A short-term abnormal narrowing of the vascular lumen due to too intense contraction of the muscular layer of veins or arteries is vasospasm of the cerebral vessels, otherwise known as vasospasm. This disorder can occur for various reasons and at any age.
However, spasm mainly affects small vessels - arteries, capillaries and venules. In this case, the blood flow passing through them is sharply limited or completely stopped. If you seek medical help in a timely manner, it is possible to eliminate cerebral vasospasm without any consequences.
Causes
Cerebral vasospasm develops as a result of the vascular wall leaving the control of the autonomic nervous system due to an imbalance in the synthesis of CNS mediators and dysfunction of the ion channels of the vascular wall membrane.
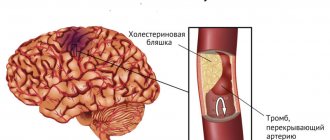
Often, along the path of blood flow in a spasmodic vessel, atherosclerotic plaques or wall thrombi occur. Diseases and pathological conditions in which cerebral vasospasm occurs:
- migraine;
- hypertonic disease;
- acute cerebrovascular accidents;
- vegetative-vascular dystonia;
- cerebral atherosclerosis;
- congenital anomalies of intracranial vessels;
- systemic vasculitis and connective tissue diseases;
- neuroses;
- chronic heart failure, heart rhythm disturbances;
- previous traumatic brain injury;
- osteochondrosis of the cervical spine;
- meningitis, encephalitis;
- postoperative period;
- liver diseases, kidney failure.
Diagnostics
Treatment of vascular spasm is prescribed after a comprehensive diagnostic examination of the patient. It is aimed at identifying the causes of this pathological condition:
- X-ray.
- Magnetic resonance examination of the cervical vertebrae area.
- Tomography of the blood vessels supplying blood to the brain.
- Angiography. How is angiography done? This is the introduction of a contrast agent through a microscopic puncture into a vessel and further monitoring of its progress using modern medical devices.
- Duplex scanning of blood flow.
At-risk groups
People of any age and gender are susceptible to cerebral vasospasm, having several risk factors for the occurrence of this pathology:
- a burdened family history that dictates a predisposition to cerebral vasospasms: early death from a heart attack or stroke, hypertension or migraine in close relatives;
- diabetes;
- predominance of the blood coagulation system over the anticoagulation system;
- brain tumors;
- altered lipid profile: high levels of total cholesterol, triglycerides, low-density lipoproteins;
- smoking, drug addiction, substance abuse;
- poor nutrition;
- dehydration of the body;
- alcohol abuse;
- abdominal obesity;
- previous streptococcal infection;
- chronic or acute intoxication with heavy metals;
- unstable psyche, stress, overwork;
- weather dependence.
Doctor's recommendations
Your attending physician will tell you in detail how to treat cerebral vasospasm. But taking the above medications should be combined with a healthy lifestyle.
For this it is recommended:
- Stop smoking and drinking alcohol.
- Establish sleep and wakefulness patterns and nutrition.
- Promptly undergo treatment for infectious and dental diseases.
- Conduct massage courses for the collar area.
- Visit the sanatorium periodically.
- Take a course of reflexology, physiotherapy, for example, electrophoresis, hydrotherapy.
Great importance should be attached to nutrition and body weight. Doctors recommend eating porridge in the morning and seafood and vegetables for lunch. It is not recommended to eat fatty, dairy, canned, fried and smoked foods, as well as sweet foods.
Coffee and tea can be replaced with herbal infusions and decoctions that help strengthen the walls of blood vessels. Such herbs include St. John's wort, rose hips, nettle and others. Carbonated drinks should also be excluded.
It is important to drink plenty of fluids daily, at least two liters. This will make it possible to avoid stagnation in the blood vessels, as well as remove harmful substances and toxins from the body.
A person’s diet should contain a lot of plant foods, fruits, vegetables, and herbs. You can add nuts and dried fruits to cereals prepared for breakfast; for lunch, you should eat legumes and lean meat along with seafood.
Signs
Intracranial vasospasm is characterized by cerebral symptoms caused by ischemia and chronic hypoxia of brain cells. Cerebral vasospasm manifests itself
- Non-localized “morning” pressing headache, often radiating to the eye sockets. Pain occurs after stress, physical activity, climate change, atmospheric and blood pressure, or a sleepless night.
- Dizziness, loss of consciousness, nausea.
- Noise in the ears.
- Feeling of heaviness and discomfort when coughing, sneezing, or bending your head.
- Decreased memory, attention, performance.
- Auditory, olfactory, visual hallucinations.
It must be remembered that the listed symptoms cannot be isolated and spontaneously occurring.
A timely visit to a doctor should establish the disease that is accompanied by them. Often, cerebral vasospasm goes hand in hand with symptoms of irritation of the autonomic nervous system:
- a drop in blood pressure with vegetative-vascular dystonia or an increase in blood pressure with hypertension;
- pallor of the limbs, redness of the facial skin;
- excessive sweating;
- increased or slowed heart rate.
For migraine sufferers, these symptoms serve as an “aura” that heralds another attack .
Prevention
To prevent such a dangerous condition as vascular spasm from bothering you again, you need to take serious measures to prevent the problem:
- Gradually increase physical activity on your body. Start with long walks outdoors. Then replace them with cycling in the park, jogging or swimming. These exercises actually help strengthen the walls of blood vessels.
- Physical activity should be constant, systematic, but not burdensome. Achieving the results of professional athletes is even dangerous here.
- Completely avoid both alcoholic and highly carbonated drinks. If you smoke, you definitely need to quit this habit. If there are reservations regarding alcohol, then you should categorically refuse tobacco.
- Take care of proper nutrition. Remove foods containing refined fats from your diet. Significantly limit yourself to eating foods rich in animal fats.
- Consider eating cereals, seafood, low-fat fish and seafood dishes, as well as low-fat dairy and fermented milk products, legumes, fresh fruits and vegetables.
- Please note that survivors of vascular spasm are also prescribed plenty of fluids - at least 2.5 liters per day. This can be purified water, fresh natural fruit drinks and juices.
- An integral part of prevention is full, healthy sleep of at least 8 hours a day. It is advisable to purchase an orthopedic mattress, on which both the skeleton and muscles relax.
Vasospasm is a condition that cannot be ignored. It is important to provide timely first aid, as well as subsequent treatment and a set of preventive measures.
Eye spasms
a close relationship between the ophthalmic artery and the vessels supplying blood to the brain tissue . Therefore, an attack of cerebral vasospasm is almost always accompanied by impaired blood flow in the retina, spasm of the eye muscles and manifests itself
- disturbance of accommodation (inability to focus on close or far away objects);
- darkening of the eyes, a feeling of flickering “flies”.
Prolonged oxygen starvation of the retina leads to swelling of the optic nerve , detachment and death of retinal cells, increased intraocular pressure, and loss of vision.
Spasm of the vertebral arteries in a child
The causes of spasm of the vertebral arteries in a child may be the following factors;
- abnormal location of the cervical arteries at birth;
- tortuous arrangement of blood vessels, which is a congenital pathology;
- various traumatic injuries, including those received at birth;
- spasms of the neck muscles resulting from hypothermia or congenital or acquired pathologies.
Spasm of the vertebral arteries in a child is dangerous because if measures are not taken to eliminate it, the blood supply to the brain may be disrupted, which entails speech impairment and paralysis of the limbs. If such symptoms continue throughout the day, we can talk about a transient ischemic attack. If no measures are taken to eliminate this condition, it can develop into further complications. These may well include a stroke, the nature of which in this case is ischemic. It is observed due to the fact that one of the vertebral arteries is blocked from the outside or from the inside to such an extent that the blood passing through it becomes insufficient for the full functioning of the area of the brain it supplies.
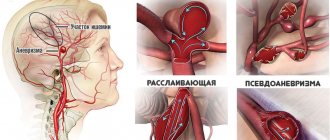
Danger and consequences
Often, cerebral vasospasm is a symptom of diseases requiring urgent surgical treatment (undiagnosed tumor, aneurysm, acute or chronic cerebrovascular accident), in which spasm of intracranial vessels is secondary. Ruptures of an aneurysm or sclerotic arterioles are fraught with hemorrhagic stroke.
An equally dangerous consequence of cerebral vascular spasm is ischemic stroke, caused by the separation of a wall thrombus or the destruction of an atherosclerotic plaque and blockage of the lumen of the arteries supplying the brain.
In children, long-term neuronal ischemia left untreated leads to mental retardation, neuropathy, hearing and vision loss.
Pathology therapy
Treatment of cerebral vasospasm will depend on the cause of its development. If you only eliminate the symptoms of the disease, it will appear again after a while. When determining the primary disease, all efforts must be directed toward its elimination. Once the cause of the disease is eliminated, the symptoms will subside.
But it is not always possible to identify the cause of the disease, and therefore it is not possible to eliminate it. In this case, the doctor develops a treatment strategy that will include changing the patient’s lifestyle.
People with vasospasm of cerebral vessels must remain in bed for four weeks. Drug therapy includes taking the following drugs:
- the action of the drugs is aimed at eliminating infection in the brain;
- painkillers in the form of intravenous injections of “No-shpa” or “Revalgin”;
- sedatives (sedatives), for example, Motherwort;
- tranquilizers: “Relanium”, “Seduxen” and others;
- nootropic drugs: “Piracetam”, “Nootropil” and others;
- drugs for normalizing cerebral vessels: Cavinton, Cerebrolesin;
- vitamin complexes;
- adaptogens: lemongrass, ginseng.
Quick relief of spasm
Sometimes mild vasospasms can be relieved at home on your own. For this it is necessary
- provide a flow of fresh air;
- keep your feet in cold water;
- drink a glass of warm water;
- lie down on a horizontal surface with a pillow under your head;
- perform self-massage.
Massotherapy
The technique can be used as a 10-15-day preventive course for the treatment of cerebral vasospasm or for pain relief as needed. The impact on each point is carried out for 2-3 minutes 5-7 times a day.
It is advisable to apply moderate pressure on symmetrical points simultaneously and combine them with massage until the skin above the active zone becomes slightly reddened. Eyes should be closed while massaging active zones.
Start with a light circular massage, gradually increasing the strength and depth of pressure over 3 minutes.
- 3-3.5 cm outward from the line vertically dividing the face in half, find the protruding tubercle of the frontal bone. The point is located on its convexity.
- Where the aforementioned midline of the face intersects with the horizontal hairline.
- Using the same line and a perpendicular lowered to it, drawn through the middle of the crown, mentally divide the head into 4 equal parts and find the central point in the crown area.
- Mark the area located along the posterior edge of the outer wall of the orbit, which is the anterior border of the temporal fossa. At the intersection of the zygomatic arch with the conditional line, which is a continuation of the eyebrow, the desired point is located.
- Behind the branch of the lower jaw, under the earlobe, find the mastoid process and the sternocleidomastoid muscle attached to it. At the top of the depression formed by the muscle and the platform of the process, the desired point is located.
- Another pair of symmetrical points is located 2-3 mm inward from the lacrimal caruncle on the bridge of the nose.
- At the top of the curve of the brow ridge, which usually corresponds to the break point of the eyebrow.
- Under the occipital protuberances, at the junction of the base of the skull with the upper cervical vertebrae, along the outer edge of the superficial suboccipital muscles, which can be easily palpated here.
Medications
Taken strictly after treatment has been prescribed by a doctor in the absence of contraindications. To relieve attacks of cerebral vasospasm, the following are used:
- vasodilators;
- drugs to improve cerebral circulation;
- antispasmodics.
What can you do at home?
There are effective methods to help relieve vasospasm at home. But before you begin to solve the problem yourself, you need to make sure that the measures you take will not aggravate the situation.
Classic drugs used for vascular spasms: Corvalol, No-spa and valerian or motherwort extract; to relieve spasms of the coronary vessels, you must take Nitroglycerin. Medicines should be taken according to instructions.
Rubbing the limbs (for peripheral vascular spasms), head massage (for cerebral spasms), and compresses help relieve spasms. Essential oils have a relaxing effect, inhaling the aroma of which will help relieve spasm of the blood vessels in the head - this is the essential oil of jasmine, thyme, mint, lavender.
It is important that if a person experiences the symptoms listed above, it is necessary to immediately consult a doctor in order to prevent further dynamics of the disease in time.
Treatment
If organic brain lesions, blood clots or atherosclerotic plaques are detected in the lumen of blood vessels, surgical treatment is indicated. In most cases, transient vasospasms are stopped or prevented conservatively.
We invite you to watch a useful video on this topic.
Severe exacerbations are an indication for hospitalization.
Drug treatment
| Groups, drug names, prices | Contraindications |
| Slow calcium channel blockers (Adalat - 190 rubles, Cinnariin - 55 rubles, Flunarizine - about 6000) |
|
| Antidepressants (Azafen – 200 rubles, Amitriptyline – 40 rubles) |
|
| Sedatives (Motherwort, Valerian – 70 RUR) |
|
| Antispasmodics (Drotaverine – 80 rubles, No-shpa – 200, Papaverine – 80, Revalgin – 190 rubles) |
|
| Nootropics (Piracetam – 150, Nootropil – 300 rub.) | |
| Drugs that improve cerebral blood flow (Vinpocetine - 80 rubles, Cavinton - 300, Cerebrolysin - 720, Actovegin - 600 rubles) |
|
Vitamins – nicotinic acid, vitamins E and C.
Traditional treatment
- Apply chilled compresses or ice cubes wrapped in cloth with infusions of dandelion and plantain root to the temples.
- Garlic broth, 3 teaspoons during meals.
- Drink a decoction of rose hips, valerian, motherwort instead of tea. Brew 2-3 teaspoons per 1 liter of boiling water.
- Drink a decoction of thyme leaves (3 tablespoons per 1 liter of water) with finely chopped garlic in courses of 2 weeks.
- Every day eat a clove of garlic, 5 tablespoons of honey with lemon slices. Drink with a weak herbal decoction.
Alternative medicine
Many traditional medicines help normalize blood circulation and vascular tone, but they are recommended to be taken regularly.
The most popular remedy for strengthening blood vessels is garlic. It needs to be crushed and filled with vegetable oil (one head of garlic per two hundred grams of oil). The mixture is left for one day, after which one teaspoon of lemon juice is added. This remedy is recommended to be taken one spoon in the morning, the course of treatment is three months.
To increase the elasticity of blood vessels, take the following remedy, one spoon per day: crush five lemons and five heads of garlic, pour in 1/2 liter of liquid honey and leave for seven days.
Every day, instead of coffee, you should drink a decoction of rose hips, St. John's wort or birch leaves. To prepare it, pour one spoon of plants with a glass of boiling water and leave for about two hours. This drink makes it possible to normalize blood circulation and increase vascular tone.
You can also prepare the following remedy. Pour three tablespoons of thyme into one liter of water, boil and leave for about an hour. Then squeeze one spoonful of juice from the golden mustache and add it to the decoction. Take this remedy 100 g per day, the course of treatment is two weeks.
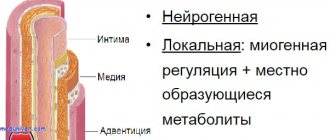
Pathogenesis
Angiospasm can occur only in arteries whose walls contain a well-developed muscle layer that overcomes intravascular pressure during contraction and sharply narrows the lumen of the vessel. This reduction in the lumen is achieved by thickening the intima of the vessel due to a significant shortening of the perimeter of the media, and the internal elastic membrane wriggles, and the endothelium protrudes into the lumen of the vessel.
If under normal conditions two conjugate processes occur in the smooth muscle cells of blood vessels under the influence of contractile stimuli - contraction and necessarily followed by relaxation, then with vasospasm relaxation is impaired and, as a result, the artery remains in a state of sharp narrowing for a long time. Long-term muscle contraction requires energy expenditure. Even a sharp vasospasm, difficult to eliminate during life, naturally disappears after death, when the metabolism in the arterial wall stops. Therefore, during autopsy of corpses, vasospasm itself cannot be detected (only the ischemic changes in tissues caused by it during life remain), which was one of the reasons for denying the possibility of vasospasm, for example, in the brain.
Angiospasm may be based on two pathogenetic variants. Angiospasm occurs either when there is excessive vasoconstrictor stimulation of the arterial wall by a nervous or especially humoral route (for example, vasospasm of the arteries of the retina and brain at the beginning of a migraine attack), or when the function of the arterial wall itself changes in such a way that even ordinary vasoconstrictor influences cause its contraction like vasospasm. Local organic, metabolic, functional changes in tissues often play a decisive role in the pathogenesis of vasospasm. Thus, spasm of the cerebral arteries is often observed near aneurysms or subarachnoid hemorrhages; with Raynaud's disease, the walls of the digital arteries become highly sensitive to the effects of cold due to local disturbances, since vasospasm also occurs after vascular denervation.
Not all arteries can be equally susceptible to vasospasm. Angiospasm detected by X-ray contrast angiography in the brain, heart and limbs is localized mainly in large-caliber arteries. However, X-ray contrast angiography cannot be considered an adequate method for studying vasospasm, in particular because there are no contrast agents that are completely indifferent to blood vessels and do not themselves cause vascular reactions. In clinical practice, symptoms of vasospasm are noted mainly in medium-sized arteries. Apparently, the tendency to develop vasospasm depends on the functional characteristics of the arteries, in particular on their typical functional behavior when regulating blood circulation. In general, vasoconstriction should develop more easily in those parts of the vascular system where vasoconstrictor innervation is better developed, where endogenous vasoconstrictor agents (catecholamines, serotonin, vasopressin, etc.) or physical environmental factors (cold) act more strongly and, finally, where vasoconstriction is a typical type vascular reactions under physiological and pathological conditions.
Due to the lack of adequate methods for studying vasospasm and lack of knowledge about the mechanisms of smooth muscle contraction, the pathogenesis of vasospasm in most organs remains poorly understood until recently. It is known that the cause of vasospasm can be changes in different links of the complex chain of processes that carry out the mechanism of contraction and relaxation of vascular smooth muscles. Based on the available experimental data, the following possible mechanisms are identified in the pathogenesis of vasospasm:
1. Stimulation of intensive and long-term synthesis of endogenous vasoconstrictor substances such as alpha-adrenergic agonists (see Catecholamines), serotonin (see), etc. in the arterial wall, which leads to its long-term contraction. For example, in relation to the internal carotid artery, it was shown that vasospasm can occur as a result of the mobilization of serotonin in the arterial wall under the influence of foreign proteins circulating in the vascular lumen.
2. A disorder of the normal destruction of endogenous vasoconstrictor substances in the arterial wall, for example, when the function of monamine oxidase, which destroys catecholamines and serotonin, is impaired (in experiments, this is achieved by pharmacological inhibition of monamine oxidase, for example, iproniazid or nialamide).
3. Disruption of the normal function of muscle membranes. In non-contracted muscle, the membranes are polarized due to the active transfer of ions through them (potassium - into the cell, sodium - out). Membrane depolarization is one of the essential parts of the process preceding the contraction of myofilaments, after which, thanks to active ion transport (the work of the “sodium-potassium pump”), membrane polarization is restored (repolarization) and myofilaments relax. If the processes leading to the repolarization of muscle membranes are disrupted, then the arterial wall remains contracted for a long time. Such disorders may depend on pathological or age-related changes in the membranes of vascular smooth muscle cells, disruption of enzymatic reactions that actively transport potassium and sodium ions across cell membranes, and from disruption of other processes involved in membrane repolarization.
4. Disruption of the normal transport of calcium ions in smooth muscle cells. After depolarization of muscle membranes, calcium ions are transferred inside the myofilaments and cause their shortening - smooth muscle cells contract, that is, calcium ions are the trigger mechanism for contraction. The subsequent removal of calcium ions from myofilaments causes the process of their relaxation. Thus, disruption of the release of calcium ions from myofilaments (due to dysfunction of the “calcium pump”) can cause vasospasm. It has been found that the antispasmodic effect of some drugs, for example. papaverine, methylxanthines (theophylline, caffeine and others), is carried out through the release of calcium ions bound in the myofilaments of the smooth muscle cells of the arteries.
5. Angiospasm may also depend on disruption of the relaxation process of myofilaments due to changes in their proteins. The immediate causes of such disorders are poorly understood.
Clinical picture
Clinical signs of vasospasm are nonspecific; they are associated with its localization and consist mainly in disorders of the function of ischemic tissue. The degree of functional disorders is proportional to the degree and duration of vasospasm.
It is believed that vasospasm in the coronary artery system forms the clinic of angina pectoris (see) and can be the cause of myocardial infarction (see) with its corresponding symptoms; spasm of the mesenteric vessels is manifested by abdominal toad (see); spasm of the cerebral arteries underlies the pathogenesis of some variants of cerebral crises and strokes with characteristic symptoms of focal neurological disorders. The development of vasospasm in muscle organs is often expressed by pain in the ischemic zone with irradiation along the corresponding segment of somatic innervation.
The course of vasospasm is most studied when it is localized in the vessels of the extremities. Short-term vasospasm of the digital artery causes a sharp pallor and coldness of the finger with impaired pain and tactile sensitivity from local paresthesia to anesthesia. This set of symptoms is characterized as a “dead finger” (digitus mortuus). Similar signs develop throughout the entire limb with vasospasm of its arteries, usually accompanying their organic damage. The alabaster (statue-like) pallor of the leg that develops in such cases is a symptom referred to as “commander’s foot.” In the case of prolonged vasospasm of the arteries of the extremities, the appearance of distal cyanosis is observed, sometimes evenly distributed, sometimes in the form of a cyanotic mesh, giving the impression of marbled skin. The appearance of cyanosis is caused by paresis of venules in the ischemic zone and is noted only when blood can enter them through anastomoses from veins in which blood flow continues, or when some minimum level of capillary blood flow is maintained due to partial patency of the spasmodic arteries. With digitus mortuus, cyanosis is usually absent, but it often occurs with ischemia of large areas of the limbs. Following cyanosis, some swelling of the tissue develops, caused by an increase in capillary permeability to proteins due to membrane hypoxia. At the next stage, necrobiotic processes develop - the faster, the greater the gap between the tissue's need for oxygen and the amount of blood flow. In the heart muscle, where the need for oxygen is high, foci of dystrophy develop after several minutes of ischemia.