of tumors, the likelihood that the tumor will grow again later increases in the area where the tumor originally grew (in this case, experts talk about a local relapse). In children with these forms of ependymomas, there is (albeit less often) a return of the disease (relapse) in other areas of the brain distant from the site of initial growth, or in the spinal cord.
This is why it is necessary to continue non-surgical treatment after surgery. This may include radiation therapy and, if required for a specific situation, chemotherapy. The remainder of the tumor, or the entire region where the tumor grew, is irradiated so that the child does not have a recurrence of the disease later. If additional courses of chemotherapy are carried out, their goal is also to reduce the risks of late relapse.
Good to know: what form of non-surgical treatment will be carried out after the operation depends, first of all, on what type of ependymoma the child has, how far the tumor has managed to metastasize, to what extent the tumor was removed during the operation, as well as on the age of the child at that time. the moment he was diagnosed.
Types of ependymoma
- Subependymoma is a benign tumor that develops slowly;
- Myxopapillary – benign tumor;
- Anaplastic ependymoma is characterized by a malignant nature and is a second-degree cancer;
- Malignant anaplastic ependymoma grade 3.
The grade indicates the level of activity of the tumor, as well as its severity. The prognosis is influenced not only by the degree of the tumor, but also by its location, since some tumors may be located in places that are very difficult to reach for surgical intervention.
Do you trust doctors and their prescriptions?
Yes
18.35%
No
13.67%
I trust, but I check all medications for reviews on the Internet from people who have already tried them and only then do I start taking them.
51.08%
Yes, but only to appointments and doctors from paid clinics.
16.91%
Votes: 278
What protocols and registries are used to treat children?
In Germany, almost all children and adolescents with ependymoma or recurrence of these types of tumors are treated according to standardized protocols called therapy optimization studies and treatment registries.
German protocols, or therapy optimization studies, are clinical studies and are strictly controlled. Their goal is to treat sick children using the most modern developments. At the same time, these studies provide an opportunity to improve treatment approaches and thereby achieve progress in treatment.
Children who are not treated according to the research protocol (for example, if at the time of illness the old protocol was closed and a new one has not yet opened; or if the form of the child’s illness does not meet the criteria described for admission to the current protocol), go through treatment registries . Treatment registries are created and operate in order to advise all patients from modern scientific positions. To ensure high quality of treatment, the research team for a particular protocol typically develops detailed therapeutic recommendations. And when attending physicians contact them, they advise them on choosing the optimal therapy for each individual child.
In Germany, at the end of 2011, the long-term protocol HIT 2000 (study of optimization of therapy for children and adolescents with ependymoma) completed its work. Numerous children's clinics throughout Germany and Austria have used this protocol. SIOP Ependymoma II protocol, is currently under development . The new protocol should begin work in 2015. Then sick children from Germany will be taken for treatment under this protocol.
Currently in Germany they work according to the following protocols and registers:
- HIT 2000 Interim Registry (abbreviated as I-HIT-MED): Children with ependymoma who are currently or in the future unable to be treated under a clinical trial protocol, or who refuse to be treated as required by a clinical trial, are enrolled in a therapeutic registry (HIT 2000 Interim Register). / register I-HIT-MED). These children receive an individual treatment plan, that is, depending on the specific form of the disease. Therefore, experts have drawn up therapeutic recommendations, based on the HIT 2000 protocol. These therapeutic recommendations can be used by all doctors in Germany. The registry is managed by the research office HIT-MED, which is located in the pediatric clinic at the University Hospital of Hamburg (the head of the research group is Prof. Dr. Stefan Rutkowski).
- HIT-REZ 2005 protocol: Another treatment optimization study is the HIT-REZ 2005 protocol (part of the E-HIT-REZ 2005 trial), which treats children with recurrent ependymoma. The central research office is located at the Center for Pediatric and Adolescent Medicine at the University Hospital Essen (headed by Prof. Dr. Gudrun Fleischhak). Please note: this protocol no longer accepts new patients as of January 1, 2013. New patients with relapse are treated according to the therapeutic recommendations developed by the central research office. These recommendations are based on the E-HIT-REZ 2005 protocol. A therapeutic registry should be opened for these children in the near future.
Symptoms when the pathology is located in the area of the 4th ventricle
This anaplastic ependymoma is distinguished by symptoms such as:
- Impaired functioning of the vestibular apparatus and coordination of the patient's movements.
- Constant migraines, manifesting themselves throughout the entire day, aggravated by coughing, changes in body position, and physical activity.
- The presence of difficulties and limitations when performing head movements.
- Sleep disorders.
- Dizziness.
- The urge to nausea and vomiting, which occurs with increased pressure inside the skull or severe migraines.
- General weakness.
- Muscle tremors, cramps.
- Weight loss.
- Loss of consciousness.
- Loss of vision.
Note! Changes in heart rate, increased blood pressure and difficulty breathing can occur if there is a displacement of the brain structures.
What are the chances of being cured from ependymoma?
The chances of recovery depend to a very large extent on how much of the tumor could be removed during surgery.
In children and adolescents who have the entire tumor removed during surgery and then irradiated to the tumor region, survival rates reach 60 to 75% five years after the end of treatment. 10 years after the end of treatment, medical statistics give figures from 50 to 60%, if the disease did not continue to grow. If the tumor could not be completely removed and the child also received radiation to the tumor region, then medical statistics on 10-year survival rate indicate only 30 to 40% of cured children.
If the disease returns, that is, the child experiences a relapse of ependymoma, then specialists, as a rule, once again check whether it is possible to undergo a new operation and radiation. Practice shows that today a new special irradiation technique is available (more precisely, radiosurgical irradiation, or stereotactic radiosurgery [stereotactic method]), which can prolong life time. In addition, recurrent ependymomas are sensitive to chemotherapy drugs. Therefore, this form of treatment can also improve the prognosis of children and adolescents with recurrent ependymoma.
A necessary note: when in the text we give figures on the survival rate of children with ependymoma, we present only statistics. Data from statistics accurately and reliably describe in numbers all children and adolescents with this type of brain tumor. But no statistics can predict whether a particular child will recover or not.
When we talk about recovery, here this term must first of all be understood as “absence of a tumor.” Because modern treatment methods, although they can save a child from a malignant tumor, are usually associated with unwanted complications and late consequences. Therefore, doctors usually monitor all children for a long time after treatment. If necessary, children undergo intensive rehabilitation [rehabilitation].
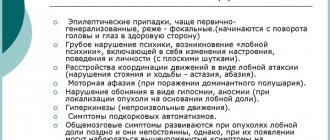
Symptoms
The main feature of brain tumors is that they are localized in a very limited cavity of the brain, which is why sooner or later the tumor begins to affect both adjacent and distant parts of the brain.
Pituitary prolactinoma: symptoms in women
Destruction or compression of tissue under the influence of tumor enlargement leads to the appearance of primary symptoms. During the active development of the tumor, general cerebral symptoms may appear, which were caused by cerebral edema, generalization of hemodynamic disorders, etc. If the tumor is located in the so-called “silent” area, then there may be no symptoms, and the disease itself will begin with general cerebral signs. In this case, focal manifestations may be absent altogether.
The main general cerebral symptom is headache, but this can also be a focal symptom, which is associated with the dura mater of the brain. Vomiting, which is a cerebral manifestation, is more common. With pituitary adenomas, visual disturbances are often observed.
Disorders of the functions of the cranial nerves also appear - loss of smell, pain or complete numbness of the face, hearing loss, disturbances in the digestive system, imbalance, etc.
As for focal symptoms, much depends on the location of the tumor and the affected areas. Movement disturbances, disturbances in the psyche and thought processes, visual disturbances, hormonal disturbances, impaired coordination, etc. may be observed.
Additional Information
The text with which you have become acquainted is compiled on the basis of the modern literature, the list of which is given below. We also took into account modern therapeutic guidelines and recommendations for the treatment of children and adolescents with ependymoma, which were developed by the central research office of HIT-MED. For now, more detailed information about ependymoma can be found on our website www.kinderkrebsinfo.de in German only. If you still have questions, you can always discuss them with your attending physicians.
Bibliography:
- Timmermann B: Die Protonentherapie. Chancen zur besseren Verträglichkeit der Tumorbestrahlung bei Kindern. Wir 2010, 1: 33 [URI: https://www.kinderkrebsstiftung.de/ servicenavigation/ presse/ zeitschriften/ wir/ wir-einzelansicht/ article/ zeitschrift-wir-12010.html] TIM2010
- Kaatsch P, Spix C: Registry - Annual Report 2008 (Jahresbericht 2008 des Deutschen Kinderkrebsregisters). Technischer Bericht, Universität Mainz 2008 [URI: https://www.kinderkrebsregister.de/ extern/ veroeffentlichungen/ jahresberichte/ jb2008/ index.html] KAA2008a
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P: The 2007 WHO classification of tumors of the central nervous system. Acta neuropathologica 2007, 114: 97 [PMID: 17618441] LOU2007
- Kühl J, Korinthenberg R: ZNS-Tumoren. In: Gadner H, Gaedicke G, Niemeyer CH, Ritter J (Hrsg.): Pädiatrische Hämatologie und Onkologie. Springer-Verlag 2006, 777 [ISBN: 3540037020] KUE2006
- Timmermann B, Kortmann RD, Kühl J, Rutkowski S, Dieckmann K, Meisner C, Bamberg M: Role of radiotherapy in anaplastic ependymoma in children under age of 3 years: results of the prospective German brain tumor trials HIT-SKK 87 and 92. Radiotherapy and oncology 2005, 77: 278 [PMID: 16300848] TIM2005
- Gutjahr P: Tumoren des Zentralnervensystems, in: Gutjahr P (Hrsg.): Krebs bei Kindern und Jugendlichen. Deutscher Ärzte-Verlag Köln 5. Aufl. 2004, 373 [ISBN: 3769104285] GUT2004a
- Timmermann B: Therapie von Ependymomen im Kindesalter - Eine aktuelle Übersicht. WIR Informationsschrift der Aktion für krebskranke Kinder eV (Bonn) 2002, 4: 21 [URI: https://www.kinderkrebsstiftung.de/ fileadmin/ KKS/ files/ zeitschriftWIR/ 2002_4/ behandlungsnetzwerk08.pdf] TIM2002a
- Kaatsch P, Rickert C, Kühl J, Schuz J, Michaelis J: Population-based epidemiologic data on brain tumors in German children. Cancer 2001, 92: 3155 [PMID: 11753995] KAA2001
- Timmermann B, Kortmann R, Kühl J, Meisner C, Bamberg M: Combined postoperative irradiation and chemotherapy for anaplastic ependymomas in childhood: results of the German prospective trials HIT 88/89 and HIT 91. Int J Radiat Oncol Biol Phys 2000, 46: 287 [PMID: 10661334]TIM2000
Ependymomas (summary in PDF format) (350KB)