Vegetative-vascular dystonia is a disease that significantly worsens a person’s quality of life. It has many manifestations, but the most severe of them is considered to be sympathoadrenal crisis.
Sudden surges in blood pressure are accompanied by a strong fear of death. Even once an attack occurs, it remains etched in the patient’s memory for a long time.
This pathology is characterized by a rapid beginning and an equally rapid end of a negative state. After a crisis, the patient is deprived of strength and desire to act for several hours.
What is sympathoadrenal crisis
Sympathoadrenal crisis is, first of all, a characteristic state of the patient’s psyche, which manifests itself with the development of vegetative-vascular dystonia. Another name for an attack is a panic attack.
The patient begins to feel strong anxiety, and then an uncontrollable fear of death. The patient's blood pressure rises sharply, severe chest pain is felt, and the heart rate increases.
An adrenaline crisis always begins suddenly and ends just as suddenly. With frequently recurring attacks, the patient becomes withdrawn. He begins to experience suicidal thoughts. Possible development of alcoholism.
According to approved statistics, sympathoadrenal crisis occurs on average in 40–70% of the population.
Sympathoadrenal crises can develop against the background of diencephalic syndrome (another disease that is difficult to diagnose).
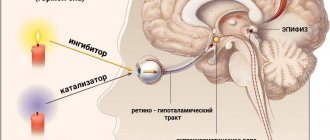
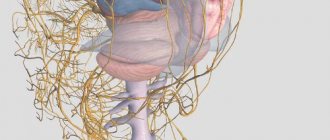
It has been established that the attack begins due to a strong release of adrenaline into the blood. The sympathetic nervous system (SNS) is responsible for the synthesis of this hormone.
Thanks to it, the body successfully copes with stress loads. The work of the SNS is directly related to the adrenal glands; adrenaline is formed in its cortex.
Under the influence of the hormone, vasoconstriction occurs, which allows (for example, in the case of bleeding) to significantly reduce blood loss.
A sudden and uncontrolled release of adrenaline has a negative effect on the human body. The sympathetic system perceives this situation as stressful. An adrenaline crisis develops.
Vagoinsular crisis: symptoms of the disease
Due to a sharp release of insulin into the blood, a decrease in sugar levels occurs - a hypoglycemic state. Signs of this pathology include severe weakness, sweating, feeling hot and a drop in blood pressure. Due to paroxysm, a person may lose consciousness within a few minutes from the onset of the listed symptoms. Since the vagus nerve regulates the functioning of internal organs, the following changes are noted:
- Bradycardia and hypotension.
- Dyspnea.
- Abnormal stool.
- The appearance of red dermographism.
- Heart rhythm disturbance.
Vagoinsular vegetative crisis can develop suddenly or gradually. In the first case, the patient instantly loses consciousness. Hemodynamic disorders are noted. Sometimes a crisis has a wave-like course. Symptoms gradually increase: weakness, deterioration, chills, sweating, hunger and nausea. These manifestations are replaced by a temporary improvement in well-being. Then they appear again.
Causes
There are several reasons that can cause symptoms of increasing fear and the development of sympathoadrenal crisis:
- internal (psychological, physical);
- external.
Psychological reasons include:
- inability to express your emotions;
- constant suppression of stress;
- bad habits;
- increased psycho-emotional stress.
Physical causes include various diseases or pathologies of internal organs, namely:
- hormonal imbalance in the patient’s body;
- problems with the cardiovascular system;
- various pathologies of the digestive system;
- suffered traumatic brain injuries;
- brain infections;
- tumors of the adrenal gland, spinal cord or brain;
- ischemia;
- excess body weight;
- elevated cholesterol levels.
External factors (genetic predisposition and the psycho-emotional background of the people around) will also have a great influence on the development of the attack.
It should be noted that in the same patient, different attacks can be triggered by completely unrelated factors.
In addition to the above reasons for the occurrence of a sympathoadrenaline crisis, there are a number of theories that explain the possibility of an attack (for example, the serotonin theory).
There is a version that incorrect functioning of the neuroendocrine system (namely, improper production of the hormone serotonin) provokes the development of a crisis.
general information
The sympathoadrenal system (systema nervorum sympathicum), when activated through the adrenal glands, ensures rapid adaptation of material metabolism, adjusted for energy sublimation, and determines the body’s adaptability to disturbances of homeostasis, especially in critical and emergency situations.
The physiological options of the SAS include the correction of many functions. In the event of the development of pathologies, the active phase of the system is transformed, provoking the reorganization of some processes. Strong and frequently repeated changes contribute to the modification of physiological regulatory reactions into the pathogenetic sphere of stimulation of adaptive diseases. They cause disturbances in the functioning of the following systems: neuropsychic, cardiovascular, endocrine and some others.
Signs and symptoms
Sympathoadrenal crisis develops instantly, and it is important to know its symptoms in order to help the patient in time.
Most often, the first signs begin to appear after suffering severe stress or extreme fatigue.
Symptoms indicating that a sympathoadrenal crisis has begun include:
- pressing, sometimes painful sensations in the chest;
- increased blood pressure;
- drying of the oral mucosa;
- vascular spasm of the extremities (arms and legs feel very cold to the touch);
- increase in heart rate;
- mono- or binocular forward displacement of the eyeball;
- chills;
- severe headache;
- problems with urination during an attack;
- sweating;
- feeling of horror;
- fear of death;
- in rare cases, increased body temperature.
Symptoms of an attack appear quickly, and then disappear just as quickly.
Sympathoadrenal function in physiological conditions
The main purpose of SAS is the sublimation of systemic and cellular energy reserves. Therefore, mild physiological stimulation allows you to create a certain energy deficit in those parts of the body that are most subject to maximum stress. The response to a lack of reserves is structural hypertrophy. At the same time, an increase in protein synthesis in them helps to avoid energy depletion.
For example, during the period of increasing muscle mass, the participation of the sympathoadrenal system is especially noticeable. For a particular muscle group to grow, it requires obvious fatigue after training. It is the SAS that makes it possible to mobilize energy reserves with some physiological depletion of muscle reserves. Signals about the depletion of reserves arrive at the receptors of the cell nucleus, provoking the activation of genes responsible for protein synthesis. As a result, the muscles hypertrophy and their mass increases.
Diagnosis of pathology
Diagnosis of sympathoadrenal crises is a rather long and difficult process. An attack developing against the background of diencephalic syndrome can be identified using differential diagnosis.
It is important not to confuse it with manifestations of other severe pathologies. Similar symptoms are caused by:
- hyperthyroidism;
- central nervous system tumors;
- epilepsy;
- post-traumatic stress;
- Addison's disease, etc.
To make a diagnosis, the doctor collects information from the patient about the manifestation of his disease. The following factors are taken into account:
- frequency of panic attacks;
- whether there was a real reason for fear;
- vegetative manifestations (tachycardia, increased blood pressure).
To clarify the diagnosis, the doctor may give a referral for examination, including:
- cardiogram;
- Ultrasound of the heart;
- spinal cord examination;
- Ultrasound of the adrenal glands and thyroid gland;
- visit to a neurologist.
Based on the information collected, a final diagnosis is made.
First aid for an attack
A panic attack always develops rapidly. Most often, assistance to a patient in this condition is not required. In almost all cases, the patient is able to independently deal with his problem and control himself.
Excessive worry can only provoke and intensify negative feelings. The environment should behave in such a way as not to aggravate the patient's condition.
When an adrenaline crisis begins, it is recommended to open the windows and unfasten too tight clothes. You can offer to drink light sedatives - such as Corvalol, Validol.
It would be a good idea to measure your blood pressure. If necessary, medications to help with hypertension should be given. If relief does not occur within half an hour, medical attention is required. It is recommended to call emergency assistance.
Treatment
An adrenaline crisis can develop both due to incorrect functioning of the autonomic nervous system and due to emotional disorders.
That is why, most often, for the treatment of sympathoadrenal crisis, treatment is recommended that is aimed not only at relieving anxiety symptoms, but also at solving identified problems.
The patient often requires not only a course of medication, but also long-term work with a psychologist.
In addition, it is important to improve your lifestyle, reducing the impact of external negative factors.
Drug therapy
Drug treatment is most often prescribed for moderate or severe disease.
The following groups of drugs are most often prescribed:
- Herbal preparations. Some herbal remedies have a mild relaxing effect on the patient. Very often this is enough to help cope with the feeling of fear. If the effect is positive, this dosage form can be taken for quite a long time.
- Beta blockers (neutralize the effect of adrenaline, thereby stopping the attack).
- Antidepressants. Prescribed for up to 6 months. After stopping the drugs, the attack may recur.
- Tranquilizers. Reduces the excitability of the central nervous system. They only relieve symptoms. Taken at the very beginning of an attack.
- Medicines that improve blood circulation.
- Nootropic drugs that improve tissue metabolism.
Self-prescription of medications is strictly prohibited.
Non-drug therapy
In addition to drug therapy, non-drug treatment also shows good results.
Since the presence of stress in a patient’s life also affects his well-being, the most reliable theory is that it requires the intervention of a psychotherapist for successful treatment.
Psychotherapy is the second, additional stage of treatment for the patient. Its main goal is to correct behavior and restore normal brain function. The most popular are hypnosis and cognitive behavioral therapy.
During such psychotherapeutic procedures, sources of stress are identified, which the patient himself is often not even aware of, and self-control improves.
Indirect action of catecholamines
For a long time it was assumed that the effects of adrenergics have only direct stimulation of the corresponding receptors. As it turned out later, the effect of many non-catecholamine inclusions of phenylethylamine is neutralized and reduced after supply with cocaine or the manifestation of chronic desympathy.
But, under similar conditions, the effect of norepinephrine is enhanced. This pattern suggests that tyramine and its analogues also have an indirect effect. In this case, adrenaline is displaced from sympathetic formations. This leads to an effect on the postsynaptic receptor node, which explains the adrenergic effect of tyramine and identical substances:
- The desympathetic process provokes the elimination of sympathetic branches.
- Reserpinization contributes to the depletion of the catecholamine depot.
- The influence of cocaine does not allow tyramine to enter the adrenergic ending, causing a blockade of drugs with an indirect effect, while simultaneously enhancing the effect of adrenergic stimulants.
Peculiarities
The most well-known method for a summary assessment of the indirect and direct effect of adrenergic models is to compare the curves of the effect on a specific organ before and after reserpinization. If the indicators are identical to each other, the drugs are classified as direct-acting substances (phenylephrine and norepinephrine). In case of neutralization of effects, the drugs are classified as sympathomimetics (indirect action). A typical representative is tyramine.
Mixed preparations are also known that have both functions. For different animals and organs, both actions from the indicated remedies may differ significantly. In humans, this ratio is not always accurately determined. Norepinephrine stimulates α and β1 adrenergic receptors; most sympathomimetics primarily affect the cardiovascular system. Non-catecholamine drugs, on the contrary, have a strong stimulating effect on β2 receptors. A typical representative of this group is ephedrine. It promotes the release of norepinephrine, while being able to neutralize bronchial spasm.
Self-coping techniques
In order to improve your well-being, reduce the frequency of attacks, and also avoid paroxysms of sympathoadrenal crisis, the patient is recommended to carefully work on himself and his condition.
First of all, it is important to understand that there is no real threat to life.
Good results for stabilizing the condition are shown by:
- meditation;
- breathing exercises;
- analytical assessment of your condition.
In addition, one should not forget about preventive measures.
Prevention
During an adrenaline crisis, the patient is tormented by fear of death, panic, anxiety and suicidal thoughts. In order to prevent this condition, it is recommended to carry out a number of preventive measures.
Doctors recommend:
- healthy sleep;
- walking in the fresh air;
- avoid overeating (it’s better to eat more often, but less);
- light physical activity;
- to refuse from bad habits;
- exclude films and programs with scenes of violence from life.
In order to completely get rid of panic attacks, the patient should completely reconsider his lifestyle and change many habits.
conclusions
Sympathoadrenal crisis is a pathology that occurs against the background of vegetative-vascular dystonia. Characterized by fear of death.
Most often, the pathology develops due to disruption of the autonomic nervous system, but disturbances of a psycho-emotional nature are also possible.
A sympathoadrenal crisis in itself does not threaten the patient’s life, but can provoke suicidal thoughts.
To avoid a paroxysm of pathology, you should work hard on yourself, change your lifestyle, and give up bad habits. In particularly severe sympathoadrenal cases, drug therapy or the help of a psychotherapist may be required.
Sympatho-adrenal crisis during menopause
This type of crisis can occur even in women during menopause . The symptoms of the pathology are the same, the causes are the same. A woman may not immediately distinguish a crisis from the symptoms of menopause, since there is also an increased body temperature and there may be problems with blood pressure.
In such a situation, professional advice . Treatment is prescribed carefully, after studying the situation and condition of the patient. Age and menopause must be taken into account.
Sympatho-adrenal crisis is a condition that is accompanied by panic and disruption of the central nervous system. It has certain provoking factors, as well as pronounced symptoms, which help to accurately establish the diagnosis. This condition is treatable and can be prevented.
06.10.2020