You are viewing the section Ischemic stroke , located in the large section Stroke Subsection: Hemorrhagic stroke
In medicine, there are two types of stroke - ischemic and hemorrhagic.
In this article we will talk about ischemic attack.
The branch of medicine neurology studies this disease.
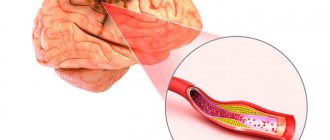
The definition of ischemic cerebral stroke is a condition in which cerebral blood flow decreases or stops, causing a cerebral infarction.
The main cause of the disease is atherosclerosis, in which the vessels supplying blood to the brain are damaged. Atherosclerosis is often combined with hypertension. Acute ischemic stroke requires urgent hospitalization, adequate diagnosis and treatment.
Description
Stroke is an acute disorder of cerebral circulation, characterized by the sudden (within minutes, hours) appearance of focal and/or cerebral neurological symptoms, which persist for more than 24 hours or lead to the death of the patient in a shorter period of time due to cerebrovascular pathology. Vascular diseases of the brain occupy second place in the structure of mortality from diseases of the circulatory system after coronary heart disease. Occurs more often in older people.
I63.9 Cerebral infarction, unspecified
Description of the disease
An ischemic stroke occurs due to obstructions in the vessels that supply blood to the brain. Such obstacles can be fatty deposits and blood clots. The disease is based on 3 pathologies associated with circulatory disorders - ischemia, stroke, and heart attack.
Reference: ischemia is the insufficiency of blood supply to an area of tissue or organ, and stroke is the death of brain tissue due to impaired blood flow due to ischemia or rupture of blood vessels.
Classification
Strokes are divided into 2 large groups: ischemic and hemorrhagic. Depending on the etiology, the former can be cardioembolic (occlusion is caused by a blood clot formed in the heart), atherothrombotic (occlusion is caused by elements of an atherosclerotic plaque) and hemodynamic (caused by vascular spasm). In addition, lacunar cerebral infarction, caused by blockage of a small-caliber cerebral artery, and minor stroke with complete regression of the resulting neurological symptoms within a period of up to 21 days from the moment of the vascular accident are distinguished. Hemorrhagic stroke is classified into parenchymal hemorrhage (bleeding into the substance of the brain), subarachnoid hemorrhage (bleeding into the subarachnoid space of the cerebral membranes), hemorrhage into the ventricles of the brain and mixed (parenchymal-ventricular, subarachnoid-parenchymal). The most severe course is hemorrhagic stroke with blood breaking into the ventricles.
ISCHEMIC STROKE
ISCHEMIC STROKE med.
Ischemic stroke is a stroke caused by the cessation or significant reduction of blood supply to an area of the brain.
Etiology
Based on thrombosis and embolism
• Cardiogenic embolus. The most common cause of embolic stroke is atrial fibrillation.
• Acute stage of MI, dilated cardiomyopathy, prosthetic heart valve, infectious and non-bacterial thromboendocarditis, left atrial myxoma, atrial septal aneurysm, mitral valve prolapse
• Atrial septal defect predisposes to the development of paradoxical embolism, especially in venous thrombosis
• Atherosclerosis of the aorta and carotid arteries
• Drug abuse
• Conditions accompanied by increased blood clotting
• Vasculitis
• Infectious lesions of the central nervous system, including conditions associated with HIV infection
• Disturbance of homocysteine metabolism
• Familial pathology (for example, neurofibromatosis and Hippe-la-Lindau disease).
Clinical picture
Depending on how long the neurological defect persists, transient cerebral ischemia or transient ischemic attacks (complete recovery within 24 hours), minor stroke (complete recovery within 1 week) and completed stroke (deficiency persisting for more than 1 week) are distinguished.
• With embolism, neurological disorders usually develop suddenly and immediately reach maximum severity; Stroke may be preceded by attacks of transient cerebral ischemia.
• With thrombotic strokes, neurological symptoms usually increase gradually or stepwise (in the form of a series of acute episodes) over several hours or days (progressive stroke); periodic improvements and deteriorations of the condition are possible.
• Circulatory disorders in the entire basin of the middle cerebral artery - contralateral hemiplegia and hemianesthesia, contralateral homonymous hemianopsia with contralateral gaze paresis, motor aphasia (Braque's aphasia), sensory aphasia (Wernicke).
• Occlusion of the anterior cerebral artery - paralysis of the contralateral leg, contralateral grasp reflex, spasticity with involuntary resistance to passive movements, abulia, abasia, perseveration and urinary incontinence.
• Impaired blood flow in the posterior cerebral artery - a combination of contralateral homonymous hemianopsia, amnesia, dyslexia, color amnestic aphasia, mild contralateral hemiparesis, contralateral hemianesthesia; damage to the oculomotor nerve, contralateral involuntary movements, contralateral hemiplegia or ataxia.
• Occlusion of the branches of the basilar artery - ataxia, gaze paresis on the same side, hemiplegia and hemianesthesia on the opposite side, internuclear ophthalmoplegia, nystagmus, dizziness, nausea and vomiting, tinnitus and hearing loss up to its loss.
• Signs of cardiogenic embolic stroke
• Acute onset
• Pathological condition of the heart predisposing to embolism
• Strokes in various vascular territories, hemorrhagic infarctions, systemic embolism
• Absence of other pathological conditions causing stroke
• Angiographically detectable (potentially transient) vascular occlusion in the absence of significant cerebral vasculopathy.
Research methods
Treatment:
Lead tactics
• Emergency treatment is necessary because patients are often delivered in a comatose state. The main factor influencing the prognosis of the disease is the timing of the start of treatment.
• Ensuring airway patency, mechanical ventilation
• Infusion therapy
• Administration of glucocorticoids may be dangerous.
• Correction of concomitant cardiac and respiratory failure is necessary
• Barbiturates and sedatives are contraindicated due to possible depression of the respiratory center
• Thrombolytic agents
• The advisability of prescribing anticoagulants depends on the duration of the disease
• It is necessary to start breathing exercises and physical therapy (exercises for paralyzed limbs) as early as possible.
Drug therapy
• Thrombolytic agents: streptokinase - in the early stages of ischemic stroke.
• Anticoagulants
• Heparin. It is most advisable to prescribe in the early stages of the disease. If a clinical picture of neurological deficit has developed against the background of arterial hypertension, heparin is not recommended to be prescribed, because it increases the likelihood of hemorrhages in the brain and other organs. Prescribed for the prevention of recurrent cardiogenic embolism
• Indirect anticoagulants (eg neo-dicoumarin).
• Antiplatelet agents
• Aspirin (acetylsalicylic acid)
• To reduce cerebral edema - mannitol, glycerin.
• Symptomatic therapy.
Surgery
Carotid endarterectomy for severe (70% or more) clinically manifested stenosis of the carotid arteries. Currently, with asymptomatic disease, the dominant trend is toward conservative treatment.
Forecast
• 20% of patients die in hospital, mortality increases with age
• The prognosis is unfavorable if the clinical picture includes episodes of depression of consciousness, mental
disorientation, aphasia and brainstem disorders
• The speed and degree of recovery of neurological functions depend on the patient’s age, the presence of concomitant diseases, as well as the location and size of the affected area
• Complete restoration of function is rare, but the earlier treatment is started, the better the prognosis
• Functional restoration is most active in the first 6 months; After this period, further recovery usually does not occur. See also Stroke. Hemorrhagic stroke. Lacunar stroke. Rehabilitation after stroke
Symptoms
Stroke includes cerebral infarction, cerebral hemorrhage and subarachnoid hemorrhage, which have etiopathogenetic and clinical differences. Taking into account the time of regression of neurological deficit, transient cerebrovascular accidents (neurological deficit regresses within 24 hours, unlike the stroke itself) and minor stroke (neurological deficit regresses within three weeks after the onset of the disease) are especially distinguished. The clinical picture of a stroke consists of general cerebral, meningeal (meningeal) and focal symptoms. Characterized by acute manifestation and rapid clinical progression. Typically, ischemic stroke develops more slowly than hemorrhagic stroke. From the onset of the disease, focal manifestations come to the fore; cerebral symptoms, as a rule, are mild or moderately expressed; meningeal symptoms are often absent. Hemorrhagic stroke develops more rapidly, debuting with general cerebral manifestations, against the background of which focal symptoms appear and progressively increase. In the case of subarachnoid hemorrhage, a meningeal symptom complex is typical. General cerebral symptoms include headache, vomiting and nausea, disturbance of consciousness (stupor, stupor, coma). About 1 in 10 patients with hemorrhagic stroke have a seizure. An increase in cerebral edema or the volume of blood spilled during a hemorrhagic stroke leads to severe intracranial hypertension, mass effect and threatens the development of dislocation syndrome with compression of the brain stem. Focal manifestations depend on the location of the stroke. With a stroke in the carotid artery basin, central hemiparesis/hemiplegia occurs - a decrease/complete loss of muscle strength in the limbs of one side of the body, accompanied by an increase in muscle tone and the appearance of pathological foot signs. In the ipsilateral limbs of the face, paresis of the facial muscles develops, which is manifested by facial distortion, drooping of the corner of the mouth, smoothing of the nasolabial fold, and logophthalmos; when you try to smile or raise your eyebrows, the affected side of the face lags behind the healthy one or remains completely motionless. These motor changes occur in the limbs and half of the face on the side contralateral to the lesion. Sensitivity decreases/losses in these same limbs. Possible homonymous hemianopsia - loss of the same halves of the visual fields of both eyes. In some cases, photopsia and visual hallucinations are observed. Aphasia, apraxia, decreased criticism, and visuospatial agnosia are often observed. With a stroke in the vertebrobasilar region, dizziness, vestibular ataxia, diplopia, visual field defects, dysarthria, cerebellar ataxia, hearing impairment, oculomotor disorders, and dysphagia are noted. Quite often, alternating syndromes appear - a combination of peripheral cranial nerve paresis ipsilateral to stroke and contralateral central hemiparesis. In lacunar stroke, hemiparesis or hemihypesthesia can be observed in isolation.
Clinic
The symptoms of an ischemic stroke usually manifest themselves abruptly, literally in a matter of seconds or minutes. Rarely, signs appear gradually over a couple of hours or days. The clinical picture depends on the location of the brain damage.
This may be blindness in one eye, weakness or paralysis of a limb, inability to understand the speech of others, or inability to speak.
There may also be double vision, body weakness, disorientation in space along with dizziness.
Important! If the symptoms listed above occur, you should immediately call an ambulance - the sooner help is provided, the more favorable the prognosis.
Course and stages
During a stroke, several stages are distinguished: the acute period (the first 3-5 days), the acute period (the first month), the recovery period: early - up to 6 months. And late - from 6 to 24 months. Neurological symptoms that have not resolved within 24 months. From the onset of the stroke they are residual (persistently preserved). If the symptoms of a stroke completely disappear within 24 hours from the onset of its clinical manifestations, then we are not talking about a stroke, but about a transient cerebrovascular accident (transient ischemic attack or hypertensive cerebral crisis).
Causes
The most common cause of stroke is cerebral thrombosis, a blockage of an artery supplying the brain by a blood clot (thrombus). Such a clot (plaque) occurs most often in atherosclerosis. Another cause of stroke is cerebral hemorrhage, internal bleeding in the brain. An artery in the brain affected by the disease may rupture (burst) and flood nearby brain tissue with blood. The cells fed by this artery are unable to receive blood and oxygen. Cerebral hemorrhage most likely occurs when a patient has both atherosclerosis and high blood pressure. In other words, the cause of a stroke is damage to nerve cells located in the brain and controlling all functions of the human body. And such damage, or rather, the death of nerve cells, occurs as a result of an acute circulatory disorder in one or another part of the brain, when its highly active cells suddenly stop receiving the necessary and sufficient amount of blood for them. As a result, blood does not flow through the vessels, brain cells die, and commands to the corresponding muscles are not supplied, which ultimately leads to paralysis, visual impairment, speech disorders and other neurological disorders.
Consequences and prognosis
After a stroke, there are various complications, from minor to very severe.
The most common consequences are listed below:
- mental disorders. We are talking about depression, fear of being a burden, disabled. The patient may become fearful or aggressive, the mood changes dramatically;
- impaired sensitivity of the face and limbs . Nerve fibers need more time to recover than motor muscles;
- movement disorder. The limbs may not fully return to normal. Because of this, difficulties arise when dressing, holding cutlery, and walking (you will have to use a stick);
- cognitive impairment. Consequences manifest themselves in the form of forgetfulness (your name, telephone numbers and addresses, childish behavior);
- speech disorder. The patient has difficulty finding words and sometimes expresses himself incoherently;
- impaired swallowing. A person chokes on solid and liquid food, which can lead to aspiration pneumonia and sometimes death;
- impaired coordination. Manifested by unsteady walking and dizziness. Possible fall due to sudden movement or turn;
- epileptic seizure. Occurs in 10% of patients after a stroke.
The prognosis depends on the degree of damage to brain tissue, the type of stroke, proper treatment, age and concomitant diseases.
Treatment
With a stroke, the most expensive are the first minutes and hours of illness, since it is at this time that medical care can be most effective. First of all, the patient must be placed comfortably on the bed, clothing that makes breathing difficult should be unbuttoned, and a sufficient flow of fresh air should be provided. Remove dentures and vomit from the mouth. The head and shoulders should lie on a pillow to prevent flexion of the neck and deterioration of blood flow through the vertebral arteries. A patient with a stroke is always transportable lying down, only if it is not a stage 3 coma. Patients rarely die directly from a stroke; a stroke is most often accompanied by pneumonia and bedsores, which requires constant care, turning from side to side, changing wet underwear, feeding, bowel cleansing, and vibration massage of the chest.
Clinics for treatment with the best prices
Price
Total: 307in 23 cities
| Selected clinics | Phones | City (metro) | Rating | Price of services |
| Leningrad Regional Clinical Hospital | +7(812) 655..show+7(812) 655-89-27+7(812) 559-50-86+7(812) 670-55-82+7(812) 655-89-27 | St. Petersburg (m. Ozerki) | — | 20132ք (90%*) |
| Road Clinical Hospital of JSC Russian Railways | +7(812) 679..show+7(812) 679-70-03 | St. Petersburg (metro station Ploshchad Muzhestva) | — | 20420ք (90%*) |
| Military Medical Academy named after. S.M.Kirova | +7(812) 292..show+7(812) 292-34-35+7(812) 292-32-86 | St. Petersburg (metro station Lenin Square) | — | 25230ք (90%*) |
| FMITs them. V.A. Almazova | +7(812) 702..show+7(812) 702-37-06+7(812) 702-37-03+7(812) 702-51-91 | St. Petersburg (metro station Udelnaya) | — | 25335ք (90%*) |
| St. Petersburg State Medical University named after. I.P. Pavlova | +7(812) 429..show+7(812) 429-03-33+7(812) 429-03-31 | St. Petersburg (metro station Petrogradskaya) | — | 29800ք (90%*) |
| K+31 Petrovsky Gate | +7(495) 152..show+7(495) 152-59-93+7(499) 116-77-31+7(499) 999-31-31 | Moscow (m. Trubnaya) | — | 53900ք (90%*) |
| KB No. 85 on Moskvorechye | +7(499) 782..show+7(499) 782-85-85+7(926) 010-84-87+7(499) 324-70-15+7(499) 324-86-65 | Moscow (m. Kantemirovskaya) | — | 19310ք (80%*) |
| MC Healthy Woman on Ivankovskoye Highway | +7(495) 488..show+7(495) 488-32-56+7(499) 193-96-56+7(499) 520-83-16+7(499) 193-52-01+ 7(495) 942-40-43 | Moscow (metro station Shchukinskaya) | — | 21050ք (80%*) |
| DKB named after Semashko | +7(499) 266..show+7(499) 266-98-98 | Moscow (metro station Lyublino) | — | 22205ք (80%*) |
| Family Clinic in Podolsk | +7(499) 519..show Appointment +7(499) 519-35-81+7(499) 969-20-02+7(495) 662-58-85 | Podolsk | rating: 4.3 | 23400ք (80%*) |
| * — the clinic does not provide 100% of the selected services. More details by clicking on the price. | ||||
Source
Lost validity - Archive
RCHR (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan)
Version: Archive - Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2007 (Order No. 764)
ICD categories: Consequences of cerebral infarction (I69.3)
general information
Short description
The concept of “ consequences ” means the presence of certain symptoms or conditions (“residual effects”) that occur a year or more after the acute cerebrovascular disease.
The term “ cerebral infarction ” is becoming increasingly widespread with the widespread use of neuroimaging methods, which make it possible to clarify the location and size of the ischemic focus and suggest its nature. However, in its meaning, the term “cerebral infarction” is not entirely equivalent to the term “ischemic stroke.” Ischemic stroke is the clinical expression of cerebral infarction, and cerebral infarction is the morphological substrate of ischemic stroke.
When recording ischemic stroke, the principle of double coding is applied. The main one is the code that determines the nature of the ischemic stroke (I63),
an additional code denotes the clinical syndrome specified in heading G46 (Cerebral vascular syndromes in cerebrovascular diseases). This category is used for additional coding of the symptom of focal brain damage in the case of cerebrovascular accident in the area corresponding to the vascularization zone of the cerebral artery. When formulating a diagnosis of ischemic stroke, its subtype should be indicated, if possible, since this to a certain extent determines the tactics of subsequent patient management.
Protocol code : H-T-038 “Consequences of cerebral infarction” For therapeutic hospitals Code(s) according to ICD-10: I69.3 - Consequences of cerebral infarction
Mobile application "MedElement"
— Professional medical reference books. Standards of treatment
— Communication with patients: questions, feedback, making an appointment
Download the application for ANDROID / for iOS
Mobile application "MedElement"
— Professional medical reference books
— Communication with patients: questions, feedback, making an appointment
Download the application for ANDROID / for iOS
Ischemic Stroke - Review of Information
Ischemic stroke is a pathological condition that is not a separate and special disease, but an episode that develops as part of a progressive general or local vascular lesion in various diseases of the cardiovascular system. Patients with ischemic stroke usually have a general vascular disease: atherosclerosis, arterial hypertension, heart disease (coronary heart disease, rheumatic disease, rhythm disturbances), diabetes mellitus and other forms of pathology with vascular damage.
Stroke includes acute disorders of cerebral circulation, characterized by the sudden (within minutes, less than hours) appearance of focal neurological and/or cerebral symptoms that persist for more than 24 hours or lead to the death of the patient in a shorter period of time due to a cause of cerebrovascular origin. In ischemic stroke, the cause of the development of the pathological condition is acute focal cerebral ischemia. If neurological symptoms regress within the first 24 hours, the pathological condition is defined as a transient ischemic attack and is not classified as an ischemic stroke . but together with the latter they are classified as a group of acute cerebrovascular accidents of the ischemic type.
ICD-10 codes:
- 163.0. Cerebral infarction due to thrombosis of the precerebral arteries.
- 163.1. Cerebral infarction due to embolism of the precerebral arteries.
- 163.2. Cerebral infarction due to unspecified blockage or stenosis of the precerebral arteries.
- 163.3. Cerebral infarction due to thrombosis of cerebral arteries.
- 163.4. Cerebral infarction due to cerebral embolism.
- 163.5. Cerebral infarction due to unspecified blockage or stenosis of the cerebral arteries.
- 163.6. Cerebral infarction due to thrombosis of cerebral veins, non-pyogenic.
- 163.8. Another cerebral infarction.
- 163.9. Cerebral infarction, unspecified.
- 164. Stroke, unspecified as hemorrhage or infarction.
Epidemiology of ischemic stroke
There are primary (development in a given patient for the first time in life) and secondary (development in a patient who previously suffered an ischemic stroke) cases of stroke. There are also fatal and non-fatal ischemic strokes. The acute period of stroke is currently accepted as the time period for such assessments - 28 days from the onset of neurological symptoms (previously it was 21 days). Repeated deterioration and death within a specified period of time are considered a primary event and a fatal ischemic stroke. If the patient survived an acute period (more than 28 days), the stroke is considered non-fatal, and with a new development of ischemic stroke, the latter is defined as recurrent.
Causes of ischemic stroke
The cause of ischemic stroke is a decrease in cerebral blood flow as a result of damage to the great vessels of the neck and arteries of the brain in the form of stenosis and occlusive lesions.
The main etiological factors that lead to decreased blood flow:
- atherosclerotic and atherothrombotic stenosis and occlusion of the extracranial arteries of the neck and large arteries of the base of the brain;
- arterio-arterial embolism from thrombotic layers on the surface of an atherosclerotic plaque or resulting from its disintegration, which leads to occlusion of intracranial arteries by atheromatous emboli;
- cardiogenic embolism (in the presence of artificial heart valves, atrial fibrillation, dilated cardiac iopathy, myocardial infarction, etc.);
- hyalinosis of small arteries, which leads to the development of microangiopathy and the formation of lacunar cerebral infarction;
- dissection of the walls of the main arteries of the neck;
- hemorheological changes in the blood (with vasculitis, coagulopathies).
Much less often, the cause of obstruction of the patency of the carotid arteries are cicatricial traumatic and external inflammatory lesions of blood vessels, fibromuscular dysplasia, as well as pathological bends and looping of blood vessels.
Occlusion of the vertebral arteries in most cases is observed in the area from the subclavian arteries.
In addition to the sclerotic process, the cause of vertebral artery stenosis is often osteophytes, which are formed during osteochondrosis of the cervical spine.
Stenosis and thrombosis of the anterior and middle cerebral arteries occur, as a rule, at the branch site of the internal carotid artery.
When the vessels of the carotid artery system are damaged, cerebral infarction often develops, and in the vertebrobasilar region - mainly transient cerebral circulation disorders.
Symptoms of ischemic stroke
Symptoms of ischemic cerebral stroke depend on the location of the lesion, and the severity and persistence of symptoms depend on the size and condition of the collateral systems. The peculiarities of collateral circulation are such that situations may arise when, when one or more great vessels are blocked, there is no or minimal impairment of brain function, and, on the contrary, when one vessel is stenosis, a focus of softening can form with the subsequent development of persistent symptoms of brain damage. An ischemic stroke can occur at any time of the day, but more often it occurs at night, during sleep. Quite often, a gradual development of ischemic stroke is observed, mainly with a predominance of focal symptoms. In general, the manifestations of a stroke are determined by the location of the cerebral infarction, which leads to disruption of the corresponding brain functions.
Diagnosis of ischemic stroke
Patients with stroke should undergo a clinical blood test (including platelet count), biochemical analysis (glucose, creatinine, urea, bilirubin, total protein, electrolytes, CPK), coagulogram (fibrinogen content, activated partial thromboplastin time, international normalized ratio), general Analysis of urine.
Treatment of ischemic stroke
The main objectives of the ongoing treatment measures (medical, surgical, rehabilitation) are the restoration of impaired neurological functions, the prevention and control of complications, and the secondary prevention of recurrent cerebrovascular accidents.
Non-drug treatment of patients with stroke includes patient care measures, assessment and correction of swallowing function, prevention and treatment of infectious complications (bedsores, pneumonia, urinary tract infections, etc.).
Treatment of ischemic stroke is most effective in a specialized vascular department with a coordinated multidisciplinary approach to the treatment of the patient. In the structure of a hospital that has a specialized department for the treatment of patients with stroke, it is necessary to have an intensive care ward (unit) with the ability to perform CT, ECG and chest radiography, clinical and biochemical blood tests, and ultrasound vascular studies around the clock.
Stroke Prevention
The main goal of the stroke prevention system is to reduce overall morbidity and reduce the incidence of deaths. Activities aimed at primary prevention of stroke are based on a population-based social strategy for the prevention of cerebrovascular diseases at the state level (mass strategy) and medical prevention (high-risk strategy).
The grassroots strategy is to achieve positive change in every person in the general population by targeting modifiable risk factors. The high-risk strategy involves early identification of patients at high risk for stroke (for example, with arterial hypertension or hemodynamically significant stenosis of the internal carotid artery), followed by preventive drug and (if necessary) vascular surgical treatment, which can reduce the incidence of stroke by 50%. Stroke prevention should be individualized and include non-drug measures, targeted drug or angiosurgical treatment.
Classification
Currently, there are several main subtypes of ischemic stroke :
- atherothrombotic;
— embolic (cardioembolic);
- hemodynamic;
— lacunar infarction;
- ischemic stroke of the microocclusion type.
Full restoration of function after a stroke is rare, but the earlier treatment is started, the better the prognosis. Functional restoration is most active in the first 6 months.
The following stages of rehabilitation treatment :
— early recovery period (up to 3 months);
— late recovery period (up to 1 year);
- compensation for residual motor dysfunction (over a year).
Spinal stroke
A spinal stroke is a rare but dangerous pathology in which there is a disruption of the blood supply to the spinal cord.
When compared with cerebral stroke, spinal stroke is less likely to cause death, but often causes severe disability . According to the frequency of detection among other diseases, spinal stroke is diagnosed in 1% of cases.
The development of pathology begins with pain in the lumbar region, lameness, and problems with urination. Then the limbs become numb and their sensitivity is lost.
Types by TOAST
Currently, the generally accepted classification of pathogenetic subtypes of ischemic stroke is the TOAST classification.
There are five types of ischemic stroke: due to atherosclerosis of large arteries (atherothromboembolic), cardioembolic, due to occlusion of a small vessel (lacunar), stroke of another established etiology, and stroke of unknown etiology.
- Atherothrombotic attack. It is provoked by atherosclerosis of a medium or large artery.
- Lacunar. Occurs against the background of hypertension, diabetes, affecting small arteries.
- Cardioembolic. It becomes a consequence of blockage of the middle cerebral artery (MCA) by an embolus.
- Ischemic stroke , developing as a result of rare causes - increased blood clotting, hematological diseases, dissection of the arterial wall, etc.;
- Of unknown origin. Pathology occurs for unknown reasons.
Diagnostics
Diagnostic criteria : - general cerebral symptoms; - disorders of the innervation of cranial nerves; - motor and sensory disorders;
— violations of statics and coordination of movements; - cognitive and mnestic disorders, speech disorders and other disorders of higher cortical functions.
Complaints and anamnesis: - headaches; - dizziness; - noise in the head; - sleep disturbance;
- transient loss of muscle tone; - motor and sensory disorders;
- mnestic disorders; - cognitive disorders; — speech disorders and others;
— disorders of higher cortical functions, various paresthesias, arthropathy; - history of ischemic stroke (atherothrombotic, cardioembolic, hemodynamic, lacunar infarction or ischemic stroke of the microocclusion type).
Physical examination: - general cerebral symptoms; - disorders of the innervation of cranial nerves; - motor and sensory disorders;
— violations of statics and coordination of movements; — cognitive and mnestic disorders;
— disorders of higher cortical functions, including speech disorders.
Classification by affected area
The classification of cerebral infarction also takes into account the location of the lesion. Taking into account localization, the following strokes are distinguished.
Right-handed
The consequences affect the motor functions of the left side of the body, with a poor prognosis for recovery (sometimes up to paralysis). Psycho-emotional indicators remain almost normal;
Left-handed
Speech and the psycho-emotional sphere suffer, but motor functions can be fully restored . After such a defeat, the patient can only use simple phrases and individual words; he cannot form or perceive complex ones.
Cerebellar
The result is impaired coordination of movements, nausea to vomiting, and dizziness. After 24 hours, the cerebellum presses on the brain stem, the person’s facial muscles become numb, coma often begins, and death often occurs;
Extensive
It is detected against the background of the cessation of blood supply to a large area of \u200b\u200bbrain tissue. Swelling appears, then paralysis with a poor prognosis for recovery.
Important: despite the fact that stroke occurs more often in older people, there is a risk of the condition occurring at any age.
Therefore, prevention and a healthy lifestyle come to the fore.
Minor ischemic stroke
A minor stroke, or microstroke, is characterized by the disappearance of pathological symptoms (paresis, speech and vision impairment) within 3 weeks.
After this period, the person can return to their normal lifestyle.
The causes of the condition are the same as with a regular stroke - atherosclerosis plaques, blood clots in blood vessels, hemorrhages . It is important not to ignore a small stroke, as it signals problems with the blood vessels of the brain. If you do not take action, you can expect a real stroke in the future with the consequences described above.
You can differentiate a micro-stroke from a hypertensive crisis by numbness of the limb, a feeling of pins and needles, and blurred speech . Such symptoms will not be detected during a hypertensive crisis. If the symptoms described above disappear within 21 days, we can confidently say that the person has suffered a minor ischemic stroke.
In children
An acute disruption of the blood supply to the brain in a child leads to a stroke. Precursors and symptoms of pathology in children differ from similar signs in adults. A problem can be suspected by squint, rapid eye movements, instability of body temperature, convulsions, tremors of the limbs, hypo- or hypertonicity of muscles.
Treatment
Treatment tactics are aimed at: — restoration of lost functions; — correction of the underlying vascular disease; — prevention of repeated cerebral dysgemia;
- restoration of quantitative and qualitative indicators of cerebral blood flow.
Basic principles of rehabilitation
The main principles of rehabilitation are: - early start of rehabilitation; — its duration and systematicity; — stages; — complexity; - active participation of the patient.
The duration of rehabilitation is determined by the timing of restoration of impaired functions: maximum improvement in motor functions is observed in the first 6 months, everyday skills and ability to work - within 1 year, speech functions - within 2-3 years from the moment of development of stroke.
1. Improving perfusion - aimed at correcting the underlying vascular disease, preventing repeated cerebral dysgemia, restoring quantitative and qualitative indicators of cerebral blood flow.
To improve perfusion, it is necessary to resolve the issue of prescribing drugs:
1.1 Platelet and/or erythrocyte antiplatelet agents:
- acetylsalicylic acid 75-150 mg per day, long-term (thrombo ACC or cardiomagnyl, tablets 75 mg, film-coated tablets forte 150 mg);
- clopidogrel 75 mg daily;
— dipyridamole 25 mg – 3 times a day;
— ticlopidine 250 mg – 3 times a day;
- low molecular weight dextrans: trental, reopolyglucin.
1.2 Indirect anticoagulants: warfarin - for the consequences of cardioembolic stroke, for arrhythmias in doses that provide the required INR level.
2. Neurotrophic drug therapy is aimed at normalizing impaired brain functions, especially indicated for speech disorders, cognitive disorders, reduced mental and motor activity:
— citicoline 1000 mg intravenously in saline solution 1-2 times a day for two weeks; then an oral solution of 200 mg (2 ml) 3 times a day for 6-8 weeks;
— vinpocytine 10 mg – 3 times/day;
- Ginkgo biloba is taken 40-80 mg - 3 times a day with meals; course of treatment is 1-3 months.
Symptomatic treatment
1. Antihypertensive therapy. In patients who have suffered a stroke or transient cerebrovascular accident, the effectiveness of ACE inhibitors has been proven, for example, enalapril up to 10-20 mg/day; perindopril up to 4-8 mg/day; ramipril up to 5 mg/day, as well as a selective beta-blocker - bisoprolol from 2.5 to 10 mg/day.
2. Drug correction of lipid metabolism disorders in persons with coronary artery disease, as well as with atherosclerotic lesions of the carotid arteries. According to indications, statins are prescribed, for example, simvastatin up to 20 mg/day.
3. For depression - antidepressants (fluoxetine 20 mg).
4. To reduce tone with high spasticity - drugs baclofen (initial dosage - 5 mg 2-3 times a day; usual dosage - from 20 to 30 mg/day) or tolperisone from 50 to 150 mg/day.
5. For insomnia - zopiclone 7.5 mg/day for no more than 4 weeks (given the interaction with other drugs, it should not be prescribed with antidepressants, tranquilizers).
6. For central post-stroke pain syndrome: prescribing antidepressants and carbamazepine in individual dosages.
Treatment goals : - relative stabilization of the process; - restoration of lost functions.
Non-drug therapy
- strict bed rest - all active exercises are excluded;
- moderately extended bed rest - allow independent turns and transition to a sitting position;
- semi-bed (ward mode) - available types of self-service;
- free mode.
Rehabilitation should be early, carried out 24 hours a day. Rehabilitation medical team (nurse, psychologist, exercise therapy instructor, massage therapist, kinesiotherapist, speech therapist, occupational therapist and other specialists). Early use (in the first hours) of positional treatment and a special system of exercises to restore impaired motor functions. Constant stimulation of motor and mental activity. Exercise therapy is used throughout the treatment. At the first and second stages, exercise therapy is aimed at restoring impaired motor functions, at stage 3 - at the formation of a compensatory stereotype.
Rehabilitation of patients with consequences of stroke
Main objectives of rehabilitation:
— restoration (improvement) of impaired functions;
— mental and social readaptation;
— prevention of post-stroke complications (spasticity, contractures, etc.).
Indications and contraindications for rehabilitation
All patients with strokes need rehabilitation measures
Contraindications to active rehabilitation are:
- severe somatic pathology in the stage of decompensation;
- mental disorders.
Basic rehabilitation methods
For movement disorders:
— kinesitherapy, including walking training;
— household rehabilitation, including training in self-care skills (can be included in a kinesiotherapy course);
Recovery
Rehabilitation after a stroke includes neurological therapy, sanatorium treatment, and observation in a dispensary. The objectives of rehabilitation include restoration of functions (speech, movements), social and mental assistance, and prevention of complications. Taking into account the course of the disease, the following regimes alternate:
- Strict bed rest , excluding active movements.
- Moderately wide, allowing independent turning in bed and sitting up.
- Ward . Involves moving around the ward, basic self-care (eating, washing, dressing).
- Free.
The duration of each regimen depends on the severity of the condition and the degree of neurological defects.
Information
Sources and literature
- Protocols for the diagnosis and treatment of diseases of the Ministry of Health of the Republic of Kazakhstan (Order No. 764 of December 28, 2007) 1. Drug treatment for hyperlipidaemias EBM Guidelines April 22, 2004 2. Cerebrovascular disease. American College of Radiology. ACR Appropriateness Criteria. Radiology 2000 3. Aspirin for the primary prevention of cardiovascular events: recommendations and rationale/ Ann Intern Med 2002. 4. Cerebral arteriosclerosis. National Institute of Neurological Disorders and Stroke (NINDS) 5. AHA|ACC guidelines for preventing heart attack and death in patients with atherosclerotic cardiovascular disease: 2001 update. 6.Complex therapy of chronic cerebral ischemia //Ed. V.Ya. Neretina.-M.: “CJSC RKI Sovero Press”, 2001.-96p. 7.Topographic mapping of cognitive event-related potentials in a double-blind, placebocontrolled study with the hemoderative aktovegin in age-associated memory impairment. Semlitsch Heribert V., Anderer Peter, Saletu Bernd, Hochmayer Ingrid. Neuropsychobiology 1990-91; 24:49-56; Sections of Clinical Psychophysiology Pharmacopsychatry 8. Clinical recommendations. Formulary. GEOTAR_MED, M., 2004. 9.Effect of Perindopril on Cerebral Vasomotor Reactivity in Patients With Lacunar Infarction.Matthew Walters, Scott Muir, Imtiaz Shah, Kennedy Lees. Stroke. 2004;35:1899 10.The 2003 Canadian Recommendations for the Management of Hypertension: Therapy.
Information
List of developers:
Kamenova S.U. – head Department of Neurology AGIUV
Kuzhibaeva K.K. – Associate Professor, Department of Neurology, AGIUV
Attention!
If you are not a medical professional:
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Guide” cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Directory” are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.
Source