Myelography is a diagnostic method performed by introducing a contrast agent into the subarachnoid space of the spinal cord, followed by fluoroscopy. This technique allows you to diagnose a number of diseases of the nervous system that are invisible during a simple x-ray examination. Conventional radiography of the spine shows only its bone structures, and it is not possible to assess the condition of the spinal cord, its membranes and roots on an x-ray. It is these structures that myelography will show.
Of course, a more modern imaging method, which allows you to see not only the spinal cord, but also all the structures around it, is computed tomography or magnetic resonance imaging, however, there are a number of contraindications to this study, and it is not available to every patient. It is in these cases that myelography comes to the aid of the doctor and the patient. What kind of study this is, what are the indications for its conduct, whether special preparation is needed for it, whether complications are possible after it, will be discussed in this article.
When is myelography indicated?
This study is prescribed in the following cases:
- in order to detect the causes of pain, weakness, numbness of the limbs;
- if there is a suspicion of the presence of neoplasms in the area of the spinal cord canal or posterior cranial fossa;
- for diagnosing intervertebral hernias;
- to detect pathological changes in the vessels of the spinal canal;
- for diagnosing damage to the spinal cord roots;
- to identify signs of inflammation in the spinal cord and its membranes;
- if there is a suspicion of narrowing (stenosis) of the spinal cord canal.
The following diseases can be confirmed using myelography:
- syringomyelia (cavities are found in the spinal cord);
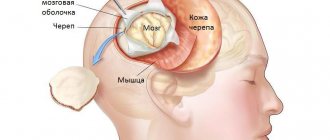
- meningocele (protrusion of the dura mater);
- traumatic spinal cord injuries;
- inflammation of the arachnoid membrane of the spinal cord, or spinal arachnoiditis;
- infections of the spinal cord and surrounding tissues;
- tumors of the central nervous system.
In addition, myelography can be prescribed to a patient before and after surgery on the spine and spinal cord in order to determine the effectiveness of treatment.
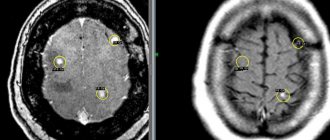
Interpretation of an MRI image of the spine with myelography
Myelograms are interpreted by a radiologist. After studying the images of the spine, the specialist forms a conclusion with detailed information about the detected changes. The final diagnosis is made by the clinician based on medical history, magnetic resonance imaging results and other research methods.
A radiologist examines MRI images.
In St. Petersburg, examination of any part of the spine with additional myelography using an expert-class Siemens Symphony 1.5 T device can be performed at the Magnit clinic. Sign up for an MRI using the number!
Contraindications for the study
There are a number of conditions when myelography must be temporarily delayed or canceled altogether. These are:
- diseases of the heart, kidneys, liver in the stage of decompensation;
- pregnancy (if the doctor and the expectant mother decide to conduct the study, measures must be taken to protect the fetus from x-ray radiation);
- acute infectious diseases with severe fever;
- anatomical or post-traumatic defects of the spine that slow down the administration of the contrast agent;
- inability to remain still;
- pustular rashes on the skin in the puncture area;
- intracranial hypertension;
- allergic reactions to the components of the radiocontrast agent.
What the pictures show
The images are interpreted by a radiologist or a functional diagnostics doctor. The 3D images are compared with previous images of the patient's or healthy person's spine. This method reveals pathological changes: osteochondrosis, hernia and others. The stage of development of the disease is determined and treatment methods are selected.
MRI of the spine can be performed an unlimited number of times to clarify the diagnosis. The photographs clearly distinguish bones and soft tissues - dark colors, the spinal cord - light shades. A tomogram helps the doctor:
- determine the degree of damage to the spine, identify developmental pathologies in the early stages;
- identify inflammation and neoplasms in soft tissues;
- detect dysfunction of the spinal membranes, determine the stage of osteochondrosis;
- identify the condition of nerves and blood vessels in the diagnosed area;
- recognize a herniated spine, protrusion of longitudinal ligaments, muscles, intervertebral discs;
- determine the nature and extent of the injury.
How to prepare for myelography
Before the study, the doctor will ask the patient in detail about the medications he is taking. Danger for the subject during myelography is represented by such groups of drugs as hypoglycemic (in particular, metformin), blood thinners (for example, warfarin), anticonvulsants and antidepressants. A few days before diagnosis, these medications should be stopped and replaced with other drugs of similar effect recommended by the doctor.
The patient should inform the doctor in detail about all allergy episodes he has had. Allergy to iodine and barium is of particular importance, since many contrast agents are based on these microelements.
The doctor must also know about all the patient's chronic diseases. Firstly, for some of them, myelography is completely contraindicated, and secondly, knowing about these diseases, specialists conducting the study can anticipate the development of certain complications and in a timely manner, and most importantly, respond adequately to them.
It is extremely important for women to notify their doctor if they may or may be pregnant because X-rays may have negative effects on the health and development of the fetus.
2-3 days before the study, the patient should exclude from his diet foods that cause fermentation and increased gas formation in the intestines (cabbage, baked goods, etc.) - the presence of a large amount of gas in it can “blur” the picture during the study. On the contrary, the amount of fluid consumed should be increased. It is not recommended to eat any food 8 hours before myelography, but you should still drink if you feel thirsty.
Before the puncture, susceptible patients may be prescribed sedatives; in addition, all subjects are given a cleansing enema.
During the examination, the patient removes some or all of his clothing and puts on a special hospital gown. It also removes glasses, jewelry, dentures, watches and other objects that may distort the image.
Can there be complications after myelography?
In the vast majority of cases, myelography is well tolerated. Despite the invasiveness, the procedure itself is not painful. During the administration of a contrast agent, the patient may feel a prick, then fullness, warmth, and sometimes a slight burning sensation. However, sometimes people feel dizzy. Approximately 20% of patients experience nausea or vomiting and headache. Therefore, it is so important to monitor the removal of contrast from the body.
Some people experience kidney problems. It is especially important for them to monitor the correct fluid intake and urination. If the patient was unable to urinate within 6-8 hours after the procedure, the doctor should be informed.
Only rarely, in some cases, do patients experience damage to the spinal canal during the administration of the drug into the spinal canal. In addition, possible complications include the development of serous meningitis and encephalopathy. There are also known cases of seizures. This is due to the fact that the contrast agent is poorly excreted and enters with the cerebrospinal fluid flow into the space between the membranes of the brain.
Preliminary preparation of the patient, analysis of his health status by the attending physician, and performance of the myelography procedure by professionals minimize the possibility of complications and side effects.
In general, the myelography method is safe. It provides invaluable assistance to doctors, as it helps to obtain valuable information - both for correct diagnosis and for monitoring therapy. The efficiency and accuracy of this diagnostic method helps many people get rid of diseases in time and regain health.
Diagnostic equipment
To perform myelography, you need a special table that can change the angle of inclination, an X-ray tube, and a monitor on which the image during fluoroscopy will be received. A special device called a fluoroscope converts X-rays into video images. To improve the picture quality of the monitor, an amplifier is used.
You will also need a puncture needle with a mandrel (a removable rod that clogs the lumen of the needle to prevent premature leakage of cerebrospinal fluid), an antiseptic solution (iodine, alcohol or another), painkiller solutions (1% lidocaine solution), and a contrast agent. As a rule, gas (nitrous oxide or oxygen) or special X-ray contrast agents are used as the latter.
To identify hypersensitivity to a contrast agent, the subject is given an allergy test: 2 ml of this drug is administered intravenously. If symptoms indicating intolerance occur, myelography is not performed or is performed using the contrast that the patient tolerates well.
The essence of examination using myelography
The myelography method is constantly being improved. In addition to an X-ray machine or fluorograph, computer or magnetic resonance imaging scanners (CT or MRI myelography) can also be used to obtain images.
In recent years, MRI has often replaced X-rays, since for some categories of patients they are safer. However, X-ray examination is still the most accessible method of examination for most patients.
The essence of myelography is that when X-rays are passed through the tissue being examined, a contrast agent illuminates the affected areas. Good visibility of the boundaries of these areas makes it possible to take clear photographs of them. The newest version of this research method is myelography with three-dimensional reconstruction.
The resulting images clearly show the spinal cord and adjacent tissues.
Research technique
In most cases, myelography is performed on an outpatient basis. If the patient has a serious somatic pathology, it is carried out in a hospital with mandatory observation by a neurologist within 24 hours after the study.
Contrast is injected into the subarachnoid space using a syringe connected to a puncture needle.
Depending on the direction of contrast propagation, there are 2 types of myelography: ascending and descending. In the first case, a spinal puncture is performed in the lumbar spine, in the second - in the cervical spine.
During the puncture, the subject is in a lying position on his side with his chin tilted towards his chest and legs bent at the knees and hip joints and pressed to the stomach. Less commonly, the puncture is performed with the patient sitting, leaning his elbows on the table in front.
The skin in the area of the intended puncture is treated three times with antiseptic solutions, after which this area is injected layer by layer with an anesthetic solution. A puncture needle under fluoroscope control is inserted into an adult at the level between the spinous processes of the 3rd and 4th lumbar vertebrae along the midline of the back at a slight upward angle (parallel to the spinous processes). When the needle passes through all the structures, pierces the arachnoid membrane and ends up in the subarachnoid space, the doctor performing the puncture will feel a kind of failure. After this, the mandrel is removed from the needle and the release of cerebrospinal fluid drop by drop is observed. A few ml of this liquid is immediately sent to the laboratory for analysis, after which a syringe is connected to the needle and a contrast agent is injected. Then the needle is removed, the skin is re-disinfected, and the patient changes position on the table - lies on his stomach face down.
And again, under the control of a fluoroscope, the radiologist slowly tilts the table - when performing a lumbar puncture, he tilts the head end, and when performing a puncture of the cervical spine, he lowers his legs. The angle of inclination is small - it is no more than 10°C.
While tilting on the monitor, the radiologist observes the spread of the contrast agent along the spinal canal - flowing around the spinal cord and other structures. The doctor pays attention to the slightest deviations from the norm and, if necessary, takes pictures of a particular area. To obtain high-quality images, the patient must lie on his side and not move at the time of the image. Even a small shake will increase the likelihood of image blur.
If there is a high risk of developing undesirable reactions to the administration of contrast, a solution of sodium thiosulfate can be administered to the patient after taking pictures.
When the examination is completed, the doctor returns the table to its original (horizontal) position and allows the subject to roll over onto his back.
In some cases, while the contrast agent is in the spinal cord canal, the patient undergoes computed tomography (in this version it is called “CT myelography”).
If a fat-soluble contrast agent was used during myelography, the doctor will evacuate it from the spinal canal at the end of the study. For 24 hours after this, the patient must remain in bed, being on a hard, flat surface (this is important!).
The research time ranges from half an hour to an hour. CT myelography takes another 20-30 minutes.
The radiologist spends some time describing and analyzing the obtained radiographs. After that, he gives a description, and sometimes the pictures themselves, to the patient. The results of the study are usually discussed with the patient not by the radiologist, but by the attending physician.
At the end of the study, the patient should be in a lying position with the head end slightly elevated for 12 hours to 24 hours. To speed up the process of removing contrast from the body, the patient is recommended to drink large amounts of water. If after rest he does not stay in the department, but goes home, it is necessary for someone to accompany him.
Where can I do it?
Myelography of the spine is a complex procedure that is not performed in all clinics. You can sign up for the study at the following medical institutions.
| Name of institution | Clinic address | Reception phone number |
| OAO "Medicine" | Moscow, st. Mayakovsky, per. 2 Tverskoy-Yamskaya 10 | +7 |
| Medical | Moscow, st. Alley Zhemchugova 5/4 | +7 |
| Scientific clinical | Moscow, Volokolamskoe highway, 84 | +7 |
| St. Petersburg, st. Marata, 6a | +7 | |
| Neurosurgical Institute | St. Petersburg, st. Mayakovsky, 12 | +7 |
Patient's feelings
Surely the reader is concerned with the question “what does the examinee feel during myelography?” When performing a puncture, a person feels light pressure in the lumbar region. At the time of contrast administration, there is a short-term burning sensation, warmth, headache and dizziness. Some patients note a salty taste in the mouth. When the drug is stopped, the patient may experience nausea and/or vomiting. In some cases, during the study, patients complain of mild pain.
Recovery period
After myelography, the patient is sent to the ward and transported on a gurney to maintain a horizontal position. During the first four hours, the patient is under the supervision of medical personnel. To remove the contrast more quickly, the patient's drinking regime is increased, and the head of the bed is also raised by 30–45 degrees. If the design is ordinary, then it is enough to place a large pillow. As the person’s condition normalizes, they are discharged.
If after the procedure there is a headache, nausea, dizziness, decreased mobility or numbness of the limbs, this indicates the beginning of the inflammatory process. Reduced urine volume and constipation should also be a concern. In this case, the patient is provided with immediate medical assistance.
After the procedure, it is recommended to avoid intense physical exercise for the first few days, for example, heavy lifting, sudden movements, or long-distance running. After a week, if you feel well, you can perform a complex of exercise therapy.
How is the preparation carried out?
A doctor performs a spinal puncture
The spinal myelography procedure requires certain preparation, which consists of abstaining from eating for eight hours before the study . It is also advisable to stop drinking. If the procedure is scheduled for the afternoon, you can drink a small amount of liquid on the morning of the test. All metal objects (jewelry made of any materials that can block x-rays) must be removed from the irradiation area.
Physicians whose task is to administer premedication should also participate in preparation for the study. When performing a lumbar puncture, it is necessary to do a cleansing enema. To suppress the swallowing reflex during spinal myelography, it is necessary to take a sedative.
Benefits and risks of myelography
Advantages:
- Myelography is a relatively safe and painless test.
- By injecting contrast material into the subarachnoid space, the doctor is able to see the contours of the spinal cord and nerve roots, which are not visible or extremely difficult to distinguish with a conventional X-ray examination.
- After completion of the examination, no radiation remains in the patient’s body.
- When used for diagnostic purposes, X-rays do not cause any side effects.
Risks:
- With excessive exposure to X-ray radiation on the body, there is always an extremely small risk of developing malignant tumors. However, the benefits of accurate diagnosis significantly outweigh this risk.
- The effective dose of radiation during myelography is different for all patients.
- Myelography is associated with a risk of headaches, although this is rare. Headaches appear after the patient returns to an upright or sitting position. One of the characteristic features of this condition is the disappearance of headaches in a horizontal position. Typically, pain begins 2-3 days after myelography. Mild attacks are relieved by drinking fluids or lying on your back, but severe headaches may require medication. In rare situations, patients continue to experience headaches, requiring a special but generally simple procedure to stop the leakage of cerebrospinal fluid from the puncture site.
- Adverse reactions to contrast material used in myelography are rare and usually mild. These include itching, skin rashes, nausea and anxiety. The development of severe urticaria and difficulty breathing is rare, but may require drug therapy. More severe reactions involving the lungs or heart are even less common.
- Other rare complications of myelography include damage to nerve tissue when the needle is inserted and bleeding around the nerve roots. In addition, inflammation or infection of the membranes covering the spinal cord is possible. An extremely rare complication of myelography is seizures. When a needle is inserted into the subarachnoid space below the site of obstruction of the outflow of cerebrospinal fluid (for example, by a tumor), in extremely rare cases an increase in pressure in the spinal canal is observed, which may require emergency surgical treatment.
- A woman should always tell her doctor or radiologist about the possibility of pregnancy.
A few words about reducing the effects of radiation on the body
During an x-ray examination, the doctor takes special measures to minimize radiation exposure to the body while trying to obtain the best quality image. Experts from international radiological safety councils regularly review radiology standards and produce new technical recommendations for radiologists.
State-of-the-art X-ray machines allow you to control the dose of X-ray radiation and provide filtration, which minimizes beam scattering. In this case, the patient’s organs and systems that are not examined receive a minimal dose of radiation.
Up