Red bone marrow plays an important role in hematopoiesis. It contains cells that provide many essential functions. Bone marrow is found in long bones, ribs, vertebrae and sternum. If pathological processes develop in it, analysis may be required.
In hematological practice, the main study of bone marrow pathologies is sternal puncture. It is carried out in the diagnosis of pathological processes occurring in the red bone marrow.
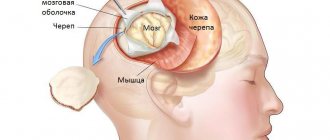
Lumbar (spinal) puncture
A lumbar puncture is a procedure in which a thin needle is inserted into the space in which the cerebrospinal fluid circulates.
This is necessary both for further study of the cerebrospinal fluid and for the introduction of various drugs into the subarachnoid space. The procedure is indispensable in some cases and can be performed by doctors of several specialties. And even though there is no longer a spinal cord in the place where the needle is inserted, the puncture is associated with certain risks. Lumbar puncture is performed according to absolute and relative indications. The absolute ones include:
- Suspicion of an infectious lesion of the membranes or substance of the brain or spinal cord;
- Oncological disease of the membranes covering the organs of the central nervous system;
- If CT or MRI is not possible, to diagnose subarachnoid hemorrhage;
- Impaired consciousness without signs of brain herniation - if it is impossible to carry out imaging diagnostic methods (neurosonography - in infants, CT or MRI - in all others);
- For the introduction of an X-ray contrast agent for the purpose of diagnosing cerebrospinal fluid fistulas, leakage of cerebrospinal fluid from natural openings (ears, nose);
- Diagnosis of hydrocephalus with normal intracranial pressure;
- For the purpose of administering antibacterial substances for severe bacterial meningitis.
Relative indications for lumbar puncture are:
- Polyneuropathy;
- Paraneoplastic syndromes;
- Demyelinating processes;
- At elevated temperature and the absence of any signs of inflammation from other organs;
- Systemic lupus erythematosus;
- Septic vascular embolism.
A spinal tap is a fairly simple procedure, but it carries certain risks due to the following conditions:
- During a lumbar puncture, performed for diagnostic purposes, about 5 ml of cerebrospinal fluid is taken for examination, which produces an average of about 700 ml per day.
- During puncture, when contrast is injected through a needle, about 10 ml of excess fluid ends up in the cerebrospinal fluid space.
- The needle passes through various tissues and can cause infection from the skin or subcutaneous tissue to enter the spinal canal.
- Even with the most careful manipulation, the vessels of the skin and deeper layers will be injured.
Therefore, lumbar puncture is contraindicated in the following cases:
- suspicion of displacement of the brain (its structures may be compressed by the bone formations of the skull, which is deadly);
- with the type of hydrocephalus that developed as a result of an obstruction to the normal flow of cerebrospinal fluid (occlusive form);
- with severe cerebral edema;
- if there is a volumetric process in the cranial cavity (tumor, hematoma);
- with reduced blood clotting (due to pathological processes or constant use of anticoagulants);
- with infectious processes (folliculitis, bedsores, furunculosis) in the lumbar region.
The last two contraindications are relative. This means that in case of direct danger to the patient’s life, the puncture should be carried out no matter what.
In very rare (1-5: 1000) cases, lumbar puncture may be complicated:
- Wedging of the brain into the bone structures of the skull;
- Headaches after the procedure;
- Pain in the back, in the leg (legs) due to injury to the spinal nerve root;
- Epidermoid cyst (this is a consequence of using needles without mandrels or low-quality needles);
- Bleeding into the tissue, including into the subarachnoid space;
- Meningitis or arachnoiditis - when an infection occurs on the membranes of the brain;
- Meningeal reaction with endolumbar administration of antibiotics or contrast agents.
Indications for spinal cord puncture
Spinal cord puncture is mandatory for infectious diseases, hemorrhages, and malignant neoplasms.
A puncture is taken in some cases for relative indications:
- inflammatory polyneuropathy; fever of unknown pathogenesis; demyelinating diseases (multiple sclerosis); systemic connective tissue diseases.
Preparatory stage
Before the procedure, medical workers explain to the patient why the puncture is being performed, how to behave during the procedure, how to prepare for it, as well as possible risks and complications.
Spinal cord puncture requires the following preparation:
Registration of written consent for the manipulation. Taking blood tests to evaluate blood clotting, as well as the functioning of the kidneys and liver. Hydrocephalus and some other diseases require computed tomography and MRI of the brain. Collection of information on the medical history, recent and chronic pathological processes.
It is necessary to stop taking blood thinning drugs, as well as analgesics and non-steroidal anti-inflammatory drugs in advance.
Before the procedure, water and food are not consumed for 12 hours.
Women must provide information about their suspected pregnancy. This information is necessary due to the expected x-ray examination during the procedure and the use of anesthetics, which may have an undesirable effect on the unborn child.
Your doctor may prescribe a medication to take before the procedure.
The presence of a person who will be next to the patient is mandatory. A child is allowed to undergo a spinal puncture in the presence of his mother or father.
Technique
Puncture of the subarachnoid space can be performed with the patient lying or sitting. It is performed at the level of the spine where the spinal cord no longer exists.
A doctor in special medical clothing treats gloved hands, treats the patient’s back three times (the first and third times with alcohol, the second with an iodine-containing solution), and dries it with a sterile cloth. Next, the puncture site is determined by palpating the intervertebral spaces at the level of bone landmarks.
In children, the puncture is performed at the level between 4 and 5, in adults - between the 2 and 3 lumbar vertebrae.
An anesthetic solution (1% lidocaine or 0.5% novocaine) is injected into the selected interval intradermally and then subcutaneously, after which the same drug is injected deeper using a regular syringe. Next, the syringe needle is removed, waited for 2-3 minutes to ensure tissue insensitivity, then an injection is made, followed by a special puncture needle being advanced inside. The introduction of a lumbar needle is accompanied by certain sensations from the doctor, based on which he removes the mandrel from the needle. Puncture of the subarachnoid space is accompanied by the outflow of cerebrospinal fluid from the needle, several milliliters of which are taken for laboratory tests.
The subsequent insertion of a lumbar needle into the skin should be painless; pressure in the back is felt only before the needle enters directly into the subarachnoid space.
Learn all about intracranial hypertension syndrome. Symptoms and treatment methods.
Read about viral meningitis in children here.
The patient can learn about the results of a cerebrospinal fluid test within an hour after the procedure. Microbiological diagnostics of the liquid (for the growth of bacteria or detection of their genome) is carried out within 3-5 days.
Normally, liquor has the following characteristics:
- colorless, transparent;
- protein: 0.15-0.33 g/l;
- glucose – approximately ½ of its content in peripheral blood;
- chlorides: 120-128 mmol/liter;
- number of leukocyte cells (cytosis): in adults - up to 10 cells in 1 microliter (children have age-specific norms, their cytosis is slightly higher);
- there should be no red blood cells;
- Pandey's and Nonna-Apelt's reactions are negative.
This type of diagnosis can be carried out free of charge according to indications in a hospital that has a neurological department that should serve the patient at his place of registration.
This diagnosis can be done for a fee in the following and other clinics:
How to take a puncture
The sequence of actions when performing a spinal puncture is as follows:
- The patient is placed on his side and asked to press his knees to his stomach and tilt his head. This position allows you to expand the spaces between the vertebrae for unhindered penetration of the needle. In some cases, the procedure is performed in a sitting position with a rounded back.
- The health worker selects the puncture site: this is the space between the 3rd and 4th or 4th and 5th lumbar vertebrae. In this place, the risk of damage to nerve tissue is eliminated, since the spinal cord ends higher.
- The skin in this area is treated with an antiseptic.
- Using a regular syringe with a thin needle, local anesthesia is performed with a solution of novocaine or lidocaine.
- After the anesthetic has taken effect, a puncture needle can be inserted. This is a special needle, 7-10 cm long, with a large clearance of 4-6 mm. The lumen of the needle is closed by a mandrin - this is a metal rod inside the needle, which is removed only when it enters the subarachnoid space of the spinal cord. The mandrin ensures the cleanliness of the needle lumen - it does not become clogged with tissue.
- During the puncture process, the needle is directed almost at a right angle to the body, pointing slightly upward. At a depth of 5-6 cm in adults or 2 cm in children, a “needle drop” is felt - tissue resistance disappears. This means that the needle entered the subarachnoid space where cerebrospinal fluid circulates.
- The mandrin is removed, and a container for collecting cerebrospinal fluid or a syringe is placed at the outer end of the needle. Normally, cerebrospinal fluid drips slowly from the needle. In cases of a strong increase in intracranial pressure, it can flow out in a stream under pressure.
- When enough cerebrospinal fluid has been drawn, the needle is slowly withdrawn. The needle insertion site is once again treated with an antiseptic and a cotton swab with collodion is applied. Collodion is a film-forming preparation (so-called skin glue).
Important. At the end of the procedure, the patient is left in a supine position for several hours.
this helps the body stabilize cerebrospinal fluid pressure and recover from shock.
Some patients (especially those who have problems with the nervous system) may respond to puncture
in the following way:
- general weakness
- headache,
- back pain,
- nausea (with possible vomiting),
- urinary retention.
If the procedure is carried out for the purpose of anesthesia, then a syringe with novocaine is attached to the needle and slowly, as the needle moves through the tissue, it is injected for pain relief.
The bulk of the anesthetic is injected into the subarachnoid space to temporarily block the sensory nerve fibers that approach the spinal cord.
Laboratory examination of cerebrospinal fluid
Analysis of cerebrospinal fluid begins from the moment it flows out of the needle. The ideal speed is 1 drop per second. If this indicator is elevated, then we can talk about increased intracranial pressure.
For reference. Next, the clarity of the cerebrospinal fluid, the presence of sediment and odor are assessed. Normally, cerebrospinal fluid will be in the form of distilled water. Some diseases of bacterial etiology lead to turbidity of the cerebrospinal fluid and the appearance of a sharp purulent odor (meningitis, encephalitis).
In the presence of pathology, the fluid may acquire a yellowish tint (this color is characteristic of the disease xanthochromia) or become cloudy (this is characteristic of inflammation of the meninges).
Various types of laboratory research are carried out on the selected material:
- biochemical analysis - allows you to evaluate the composition of the fluid and detect pathological components;
- bacteriological culture - makes it possible to detect the presence of microorganisms in the cerebrospinal fluid (normally it should be sterile);
- immunological analysis - checking for the presence of leukocytes in the cerebrospinal fluid (immune cells).
For reference. The data from these studies confirm or refute the proposed diagnosis. With such information, the doctor can prescribe or adjust treatment for the patient.
Lumbar puncture – does it hurt?
Lumbar puncture is performed with preliminary local anesthesia with lidocaine. Almost everyone experienced the sensations after the administration of this anesthetic: this is numbness, similar to what happens during dental treatment. Due to anesthesia, the injection itself is almost painless. When a spinal nerve is touched, the patient may feel a lumbago, similar to an electric shock. Headache complaints are common.
Here's how to relieve spinal tap symptoms:
- From the very beginning, after the manipulation, the patient is prescribed absolute bed rest for at least 18 hours. Sometimes, if necessary, it is extended to 3 days.
- For pain (headaches and at the puncture site), pain relief therapy is prescribed in the form of NSAIDs.
- The patient is also recommended to drink plenty of warm fluids. If necessary, plasma substitutes are administered.
Contraindications
An absolute and categorical contraindication for performing a subarachnoid puncture is the displacement of some segments of the brain relative to other structures, since the introduction of instruments into the subarachnoid space in this case leads to a difference between cerebrospinal pressure in different areas and can cause sudden death of the patient right on the operating table .
Contraindications to lumbar puncture
All possible risks and their relationship with the expected benefits are carefully weighed and assessed in the presence of the following contraindications, which are considered relative:
- infectious and pustular skin diseases in the lumbar region (furunculosis, carbunculosis, fungal diseases, etc.);
- congenital anomalies, malformations and defects of the spinal tube, central spinal canal and spinal cord;
- impaired blood clotting ability;
- previously performed blockade of the subarachnoid space.
If there are these contraindications, which most neurosurgeons and neurologists consider conditional, the procedure is postponed until the existing restrictions and diseases are eliminated. If this is not possible and diagnosis must be carried out urgently, it is important to consider all possible risks. For example, in the case of infectious skin diseases at the puncture site after puncture, the patient is prescribed antibiotics and broad-spectrum antimicrobial agents to prevent infection of the internal tissues of the body and the development of inflammatory reactions.
What is lumbar puncture
Risks of axial herniation during the procedure
Axial (cerebellar-tentorial) herniation is the descent of the brain into the foramen magnum, which is the natural opening of the skull bones. Clinically, the pathology is manifested by the onset of coma, stiffness of the neck muscles, and sudden cessation of breathing. In the absence of emergency assistance, acute ischemia and hypoxia of brain tissue occurs, and the person dies. To prevent herniation syndrome during the procedure, the doctor uses the thinnest possible needle and takes the minimum required amount of fluid to prevent sudden changes in cerebrospinal pressure.
The maximum risks of axial herniation are observed in the presence of the following pathologies:
- hydrocephalus 3-4 degrees;
- large neoplasms;
- greatly increased ICP (difference between cerebrospinal fluid pressure and atmospheric pressure);
- violation of the patency of the liquor-conducting pathways.
Complications of the procedure
In the presence of these four factors, the risk of sudden brain herniation is maximum, therefore these pathologies in most cases are absolute contraindications for lumbar puncture.
Contraindications to lumbar puncture
This manipulation is not particularly difficult for specialists. But since there is a possibility of possible negative consequences, there are also contraindications. For diagnostic purposes, only 5 ml of cerebrospinal fluid is taken, and about 700 ml is produced per day. When a contrast agent is injected into the needle, about 10 ml of fluid enters the spinal space. Infections may enter through the needle, and blood vessels may also be injured. Based on the above, the procedure should not be carried out:
- with intracranial hematoma, infringement of the brain stem, its edema, abscess, space-occupying formation and other brain modifications;
- with traumatic shocks;
- with severe damage to the spinal tissues and bedsores in the place where the puncture is made;
- with hemorrhagic diathesis;
- with pathologies of the spinal canal and impaired circulation of cerebrospinal fluid;
- with occlusive form of hydrocephalus.
One of the unpleasant and common consequences is headache after a spinal puncture. It often occurs in patients of all ages. As a rule, the pain intensifies when standing up; on the contrary, it decreases when lying down. Smaller diameter needles reduce the incidence of headaches. Often the symptom goes away on its own and spontaneously. Also, to get rid of it, bed rest, drinking plenty of fluids, analgesics and caffeine are used.
Indications for the procedure
As mentioned, a spinal tap may be performed for diagnosis or treatment. In the first case, the procedure is carried out when it is necessary to study the composition of the cerebrospinal fluid, identify pathogens in it, measure the pressure of the cerebrospinal fluid, as well as the patency of the subarachnoid (subarachnoid) space.
To study Neck braceIndications for lumbar puncture are divided into absolute and relative. In the first case, the procedure is mandatory, and in the second, it is recommended, but the decision is made by the doctor.
Lumbar puncture must be performed in the following cases:
- Infections affecting the central nervous system, for example, meningitis, encephalitis.
- Oncological formations in the membranes or structures of the spinal cord.
- Diagnosis of liquorrhea (leakage of cerebrospinal fluid) using radiocontrast agents.
- Subarachnoid hemorrhage (bleeding under the arachnoid membrane).
Relative indications include:
- Multiple sclerosis and other pathologies in which the myelin sheath of neurons is destroyed.
- Diseases characterized by systemic damage to peripheral nerves.
- Septic vascular embolism.
- Lupus erythematosus and other systemic connective tissue pathologies.
Meningitis is often preceded by an infection, and a lumbar puncture is performed to determine its cause.
During a lumbar puncture, the presence of pathogenic bacteria in the cerebrospinal fluid can be determined.
It is necessary to take cerebrospinal fluid for examination to determine intracranial pressure, the number of neutrophil granulocytes, and the presence of pathogenic bacteria (Haemophilus influenzae, meningococcus, pneumococcus).
A lumbar puncture is done to distinguish a stroke from other pathologies and to determine the cause of its development. A spinal puncture helps determine antibodies in the cerebrospinal fluid, then doctors talk about multiple sclerosis. If tuberculosis is suspected, the cerebrospinal fluid is examined for sugar, neutrophils and lymphocytes. A spinal tap is performed to detect syphilis in asymptomatic cases.
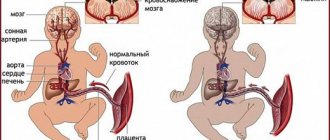
Lumbar puncture in newborns is performed if meningitis is suspected. The study will help identify the causative agent of infection (viruses or bacteria). The study will also help to identify the level of protein and red blood cells in a child, because their deficiency increases the risk of infectious diseases.
Spinal puncture is an event that has a number of contraindications:
Space-occupying formations in the posterior cranial fossa or temporal lobe of the brain. Even taking a minimal amount of lumbar fluid in this case is fraught with dislocation of brain structures and pinching of the brain stem in the space of the foramen magnum. For the patient, this all threatens instant death. The procedure is prohibited if the patient has purulent lesions of the skin, soft tissues or the spine itself at the site of the intended puncture. Relative contraindications are pronounced deformities of the spinal column. These include scoliosis, kyphoscoliosis, etc. The procedure will be fraught with complications
Puncture is prescribed with caution to patients with poor blood clotting, as well as to patients taking medications that affect blood rheology. These are anti-inflammatory non-steroidal drugs, antiplatelet agents, anticoagulants
Spinal tap kit
For manipulation, the following set of tools, preparations and materials is required:
- iodine solution 5%;
- alcohol
- collodion;
- novocaine solution 0.5%;
- syringes 5 and 10 ml;
- thin needles for syringes;
- needle for lumbar puncture (the most convenient flexible iridium-platinum needles that do not break or rust);
- a water manometer to monitor cerebrospinal fluid pressure;
- sterile test tubes, napkins and cotton wool.
Complications and consequences of lumbar puncture
In the first 2-3 hours after the procedure, the patient should be in a horizontal position; some discomfort is possible - for example, a headache after a lumbar puncture, which quickly disappears and does not require the use of painkillers. You should not lift weights or walk a lot in the first 3-4 days.
Possible complications and consequences of lumbar puncture:
- irritation of the meninges;
- persistent pain in the puncture area;
- disc damage and hernia formation;
- bleeding;
- infection of the central nervous system.
More detailed information about the rules of the procedure and the cost of a needle for lumbar puncture can be obtained on the pages of our website Dobrobut.com.
Preparing for a spinal tap
Spinal (lumbar) puncture requires preliminary preparation. To begin with, the doctor must find out the following circumstances:
- in relation to a female patient, whether she is pregnant;
- does the patient have allergic reactions to medications and anesthetics;
- are you currently taking any medications?
- about bleeding disorders.
The manipulation does not require any complicated preparation. There are only certain rules. The patient should empty the bladder and cleanse the intestines. The last meal is taken no later than 2 hours before the procedure. It is recommended to refrain from smoking on the day of a lumbar puncture. All other procedures and medications are canceled.
Indications and contraindications for use
Sternal puncture is performed when diagnosing disorders in patients with hematological diseases, as well as in other categories of patients when differential diagnosis of pathological conditions is needed.
The main indications for sternal puncture include:
- tumors of the hematopoietic system (acute and chronic leukemia);
- multiple myeloma;
- lymphomas (for comparative diagnosis with leukemia);
- anemia (hemolytic, applastic);
- myelodysplastic syndrome;
- Gaucher disease;
- leishmaniasis;
- oncological diseases of a non-hematological nature, with suspected bone marrow metastasis;
- monitoring the effectiveness of treatment for hematological patients;
- bone marrow examination of the donor;
- bone marrow examination for the purpose of autotransplantation;
- injection of chemotherapy drugs into the bone marrow (for the treatment of metastatic bone marrow lesions).
Sternal puncture also has some contraindications.
These include:
- the patient's serious condition (when important body functions are impaired);
- elderly age;
- inflammatory process in the sternum;
- purulent process in the body;
- acute infectious diseases;
- poor blood clotting;
- low level of platelets in the blood;
- acute heart failure;
- increase in body temperature on the day of the procedure.
Performing a spinal tap
Lumbar puncture - technique:
- Treatment with antiseptic soap, then alcohol or iodine.
- Apply a napkin around the puncture site.
- The patient takes the required position: lying on his side, bending his knees, pressing his head to the chest, or sitting with his back bent forward.
- Treating the puncture site with alcohol.
- Determining the puncture site (in adults - between the 2nd and 3rd lumbar vertebrae, in children - between 4th and 5th).
- Administration of a local anesthetic (novocaine or lidocaine solution).
- After waiting 2-3 minutes for the anesthetic to take effect, a spinal puncture needle is inserted. When administered correctly, the doctor and patient feel it sinking into the area of the dura mater.
- Removing the mandrin, cerebrospinal fluid begins to flow.
- Measuring pressure with a pressure gauge.
- Apply a sterile bandage to the puncture site.
Preparation and technique for performing sternal puncture
Sternal puncture is not a complex procedure; it is safe, does not require anesthesia and is performed both in a hospital and on an outpatient basis. Preparation for sternal bone marrow aspiration is extremely simple:
- The patient undergoes a blood clotting test and a general analysis no more than 5 days before the planned manipulation;
- Two hours before the puncture, the last meal and water is possible;
- Before the procedure, the bladder and intestines are emptied;
- All medications are canceled, except those that are vital;
- On the day of the puncture, no other procedures are prescribed.
Before the manipulation, the patient must inform the doctor about all the medications he is taking, especially for anticoagulants and other blood-thinning agents, which should be discontinued due to the greatly increasing risk of bleeding while taking them.
The specialist who will perform the sternal puncture will find out information about the presence of allergies to medications, since the administration of anesthetics will be required. The patient is told in detail about the essence of the puncture, its purpose and the meaning of the upcoming operation. The doctor warns about the possible pain of the puncture and subsequent precautions. It is mandatory to obtain the written consent of the person being examined (or the parents during a puncture of the child) to carry out the procedure.
The technique of performing sternal puncture includes several stages:
Lay the patient on his back and place a cushion under his shoulder blades.- Treatment of the puncture site with antiseptic solutions (iodine, ethanol); in men, the hair is shaved.
- For pain relief, local anesthetics (lidocaine, novocaine) are injected into the skin, subcutaneous tissue and periosteal space, since a puncture is a rather painful event, especially when the needle passes through the periosteum.
- The puncture is performed at the level of attachment to the sternum of the third or fourth rib, along the midline, using a Kassirsky needle, which is inserted into the bone with a quick twisting motion. When the bone marrow enters the receptacle, the doctor will feel a dip, which indicates that the needle is passing through the surface of the bone. When the needle is immersed through the compact bone layer and the bone marrow is aspirated, the patient will feel a short-term pain.
- When the needle is in the medullary canal of the sternum, a syringe is connected to it, through which the doctor aspirates 0.3 ml of bone contents.
- After obtaining the required volume of hematopoietic tissue, the needle is removed, and a sterile napkin or patch is applied to the puncture site.
Special precautions should be taken when puncturing the sternum in children. Their bone is softer and more elastic, so careless actions can pierce it through. If possible, the child should be immobilized so that his movements do not disrupt the process of puncture of the sternum.
Features of sternum puncture in children:
- Sternal puncture is possible only from two years of age;
- Special needles of smaller diameter than for adults are used;
- General anesthesia is possible.
Elderly people, patients receiving long-term corticosteroid drugs may suffer from osteoporosis, so precautions for through puncture, which is possible due to a decrease in bone tissue density, also apply to them.
The sternum puncture procedure is rarely performed without anesthesia - if it is unavoidable, and the patient has absolute contraindications to the administration of anesthetics. In such a situation, the patient is warned about the painfulness of the manipulation; it is possible to use tranquilizers before the procedure and analgesics.
The bone marrow obtained by puncturing the sternum is placed on a glass slide, then a cytological preparation is prepared, which is assessed by a cytologist. When diagnosing hematological pathology, the latter pays attention to the structure of blood cells, their number, degree of maturity, and the ratio of various elements in the total volume of punctate.
Bone marrow extracted from the sternum can also be subjected to cytochemical, immunological, and histological examination. Histological assessment of punctate provides more opportunities to assess the ratio of fatty and active bone marrow, the state of the vascular component and cellular elements of varying degrees of maturity.
The results of a sternal puncture can be obtained on the same day if a cytological examination of a bone marrow smear is expected. With histological analysis and other more technically complex studies, the diagnosis is extended for a period of 7-10 days.
The above method of sternal puncture was proposed in 1927 by Arinkin M.I. and is still practiced to this day. The Kassirsky needle has been successfully used by hematologists for decades. It is durable, wide, has a removable handle that is convenient for insertion, and is also equipped with a limiter that prevents the needle from moving too deeply.
Video: sternal puncture technique
Spinal tap in children
Diagnostic spinal puncture: obtaining cerebrospinal fluid for examination, measuring cerebrospinal fluid pressure.
Therapeutic spinal puncture: intrathecal administration of drugs, removal of cerebrospinal fluid to reduce ICP.
- lumbar region;
- fontanel in premature infants, newborns, infants (rare);
- suboccipital region (suboccipital puncture).
Conduct an explanatory conversation with the patient appropriate to his age; administer sedatives as prescribed by the doctor.
If necessary, shave the puncture site (fontanelle, suboccipital region).
By agreement with your doctor, monitor your blood sugar level (glucose level in cerebrospinal fluid = 2/3 of blood glucose level).
Check the condition of the fundus (congestive discs are a contraindication to lumbar puncture).
Pre-direct the patient to the toilet or swaddle him.
- cannula for puncture, puncture site;
- laboratory tubes with directions for research and corresponding inscriptions: tube 1 (sterile) for the number of cells and smear, tube 2 (sterile) for inoculation, tube 3 (non-sterile) for determining the level of protein, sugar, lactic acid;
- sterile gloves for the doctor;
- non-sterile latex gloves for assisting personnel;
- if necessary, sterile clothing and mask;
- skin disinfectant, sterile compress, patch.
The composition of cerebrospinal fluid and the norm of cerebrospinal fluid in adults
Liquor plays an important role in the functioning of both the spinal cord and the brain. It is a mechanical protection, forms a liquid medium necessary for biochemical processes, cell activity and the transmission of nerve impulses.
In an adult, the total volume of cerebrospinal fluid ranges from 140 to 270 ml. About half comes from cerebrospinal fluid.
The fluid is produced by the glandular cells of the choroid plexuses in the ventricles of the brain. It runs throughout the entire space of the central nervous system. The composition of cerebrospinal fluid is close to blood serum, but some components are contained in larger or smaller quantities compared to it. For example, liquor fluid contains more proteins, but about half as much glucose. In a healthy person, the cerebrospinal fluid is colorless, its density is 1005-1009 units.
Cerebrospinal fluid (liquor cerebrospinalis) has a slightly alkaline reaction with a pH range from 7.31 to 7.33. Normally it contains:
- 0.16-0.33 g/l proteins,
- 2.78-3.89 mmol/l glucose,
- 120-128 mmol/l chlorine ions.
Cerebral liquor does not contain large protein molecules. The amount of protein in it varies from person to person and changes with age (adults have more than children). Normally, the cerebrospinal fluid also contains a small amount of carbohydrates, lactic and uric acid, creatinine, cholesterol, and urea. The liquid is involved in water-salt metabolism in the body and maintaining electrolyte balance. It is constantly renewed, flowing through the glandular cells of the choroid plexuses.