Indications and contraindications for lumbar puncture
The procedure in question may be performed to diagnose or treat certain diseases. If you need to obtain accurate diagnostic data, then a lumbar puncture is prescribed if necessary:
- identify or exclude the presence of an infectious agent in the cerebrospinal fluid (CSF);
- clarify the indicators of liquor pressure;
- identify the patency of the subarachnoid space of the spinal cord.
In the case of therapeutic measures, a puncture may be necessary to introduce antibacterial agents into the cerebrospinal fluid and get rid of excess cerebrospinal fluid. Indications and contraindications for lumbar puncture are divided into mandatory and conditional. As part of diagnosis and treatment, the procedure is indicated for:
- any infectious diseases of the central nervous system;
- suspected leakage of cerebrospinal fluid;
- malignant tumors localized directly in the structures of the spinal cord;
- hemorrhage into the arachnoid membrane.
Lumbar puncture is also allowed for multiple sclerosis, vascular embolism, systemic diseases, and fever in early childhood. In case of these problems, the appropriateness of the procedure in question is determined by the attending physician.
Cerebrospinal fluid puncture is often performed in premature infants, and this procedure can be decisive in making a diagnosis. Such “complex” newborns may have hydrocephalus without pronounced symptoms, and the diagnostic results from the cerebrospinal fluid will provide answers to doctors’ questions regarding the correct diagnosis.
Contraindications to the procedure in question for diagnostic or therapeutic purposes are:
- cerebral edema, severe and with severe symptoms;
- high intracranial pressure of clarified or unknown etiology;
- diagnosed brain tumors;
- occlusive hydrocephalus;
- problems in the blood coagulation system;
- pregnancy;
- long-term use of anticoagulants.
In some situations, when accurate diagnosis is required, a spinal puncture can be performed despite existing contraindications. For example, the results of a lumbar puncture analysis for meningitis make it possible to determine the type of infectious agent and select effective medications. And if a pathology is diagnosed or suspected in a pregnant woman, then doctors neglect this situation and do everything to save the patient’s life.
What is it done for - diagnostic and therapeutic purposes
Obtaining cerebrospinal fluid to determine treatment tactics, analysis and diagnostic prognosis is carried out with the goal of achieving a certain result, and before prescribing a puncture, the tasks are strictly delimited. However, there are situations when a cerebral puncture for the purpose of research, collection of cerebrospinal fluid, as material for diagnostics, turns into shunting or removal of excess fluid to reduce pressure inside the skull.
Ventricular puncture (penetration into the lateral ventricles of the brain) helps doctors achieve several goals:
- performing diagnostics by obtaining important biological fluid for research;
- measuring intracranial pressure or conducting studies with a radiopaque substance;
- operations performed using a special device - a ventriculoscope, or shunting in the cerebrospinal fluid system;
- reducing intracranial pressure by removing spinal fluid if the natural outflow system does not work.
Well-established techniques and precautions allow operations to be performed as needed, using only local anesthesia. The methods and routes of penetration have been developed over many years of practice, and the data obtained in most cases helps to carry out more effective treatment based on objective information.
How is a lumbar puncture performed?
Since the procedure in question is quite complex, it is carried out by an experienced doctor and only after preliminary preparation of the patient. Algorithm for preparing for a spinal puncture:
- the skin in the area of the future puncture and insertion of a special needle is treated with medical alcohol and lubricated with iodine;
- then novocaine or lidocaine (painkillers) is injected subcutaneously;
- immediately after the formation of the so-called lemon peel, the administration of these drugs continues intradermally and further into the future puncture.
Many patients wonder whether it hurts to do a spinal tap. Unpleasant (but not painful) sensations are possible only during the period of preparation for the procedure, when the doctor administers painkillers.
After preparation, the procedure itself begins:
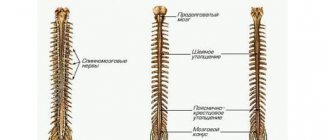
- The puncture is made between the spinous processes between the 3rd and 4th vertebrae (in childhood patients - between 4th and 5th). Some patients are terrified of a lumbar puncture because they believe that there is a possibility of spinal cord damage. But the puncture is made where there is simply none! The spinal cord ends between vertebrae 1 and 2, so there is no such threat to health.
- The doctor inserts a special needle with a device that closes its lumen (mandrin) at a slight angle. As soon as the needle enters the subarachnoid space, the specialist feels a certain “failure”. After this, you can remove the mandrin - cerebrospinal fluid will begin to come out of the needle.
- If cerebrospinal fluid does not drain, the patient may be asked to elevate their upper body to increase pressure. If the procedure in question was performed frequently, then the doctor may try to collect cerebrospinal fluid for examination a little higher than the specified location - adhesions may prevent a quick and successful puncture.
- If it is necessary to measure the pressure of the cerebrospinal fluid, a special tube is attached to the needle. But an experienced doctor will make such measurements without additional instruments - the output of cerebrospinal fluid at a rate of 60 drops per minute will indicate the norm. But it must be taken into account that the rate of spinal puncture in newborns when measuring pressure will be slightly higher.
What is a cerebral puncture?
Penetration into the cranium at the location of parts of the brain is carried out less frequently than other manipulations in places that are less dangerous and threaten negative consequences.
Although any puncture can cause complications if it is carried out unprofessionally, affects some important segments or becomes a source of infection. Each invasive procedure has features specific to a particular department, developed techniques and precautions. Brain puncture (cerebral puncture) is a collective name for a therapeutic or diagnostic procedure carried out according to indications at a strictly defined destination:
- in the lower parts of the temporal or frontal lobes;
- over the tympanic space or mastoid process;
- ventricular, in the region of the lateral ventricles;
- within the central nervous system, to obtain a sample to study the spinal cord and brain simultaneously.
To carry out the procedure, a special needle and scalpel are used, the trepanation window is cut out with a special cutter, and bone bleeding is stopped by rubbing wax or electrocoagulation. To regulate the flow of cerebrospinal fluid there is a special device - a mandrin. In most cases, the procedure is performed under local anesthesia, in compliance with all necessary conditions of sterility and preparation of a sterile surgical field.
However, just in case, a large operating room is being prepared, which in rare cases can be used to perform open brain surgery. This scenario is possible when surgical complications arise - damage to a vessel, air entering the cavity, or insertion of a needle to an unexpected height.
Although sometimes the reason for further surgical tactics is an insufficiently studied pathology located directly in the brain (abscess, abscess, cyst, neoplasm).
Complications and consequences of lumbar puncture
In the first 2-3 hours after the procedure, the patient should be in a horizontal position; some discomfort is possible - for example, a headache after a lumbar puncture, which quickly disappears and does not require the use of painkillers. You should not lift weights or walk a lot in the first 3-4 days.
Possible complications and consequences of lumbar puncture:
- irritation of the meninges;
- persistent pain in the puncture area;
- disc damage and hernia formation;
- bleeding;
- infection of the central nervous system.
More detailed information about the rules of the procedure and the cost of a needle for lumbar puncture can be obtained on the pages of our website Dobrobut.com.
Doctor's competence
Taking biological fluid for analysis or to alleviate the patient’s condition is considered a surgical intervention of a high degree of complexity. The procedure is the responsibility of the neurosurgeon and anesthesiologist. The first one must certainly have extensive practical experience in order to transfer the process from puncture to open brain surgery in case of complications.
No one is immune from errors or complications during the operation. The result may be bleeding and hematoma, damage to the brain substance itself or its vessels, displacement of brain structures or rapid swelling.
Indications
A puncture of the brain with a needle is carried out for the following indications:
- Neuroinfections and inflammatory diseases of the brain.
- Neurosyphilis, meningeal tuberculosis.
- Hemorrhagic stroke, hemorrhage into the ventricles of the brain and subarachnoid space.
- Traumatic brain injury accompanied by swelling.
Why is a lumbar puncture done:
- Confirm or deny the presence of a neuroinfection, for example, meningitis or encephalitis.
- Administer an antibiotic or chemotherapy drug.
- Reduce intracranial pressure.
Features of the procedure
Taking a puncture from a woman during pregnancy can only be dictated by emergency circumstances. The sample is taken solely according to absolute indications, since pregnant women, especially those in early pregnancy, are classified as patients at risk. The manipulation in many cases leads to miscarriage.
When performing a lumbar puncture, special attention is paid to patients suffering from cardiovascular diseases. The body's reaction to such intervention can have catastrophic consequences, including cardiac arrest or respiratory arrest.
Meningitis is a disease that can affect the human body at a very early age. Children under six months of age are often susceptible to the bacterial form of the disease. Symptoms of the disease can appear suddenly and rapidly. As in cases with adult patients, puncture is considered the main tool in diagnosing the disease. The specifics of the manipulation performed on children are completely identical to the procedure for adults.
WE RECOMMEND SEEING: The danger of viral encephalitis and how it is transmitted
The only difference is in a more complete examination of the small patient before starting the manipulation, which is associated with a large number of contraindications in children. A small patient is required to undergo a series of blood tests, a computed tomography scan or an electroencephalogram.
At the end of the procedure, children are prescribed bed rest and complete rest for 1 to 3 days to avoid complications. In the first hours after the puncture was taken, you should try to lay the child down so as not to disturb the site where the cerebrospinal fluid was taken, that is, put him on his tummy.
Consequences
Only a specially trained doctor with the necessary tools can take a puncture correctly.
As mentioned above, if the patient correctly follows all the recommendations prescribed to him and the medical staff is competent, complications after the puncture are minimal. However, there are still some situations that can appear even with competent manipulation. They make up a small percentage in the overall summary of all cases, but you should not forget about them:
- Herniation of brain structures or dislocation of midline structures.
- Pain syndrome due to damage to nerve roots.
- Headache.
- Hematomas that develop as a result of damage to small vessels along the puncture needle.
Also, a separate group of complications are complications of puncture when performed in pregnant women. Such patients, especially in the first trimester, may be at risk for miscarriages in response to puncture.
Patients with heart disease and a spinal puncture require close attention, since when vasovagal reactions are triggered, the consequences can be catastrophic, as breathing or cardiac activity may stop.