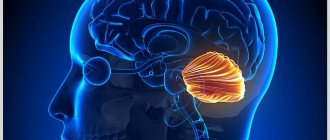
A cerebellar cyst is a dangerous neoplasm that can lead to disruption of brain activity and paralysis of the limbs. This type of benign tumor requires mandatory treatment. The characteristics of the compaction determine whether the doctor will prescribe drug therapy or surgical intervention.
It threatens with disruption of brain activity and paralysis of the limbs.
Features of the pathology
A thickening is a cavity that appears in different parts of the cerebellum. It is filled with liquid contents and gradually increases in size. This cyst provokes consequences, so it must be treated immediately after diagnosis.
The pathology is located between the roof of the brain (blue arrow) and the pineal gland (red arrow).
The difficulty in prescribing therapy in a timely manner is that there are no symptoms, at least in the early stages of tumor development. As its size increases, signs appear, but by this time the capsule may already have grown significantly.
Causes
Cysts in the cerebellum can be congenital or acquired. Its causes depend on what type it belongs to. If the neoplasm is of the congenital type, it is formed during the period of embryonic development. This is due to developmental disorders during pregnancy or death of brain tissue. Necrosis may occur due to suffocation. This occurs during childbirth or in cases where the fetus, for certain reasons, lacks oxygen.
Risk factors that provoke the development of acquired pathology include:
Head injuries, concussions.
- acute foci of inflammation;
- hematoma in the brain area, which appeared due to mechanical impact;
- stroke;
- previous surgical interventions (related to the brain);
- concussions;
- injuries, blows, skull fractures;
- infections with parasites;
- multiple sclerosis.
Can it develop into cancer?
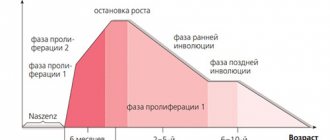
In most cases, meningioma is a benign formation. In this case, the tumor is characterized by slow growth.
However, in the absence of timely diagnosis and quality treatment, the pathological neoplasm gradually increases, compresses adjacent tissue structures and degenerates into a cancerous disease.
Damage to the cerebellum is dangerous because the defect is often located next to the brainstem. Because of this, surgical intervention is difficult; the specialist is forced to only partially excise the formation.
If malignant degeneration occurs, the tumor compresses the medulla, causes metastasis, and often recurs.
Types of cysts
Doctors have developed classifications that relate to the location and etiology of the tumor. There are the following varieties:
- Cystic-glial changes usually appear against the background of previous injuries in the head area. A cyst of the right or left hemisphere of the cerebellum has pronounced symptoms. These include worsening migraines, constant loss of strength, and dizziness. Subsequently, convulsions appear;
- A retrocerebellar tumor occurs where necrosis of gray matter cells occurs. This is often associated with a stroke, surgery in the skull, or blows. If it appears between the hemispheres, it is triggered by problems with the blood supply to tissues, with infections and with a source of inflammation. It provokes a severe migraine, which painkillers cannot cope with, as well as significant changes in consciousness and even hallucinations;
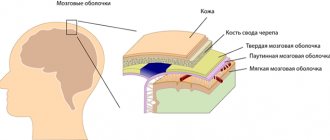
Occurs in the place where cell necrosis occurs. - An arachnoid cyst appears in the cerebellar space. The appearance of the capsule is facilitated by scars on the tissue, which are associated with problems with the flow of cerebrospinal fluid. Signs appear depending on where the lump appears. An arachnoid cyst must be removed if it enlarges. When the capsule reaches a large size, it causes severe symptoms, such as seizures similar to epilepsy;
- the subarachnoid cavity is usually congenital. It is discovered after the baby is born during a standard examination. Less commonly, this type of neoplasm is acquired. Then the appearance is associated with infection with neuroinfections, with a stroke. Accompanied by pulsation in the brain tissue, convulsions;
- A pineal tumor appears in the pineal gland, which affects the production of hormones. An epiphysis cyst is characterized by loss of orientation in space and a constant desire to go to bed. The patient may experience double vision;
- pseudocyst is a congenital type of seal. They lack a lining of epithelial tissue.
Chapter 4. CEREBELLUM. SYMPTOMS OF DEFEAT
CEREBELLUM _
Located in the subtentorial space of the skull above the brain stem
(see), consists of white and gray matter. It consists of a worm and two hemispheres. Gray matter is represented by paired nuclei: tent, spherical, corky and dentate, as well as the cortex covering the entire surface of the cerebellum. The cerebellum is connected to other parts of the brain by the lower, middle and superior peduncles, consisting of afferent and efferent pathways. The cerebellum is involved in coordinating movements, regulating muscle tone, coordinating the actions of agonist and antagonist muscles, and maintaining balance.
CEREBELLAR SYNDROME
Damage to the cerebellum manifests itself as static
and
dynamic ataxia
(see), impaired coordination of movements, horizontal
nystagmus
(see),
scanned speech
(see),
intention tremor
(see),
hypermetry
(see),
megalography
(see),
asynergia
(see) , decreased muscle tone.
Ataxia
From Greek: a -
negation +
taxis -
movement - erratic, discoordinated movements.
(static ataxia,
see) and purposeful movements
(dynamic ataxia,
are possible due to a disorder in the coordination of the muscles of agonists and antagonists, manifested by
dysmetria
(see) and disproportionality of movements.
May be caused by damage to the cerebellum and its connections (cerebellar ataxia,
see), the posterior parts of the frontal lobes and their connections with the cerebellum
(frontal ataxia,
see), the vestibular analyzer
(vestibular ataxia,
see), reverse afferentation due to muscle disorder -articular sensation
(sensitive ataxia,
see).
In addition, the phenomena of ataxia can be a consequence of damage to the posterior columns of the spinal cord (posterior columnar ataxia,
see).
Cerebellar ataxia
It occurs due to damage to the vermis, hemispheres and cerebellar peduncles. Can be observed with its tumors, MS
(see), infectious, toxic and vascular diseases, hereditary processes, primarily
Friedreich's diseases
(see),
Pierre Marie
(see),
olivopontocerebellar degeneration
(see),
Louis-Bar disease
(see), in which ataxia is the leading clinical sign.
Damage to the cerebellar
(see) is accompanied by the loss of physiological synergies that ensure stabilization of the center of gravity, which leads to “trunk”, static ataxia against the background of diffuse muscle hypotonia.
In this case, it is difficult for the patient to be in an upright position, in particular in the Romberg test
(see), he falls forward or backward, which is associated with damage to the front or back part of the worm, respectively, when walking he spreads his legs wide apart, shows caution, the steps are of different lengths, deviates to the sides
(cerebellar gait,
see).
With lesions of the cerebellar hemispheres, muscle hypotonia and dynamic ataxia
(see) appear on the side of the pathological focus.
Movements often become excessively sweeping (hypermetry,
see), accompanied by
intention tremor
(see),
adiadochokinesis
(see), speech is changed according to the type of
cerebellar dysarthria
(see), handwriting changes
(megalography,
see). In the Romberg test and when walking, the patient sways and deviates towards the pathological process. Horizontal nystagmus is often noted. Deep sensitivity is not impaired. Visual control does not have a significant effect on motor coordination.
Symptoms
It is quite difficult to determine the development of a cyst in the early stages. This happens because it does not manifest itself in any way and does not bother the person. Congenital tumors may not affect infants and sometimes resolve spontaneously.
If the acquired neoplasm increases in size or even provokes the appearance of adhesions, the following symptoms occur:
- there is a feeling of compression and pulsation in the area of the skull;
- Coordination gradually deteriorates, the patient experiences loss of orientation in space;
- tinnitus is accompanied by nausea. Possible partial hearing loss, bouts of vomiting;
- the pain in the head sometimes becomes very severe. Painkillers do not cope with it;
- the rhythm of sleep and wakefulness is disrupted, insomnia appears;
- in difficult situations, convulsions, trembling of hands and fingers occur;
- periodic fainting occurs;
- subsequently vision deteriorates, paralysis (partial or complete) cannot be ruled out;
- the person begins to limp and cannot relax the muscles that are cramped by tension or cramps.
If we talk about symptoms in newborns, we are talking about constant regurgitation and vomiting.
What is the danger?
Small seals do not pose a danger to human life and health. The problem is that in most cases they continue to grow and begin to put pressure on the brain tissue. This provokes the following complications:
Complete or partial paralysis cannot be ruled out.
- blood circulation deteriorates, insufficient oxygen reaches the cerebellum;
- irreversible processes occur that affect speech, vision, hearing, and coordination of movements;
- complete or partial paralysis cannot be ruled out, in which it is impossible to restore lost functions;
- in the most severe cases, the pathology leads to the death of the patient.
Sometimes spontaneous rupture of the capsule membranes occurs, which leads to sepsis and a purulent inflammatory process in the cerebrospinal fluid. There is also a risk of internal bleeding, paralysis and death.
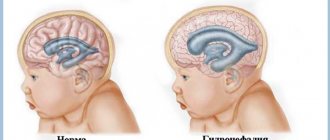
A cerebellar cyst in a newborn child (if it does not resolve) causes developmental disorders and delays in many functions.
Likely consequences
In the final stages, a large tumor causes memory loss, epileptic seizures with convulsions, impaired concentration, balance, coordination of movements, and mental disorders.
If a malignant degeneration of the tumor occurs, then the lack of timely treatment leads to the growth of the pathology into neighboring tissue structures, damage to the brain stem, and the occurrence of metastases, which often lead to death.
In addition, meningioma of the tentorium cerebellum is prone to recurrence. During surgical removal, there is a possibility of infection, bleeding, and swelling.
Diagnostics
During a visit, during which the patient complains of unpleasant symptoms, the doctor prescribes diagnostic measures to clarify the diagnosis. MRI is considered the most revealing examination method. Magnetic resonance imaging demonstrates where the tumor is located and clarifies its size and structure. During the examination, you can find out how the tumor affected the surrounding tissues, whether deformation of the worm and other parts has occurred.
In addition to MRI, the following procedures are prescribed:
- puncture. Provides analysis of cerebrospinal fluid in order to exclude or confirm an inflammatory process in tissues;
- the contents can be sent for histological examination in order to clarify the nature of the compaction. If cancer cells are present, the treatment will be radically different than for a benign type of cyst;
- An electroencephalogram is designed to calculate convulsive contractions of the brain. The results of this manipulation also influence the prescribed treatment;
- if the patient is a small child who has not yet turned 2 years old, neurosonography is prescribed. This is a safe type of research that gives a complete picture of the processes occurring in the cerebellum;
- A blood test is necessary in order to exclude concomitant infectious diseases or foci of inflammation.
RADIAL ANATOMY OF THE POSTERIOR CRANIAL FOSSA STRUCTURES
Radiation anatomy of the brain.
The posterior cranial fossa is a part of the base of the skull, limited centrally in front by the dorsum of the sella turcica and the clivus, in the anterolateral sections by the pyramids of the temporal bones, below by the basal part of the occipital bone, and along the posterolateral surfaces by its scales. It communicates through the foramen magnum with the lumen of the spinal canal.
It should be noted that currently the optimal method for studying the structures of the posterior cranial fossa is MRI, which, unlike CT, is devoid of artifacts from bone structures.
For ease of analysis, it is customary to distinguish several levels of image acquisition on CT and MR images.
On a CT slice taken along the upper edge of the foramen magnum, the medulla oblongata, meninges, liquor-containing spaces, and vascular structures are differentiated (Fig. 1.3). Sometimes you can see the laterally located lower poles of the cerebellar tonsils (Fig. 1.4).
The cerebellum fills almost the entire volume of the posterior cranial fossa. Its transverse size (90-100 mm) significantly exceeds the anteroposterior one (up to 50 mm). In front, the cerebellum is adjacent to the medulla oblongata, the pons and the quadrigemulus and is connected to them through three pairs of legs. The upper pair of legs goes to the quadrigemulus, the middle one to the pons, the lower one to the medulla oblongata. Identification of zones of pathological density (signal) in these sections allows us to talk about possible damage to one or another leg. Since the cerebellar peduncles are represented by white matter, they are easily differentiated against the background of the denser cerebellar cortex. The cerebellum consists of two hemispheres, between which the vermis is located, which is clearly visualized on CT and MRI sections thanks to the characteristic short convolutions running in the frontal plane parallel to each other. Moreover, the cerebellar vermis has a relatively higher density than the hemispheres. The worm moves obliquely from the bottom back up and forward, which makes it possible to analyze the state of its lower and upper sections. The lower parts of the cerebellum are ventrally adjacent to the medulla oblongata, located on the lower parts of the clivus.
Rice. 1.3. Level of the foramen magnum: a — axial CT section; b — axial MRI section (T1-WI); c — axial MRI section (T2-WI).
1 - opener; 2 - occipital bone; 3 - medulla oblongata; 4 - cerebellum; 5 - maxillary sinus; 6 - large tank; 7 - head of the lower jaw; 8 - mastoid process; 9 - vertebral artery; 10 - nasopharynx; 11 - temporal bone (pyramid).
Rice. 1.4. Level above the foramen magnum: a — axial CT section; b — axial MRI section (T1-WI); c — axial MRI section (T2-WI).
1 - temporal lobe; 2 - slope; 3 - medulla oblongata; 4 - cerebellar hemisphere; 5 - basilar artery; 6 - cerebellar amygdala; 7 - main sinus; 8 - temporal bone; 9 — shaft-lecule; 10 - large tank.
Its dimensions in the longitudinal direction are up to 30 mm, in the transverse direction - up to 20 mm. It has a rounded shape and a median slit along the front and back surfaces. 2 cm higher, the bridge begins to be visualized, in front of which there is the BA, clearly visible against the background of the anterior tank of the bridge (Fig. 1.5). On the sides of the bridge, the apexes and posterior surfaces of the pyramids of the temporal bones are visualized, separated from the latter by the cerebellopontine cisterns. In cross-sections, the image of the bridge resembles a square with rounded corners. Between the brainstem in front and the cerebellum behind is the unpaired fourth ventricle. On axial CT and MRI sections it is localized strictly centrally and has a crescent shape. Its side pockets should normally be strictly symmetrical (Fig. 1.6). The absence of an image of the fourth ventricle, its displacement, deformation, and spherical shape are indirect signs of a pathological process and require further examination. The dimensions of the fourth ventricle are quite variable and do not play a significant role in classifying observations on this basis as normal or pathological. The fourth ventricle communicates through the cerebral aqueduct with the third ventricle. Normally, the water supply is not visualized. There are three openings connecting the IV ventricle with the subarachnoid space - the middle and two lateral, located in the lateral recesses (Fig. 1.7.). These holes cannot be differentiated either normally or during pathological processes in the brain.
Rice. 1.5. Level of the fourth ventricle:
a — axial CT slice; b — axial MRI section (T1-WI); c — axial MRI section (T2-WI).
1 - falx cerebri; 2 - frontal lobe; 3 - lateral gap; 4 - temporal horn of the lateral ventricle; 5 - bridge; 6 - fourth ventricle; 7 - cerebellar vermis; 8 - upper lunar lobule; 9 — orbit; 10 - sphenoid sinus; 11 - pontocerebellar cistern; 12 - middle cerebellar peduncles; 13 - interhemispheric fissure; 14 - basilar artery; 15 - eyeball; 16 - temporal lobe; 17 - cerebellar hemisphere; 18 - eyeball.
It is worth dwelling on the anatomy of the subarachnoid spaces of the posterior cranial fossa (Fig. 1.8). The large cistern of the brain (cerebellomedullary cistern) is identified. It is the space between the medulla oblongata, the bottom of the fourth ventricle and the inferior surface of the cerebellum. Its width is close to 30 mm, and the anteroposterior dimension is 20 mm. Between the base of the skull and the lower surface of the brain, the posterior basal cistern extends from the foramen magnum along the clivus and the dorsum of the sella turcica. Depending on the adjacent anatomical structures, a medial one is distinguished, which runs between the clivus and the pons (width up to 10 mm), and paired lateral (lateral) cerebellopontine cisterns lie in the cerebellopontine angles. The lateral recesses of the fourth ventricle are connected to them through the lateral openings (Lushka). The upper portion of the posterior basal cistern forms the interpeduncular cistern, which must be traced on the corresponding section and located strictly in the middle. Outside the cerebral peduncles lies an enclosing cistern, forming a cerebrospinal fluid-containing space within the tentorial notch (Fig. 1.9). It communicates with the interpeduncular cistern, covers the lateral surfaces of the cerebral peduncles and continues posteriorly into the quadrigeminal cistern, and above it is connected with the pericallosal and paired interhemispheric cisterns.
Rice. 1.6. Level above the fourth ventricle: a - axial CT section; b — axial MRI section (T1-WI); c — axial MRI section (T2-WI).
1 - frontal lobe; 2 - frontal horn of the lateral ventricle; 3 - lateral fissure of the brain; 4 - third ventricle; 5 - cerebral peduncle; 6 - quadrigeminal cistern; 7 - temporal lobe; 8 - superior sagittal sinus; 9 - sickle of the brain; 10 - head of the caudate nucleus; 11—islet cortex; 12 - shell; 13 - internal vein of the brain; 14 - quadrigeminal; 15 - cerebellar hemisphere; 16 - optic nerve; 17 - temporal horn of the lateral ventricle; 18 - hippocampus; 19 - anterior lobe of the cerebellum; 20 - chiasma; 21 - internal carotid artery; 22 - covering tank; 23 - fourth ventricle; 24 - straight gyrus; 25 - olfactory groove; 26 - middle cerebral artery; 27 - worm; 28 - occipital lobe; 29 — fiber of the orbit; 30 - anterior cerebral artery; 31 - interpeduncular cistern.
Between the tentorium and the anterior surface of the cerebellum is the superior cerebellar cistern. The cerebellum is separated from the occipital lobes of the cerebrum by a process of the dura mater, which gives a characteristic hyperdense shadow on CT sections, extending from the upper edges of the pyramids of the temporal bones upward and inward, repeating the shape of the tent, and ends with the tentorial notch, through which the brain stem passes. The presence of liquor-conducting pathways in this area allows one to confidently assess its condition, which plays an important role in the diagnosis of dislocations. On CT sections from above, the bridge borders the midbrain, namely the quadrigeminal.
Rice. 1.7. Level behind the lateral ventricles. Coronal MRI sections: a — T1-weighted image; b — T2-weighted image.
1 - sickle; 2 - precuneus; 3 - pericallosal cistern; 4 - tentorium cerebellum; 5 - superior parietal lobule; 6 - angular gyrus; 7 - interparietal groove; 8 - occipital horn; 9 - parieto-occipital fissure; 10 - lingual gyrus; 11 - superior semilunar lobule; 12 - horizontal slot; 13 - anterior lobe of the cerebellum.
Rice. 1.8. Median sagittal MRI slice: a — T1-weighted image; b — T2-weighted image.
1 - genu corpus callosum; 2 - vault; 3 - funnel; 4 - bridge; 5 - cerebral aqueduct; 6 - quadrigeminal; 7 - medulla oblongata; 8 - spinal cord; 9 - cingulate gyrus; 10 - corpus callosum; 11 - splenium of the corpus callosum; 12 - interpeduncular cistern; 13 - fourth ventricle; 14 - large tank; 15 - cingulate groove; 16 - pericallosal cistern; 17 - lateral ventricle; 18 - anterior cerebral artery; 19 - basilar artery; 20 - paracentral lobule; 21 - precuneus; 22 - wedge; 23 - cistern of the great vein of the brain; 24 - direct sinus; 25 - cerebellar amygdala.
Rice. 1.9. Level of the foramen of the cerebellar tentorium: a — axial CT section after contrast; b — axial MRI section (T1-WI); c — axial MRI section (T2-WI).
1 - sickle; 2 - corpus callosum; 3 - frontal horn; 4 - pillars of the vault; 5 - third ventricle; 6 - pineal gland; 7 - quadrigeminal cistern; 8 - contrasted tentorium of the cerebellum; 9 - superior frontal gyrus; 10 - caudate nucleus; 11 — transparent partition; 12 — leash; 13 - worm; 14 - genu corpus callosum; 15 - shell; 16 - superior temporal gyrus; 17 - vault; 18 - edge of the tentorium; 19 - middle frontal gyrus; 20 - inferior frontal gyrus; 21 — insular cortex; 22 — cavity of the transparent septum; 23 - external occipital gyrus; 24 - middle cerebral artery; 25 - quadrigeminal; 26 - cingulate groove; 27 - head of the caudate nucleus; 28 - globus pallidus; 29 - temporal horn of the lateral ventricle.
The posterior contour of the lower colliculi in the form of a broken line, emphasized by the quadrigeminal cistern, allows one to confidently differentiate this zone. Slightly above and anterior to the quadrigeminal peduncle are located the cerebral peduncles in the form of two diverging short, rather thick oblong formations, between which passes the interpeduncular cistern, which has a triangular shape with the apex facing posteriorly.
Treatment
This type of neoplasm requires a special approach. Doctors seek to remove most thickenings in order to improve the person’s condition. But brain intervention always carries serious risks, so it is prescribed only in the most severe cases.
Therefore, most often they try to limit the growth of the cyst and reduce the unpleasant symptoms experienced by the patient. Drug treatment is prescribed in most cases.
Drug therapy
After completing diagnostic measures, the doctor chooses treatment tactics. It is aimed at preventing the growth of the cyst. In addition, it contributes to the achievement of the following goals:
- resorption of adhesions that appear due to the progression of pathology;
- ensuring proper functioning of the circulatory system;
- saturation of brain cells with oxygen and necessary components;
- lowering cholesterol;
- normalization of blood pressure levels;
- maintaining blood clotting;
- combating pathogens of dangerous infections (if they are present);
- maintaining a high level of immunity;
- antioxidants should increase cell resistance to increased pressure.
The attending physician decides how long the rehabilitation will last. The patient should not independently discontinue medications or change the established daily dosage.
Surgery
Doctors put off surgical intervention until last. It is prescribed when medications do not cope with their tasks. The operation is associated with a high risk of damage to brain structures, so it is prescribed in specific cases:
Microneurosurgery is used.
- coordination of movements is increasingly impaired;
- cancer cells have been identified;
- the patient suffers from severe cramps;
- the tumor is constantly increasing in size;
- there is a possibility of cerebral hemorrhage.
The intervention is carried out using one of three main methods. Microneurosurgery is used, which requires opening the skull. The accuracy of capsule removal is guaranteed, but the risk of damage to healthy tissue is also higher.
The endoscopic method minimizes the risk of complications and also shortens the recovery period. The third type of operation is bypass surgery. With it, a catheter is inserted into the cavity, through which the contents of the capsule are pumped out. However, it cannot be kept for a long time, otherwise there is a possibility of penetration of pathogenic pathogens.
What it is
Benign meningioma arises from the dura arachnoid membrane of the brain or the stroma of a plexus of blood vessels. The neoplasm is characterized by a change in the cranial shape in the affected area or protrusion of the defect into significant bumps.
The disease affects the surfaces of the large hemispheres, the anterior and posterior fossae of the skull, the cerebellar zone, the sphenoid or temporal bones.
Meningioma is characterized by slow growth, so surgical intervention often gives a positive result. However, the tumor is prone to recurrence. If malignant transformation occurs, the neoplasm grows into bone structures, nearby tissues and brain matter.
On this topic
- central nervous system
How does a headache with a brain tumor hurt?
- Natalya Gennadievna Butsyk
- December 3, 2021
In addition, metastases often occur. If the pathology grows towards the brain side, then a node forms and the adjacent substance is compressed.
Most often, meningioma develops in middle age. Moreover, women are more susceptible to the disease than men, while in children and adolescents this tumor is diagnosed extremely rarely.
Folk remedies
Traditional recipes help curb tumor growth. However, they should not be used thoughtlessly. Before using any product, you must obtain the approval of your physician. Otherwise, you may not improve the condition, but only provoke the development of complications.
Traditional recipes can be used during the recovery period, but not in the acute stage. They are used only in combination with medications prescribed by a doctor. To slow down the growth of a tumor, the following means are used:
- spotted hemlock. It is used alone or in combination with elderberry and violet;
- tea from viburnum, rowan or horsetail helps stabilize blood pressure, which has a positive effect on the patient’s condition;
Viburnum tea stabilizes blood pressure levels. - fresh vegetables (celery, asparagus, etc.) help strengthen the immune system and give strength to fight pathology.
Prevention
If we talk about the prevention of congenital neoplasms, then a pregnant woman should lead a correct lifestyle. You need to give up bad habits and avoid emotional stress. It's important to eat right. If the body does not receive enough nutrients with food, it is necessary to additionally consume vitamin complexes designed for pregnant women.
Secondary tumors can also be prevented. To do this, follow the general recommendations:
Monitor your blood pressure readings.
- diseases associated with the nervous system require prompt treatment. Their nature does not matter - infectious, vascular, etc.;
- undergoing a routine examination by a doctor. If you experience any disturbing symptoms, even minor ones, consult your doctor immediately;
- don't let yourself freeze. It's about the head - always wear a hat;
- monitor your blood pressure and take medications if it changes;
- watch your cholesterol;
- minimize the likelihood of developing infectious diseases, avoid contact with sick people;
- get rid of bad habits.
Neoplasms in the cerebellum usually require immediate treatment. In newborns, they can resolve spontaneously. But adults need to take medications under the supervision of a physician. In the most severe cases, surgical intervention is prescribed.
Rehabilitation after removal
As a result of the fact that during its formation, malignant or benign meningitis has a negative effect on the functioning of the brain, after surgery the tissues require a certain amount of time to restore their functions.
The rehabilitation period, depending on the patient’s well-being, lasts from several weeks to six months. Physical therapy and additional procedures are prescribed to restore the nervous system.
In addition, depending on the patient’s condition, the following is prescribed:
- Acupuncture . Necessary for activating the nervous system and restoring sensitivity of the lower extremities. It also helps get rid of numbness.
- Medications . To prevent tumor recurrence. Medications are often prescribed to lower blood pressure, which may occur after surgery. Under certain circumstances, replacement therapy is required.
- Exercise therapy . The duration of recovery also depends on the efforts the patient puts in. Physical exercise helps to gradually restore lost mobility of the limbs and other body functions. Classes are held in the swimming pool.
To achieve the best results, complex therapy is used. This helps you recover faster and significantly reduces the risk of recurrence of the tumor.