A hematoma forms in the brain due to rupture or mechanical damage to the vascular wall. As a result, hemorrhage occurs in nearby brain structures. Acute cerebrovascular accident ranks 2nd among causes of mortality and 1st among pathologies that lead to disability. Stroke (an acute disturbance of blood flow in the brain) occurs with a frequency of 3 cases per 1 thousand population annually. Every third case ends in death. Intracerebral hematomas account for 10% of the total mass of all forms of stroke, subarachnoid hemorrhages – 4%.
Causes
Bleeding inside the cranial cavity occurs for many reasons. This could be a head injury, accompanied by a brain contusion, or a fracture of the skull. Many vascular diseases lead to thinning of their walls. Strong blood pressure helps fill the empty space in the skull and compress brain tissue.
Hemorrhagic stroke, vascular damage due to atherosclerosis, angioedema disorders also lead to such consequences. Blood can accumulate due to damaged capillaries suffering from an increased level of permeability.
Other causes of intracranial hematoma include brain tumors or past infectious diseases, blood and liver diseases, taking medications such as anticoagulants, or one of the autoimmune diseases.
Signs of a hematoma formed
With an intracranial hematoma, symptoms may not be felt immediately. This is its main danger. Also, due to different types of blood accumulation and the age characteristics of a person, the signs are of a different nature.
With hematomas located between the skull bone and the lining of the brain, manifestations very quickly make themselves felt. A person feels severe oppressive pain, a constant feeling of drowsiness, and there is confusion in consciousness. Epileptic seizures or muscle paralysis occur. People may suddenly lose consciousness. If such a cavity has a volume of 150 ml or more, then the person will die.
There are hematomas that are caused by a ruptured vein. Symptoms appear very slowly. In babies, the volume of the head may gradually increase. Nausea and vomiting occur. There are convulsions and fainting. The pupil of the eye may expand on the side of the hematoma. If an aneurysm ruptures in the head, the resulting sharp pain sensation resembles a stab with a knife.
Common to all types of hemorrhages are pain in the head, nausea and vomiting, frequent dizziness, sometimes slowness of speech and confusion in consciousness. The pupils of the eyes have different sizes. Constant drowsiness and weakness in the arms and legs on one side of the body. With particularly strong accumulations of blood, a person falls into a coma and experiences frequent convulsive attacks.
The most reliable symptom is loss of consciousness and periods of lucidity, when it seems that it has become much easier. Blood pressure readings may also jump (hypertension, bradycardia, epileptic seizures).
If you discover an intracranial hematoma according to the signs described above, you should immediately go to the hospital for advice. Delay can have a detrimental effect on the vital functions of the body.
Clinical picture of the pathology
How to determine that an intracranial hematoma has formed? Symptoms of the pathology depend on the type of hemorrhage. Thus, signs of an epidural hematoma include severe headache, convulsions, impaired consciousness and drowsiness. When studying the reaction of the pupils to light, anisocoria is noted. Later, paralysis of the limbs occurs. Signs of an intracranial hematoma are detected within several hours or days from the moment of damage to the artery. In children, symptoms develop more quickly.
Subdural hematoma is characterized by the following clinical picture:
- headache predominates;
- nausea and vomiting that does not bring relief;
- meningeal signs;
- Convulsive seizures are sometimes observed.
The symptoms of intracerebral hemorrhage are similar. In contrast to the signs of a subdural hematoma, the pain covers one side of the head, and loss of consciousness is noted. Intracerebral hemorrhage often leads to paralysis of the limbs.
Diapedetic hematomas are characterized by constant headaches. They are the most difficult to identify because they are small in size.
Types of cranial hematomas
Intracranial hematomas differ according to the relative extent of their manifestations, size and location in the head. They are localized near the brain itself, the bones of the skull and membranes.
By time they are divided into acute, subacute and chronic. In an acute process, signs appear within the first few days. Subacute - within 3 weeks, and chronic - even later.
The size of hematomas is also of great importance when providing assistance. Small blood accumulations are up to 50 ml, medium ones reach 100 ml, and large ones have a volume of over 100 ml.
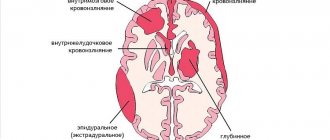
The location of blood tumors is also different:
- Epidurals are located above the dura mater of the brain;
- Between the gray matter itself and its membrane are the subdurals.
- They also distinguish between intracerebral and intraventricular. These hematomas are located directly in the substance of the brain.
- There are hematomas formed near the brain stem.
Hematomas also form during hemorrhagic impregnation. In this case, the walls of the vessels are in an intact state.
Diagnosis of hematoma inside the skull
Intracranial traumatic hematomas are diagnosed first of all, since in most cases people seek medical help after receiving injuries. It is more difficult to detect hemorrhages that occur against the background of vascular diseases. Diagnostic methods include:
- Computed tomography of the brain.
- X-ray examination of the skull.
- Magnetic resonance imaging.
To conduct a differential diagnosis of headaches, ultrasound of blood vessels with Dopplerography, EEG, and echoencephalography are performed.
How is diagnosis carried out?
Detecting blood clots in the brain is not easy. If an intracranial hematoma is suspected, diagnosis begins with a fluoroscopic image. Such a study is relevant if there has been a head injury. The purpose of this study will be to identify skull fractures, cracks and bone fragments.
In case of intracranial hematoma, studies are also carried out using MRI (magnetic resonance therapy) or CT (computed tomography). Such methods make it possible to obtain detailed information about the state of the brain, obtaining its image from different angles.
The examinations are completely painless. Images are produced using a magnet and radio waves. They may also prescribe echoencephalography of the head.
What is an intracranial hematoma?
Symptoms that occur with an intracranial hematoma develop due to compression of the brain by blood. Left untreated, severe damage to the central nervous system can occur. The danger of the disease is that signs of pathology appear gradually.
So, what is a hematoma inside the skull? Due to various reasons, hemorrhage from the vessels of the head may occur. As a result, a so-called bruise in the meninges is formed - a hematoma. Unlike hemorrhages in soft tissues and skin, it resolves very slowly. Only small hematomas can disappear on their own. For medium and large hemorrhages, surgical intervention is necessary.
When should you rush to the doctor?
If the blow to the head was so significant that there was loss of consciousness, then you should immediately go to the doctor. After all, symptoms do not always appear immediately. Knowing the signs of a hematoma, the victim should monitor his condition and be sure to tell his family or colleagues, since consciousness is often impaired and memory loss may occur. The person who received the blow may not even remember it.
Therefore, relatives also need to be attentive and monitor changes in the patient’s condition. At the first manifestations of a hematoma, you need to rush to the doctor and undergo the necessary examination. After all, any intracranial hematoma poses a threat to life.
Treatment
Such hemorrhages can only be removed surgically. The type of operation is selected by the doctor depending on the location, size and nature of the hematoma. If the blood is in a liquid state and collected in a certain place, then during the operation the surgeon makes a burr hole in the skull and the blood is sucked out.
If the hematoma is large and clots have formed in the cavity, then craniotomy is performed. During the operation, the cavity is cleaned in an open state.
There are small subdural hematomas that are asymptomatic and do not require surgical intervention. They are treated with diuretics and corticosteroids. It is necessary to monitor the patient's condition to exclude cerebral edema.
Carrying out surgery
In most cases, surgical removal of an intracranial hematoma is indicated. It involves the evacuation of blood. For this purpose, the following types of surgical interventions are performed:
- Osteoplastic trepanation. It is characterized by making a small hole in the skull and removing blood clots with special instruments and a vacuum device.
- Stereotactic intervention. Blood is removed from the cranial cavity using a special cannula.
- Puncture-aspiration removal of hematoma. It involves inserting a thin catheter.
The method of surgical treatment is selected by the neurosurgeon, depending on the size of the hemorrhage, concomitant pathologies and the age of the patient.
Postoperative rehabilitation
Cramps are common after this type of surgery. They can begin even a year after the injury. This is accompanied by memory loss, lack of attention, and headaches. After severe injuries and lengthy operations, the rehabilitation period is always long.
But if you have patience and follow all the doctor’s recommendations, you can recover completely within six months. For children, this process takes much less time. You need to rest more time and not be overloaded during the day. Driving and playing sports are prohibited during the recovery period. Alcohol is also strictly prohibited.
Since consciousness and memory may have lapses, you cannot make important decisions; everything needs to be written down and consulted with loved ones.
Consequences of hematoma
After the formation of an intracranial hematoma, consequences can occur even after a successful operation. Residual effects appear for a long time. These are dizziness, amnesia (partial or complete loss of memory), pain in the head, weakness throughout the body. Often, traumatic brain injury results in complications such as epilepsy. So, after the first attack you need to start taking appropriate medications.
A common consequence of traumatic brain injury and brain surgery is a decrease in intelligence, which gets worse over time. But this is only in difficult cases, if the hematoma was large. The consequences also depend on the location of the accumulated blood in the brain.
Subdural hematoma
Subdural hematomas are an accumulation of blood in the space between the dura mater and the arachnoid membrane of the brain. It can occur in any age group, the main cause being traumatic brain injury. A CT scan is sufficient to make a diagnosis. The prognosis varies widely depending on the size and duration of the hemorrhage. More than >70% of subdural hematomas have other important injuries: SAH, DAP, contralateral contusions.
Epidemiology
Subdural hematomas occur in all age groups:
- In children, accidental injury is more common,
- in young people: road traffic accidents,
- in older people: falls (there may be no obvious history of injury),
- occur in ~15% of all head injury cases,
- occur in 30% of fatal head injuries.
Clinical picture
Acute subdural hematomas usually occur with traumatic brain injury, especially in young patients, where they are combined with brain contusions. In the majority of patients (65-80%), subdural hematomas are accompanied by severe depression of consciousness and abnormalities of the pupillary reflex. The clinical manifestations of subacute/chronic subdural hematomas in elderly people with no or minor history of head trauma are often vague and are one of the classic causes of pseudo-dementia.
Pathology
Subdural hematomas occur when the bridging veins located in the subdural space are stretched and ruptured when exposed to sudden shearing forces during injury. The arachnoid membrane can also be damaged, causing blood to accumulate between the arachnoid and dura mater. In 10 - 30% of chronic subdural hematomas there are repeated hemorrhages. Rebleeding usually occurs when overstretched cortical veins rupture as they traverse an enlarged, filled subdural space, or from a vascularized pseudocapsule. Subdural hematomas are located between the dura mater and the arachnoid membrane. As a rule, they are ribbon- or crescent-shaped and are more extensive than epidural hematomas. Unlike an epidural hematoma, subdural hematomas are not limited to the sutures of the skull, but are limited to the falx cerebri and tentorium cerebellum.
Diagnostics
In adults, 85% of subdural hematomas are unilateral. In young children, 75-85% are bilateral. Typical locations for subdural hematomas are the frontoparietal regions and the middle cranial fossa. Interhemispheric subdural hematomas are more common in children with non-road traffic injuries. In the vast majority of cases, CT is sufficient to make a diagnosis. Contrast administration is sometimes useful when subdural empyema is suspected, when a small isodense subdural hematoma is suspected, or when attempting to differentiate enlarged subarachnoid spaces from chronic subdural hematoma.
X-ray of the skull
If available, CT or MRI modalities are inappropriate, useless and even harmful.
CT scan
The whirlpool sign is a sign of active bleeding. Manifestations of a subdural hematoma on CT depend on the duration and degree of organization of the hematoma - on average, the density of a subdural hematoma decreases by 1.5 HU per day.
Acute subdural hematoma
In most cases, the examination of patients is carried out later than the acute phase (the first hour), but in cases where the examination is performed during this period, subdural hematomas appear at a relatively isodense density in relation to the cerebral cortex, with heterogeneity in the form of swirls, due to a mixture of blood clots and the continued flow of unclotted blood. The degree of cerebral edema (especially in young patients in whom traumatic brain injury is often more severe) affects the volumetric effect; there is no direct relationship between the size of the subdural hematoma and the degree of dislocation [2].
Acute subdural hematoma
The classic presentation of an acute subdural hematoma is a homogeneous, hyperdense, extra-axial, ribbon- or crescent-shaped zone that extends widely along the convex of the cerebral hemisphere. As the blood clots, the density of the hematoma increases, usually to > 50-60 HU, thus the hematoma is hyperdense in relation to the cerebral cortex [2]. Up to 40% of subdural hematomas have mixed hyper- or hypodense density, due to uncoagulated blood and plasma. Rarely, acute subdural hematomas may be isodense in density to the cerebral cortex, as occurs in coagulopathies or severe anemia when the hemoglobin concentration drops to 8 to 10 g/dL.
Subacute subdural hematoma
Over time, due to protein degradation, the density of blood clots decreases. In the period from 3 to 21 days (usually 7-14 days), the density decreases to ~30 HU and the hematoma becomes isodense with respect to the cerebral cortex, which makes diagnosis difficult, especially if there are bilateral subdural hematomas [2]. Contrast-enhanced CT is useful when MRI is not available. The key points in diagnosis are a number of indirect signs:
- CSF grooves do not reach the skull bones
- volumetric effect including smoothing of grooves and lateral dislocation of median structures
- apparent thickening of the cortex
Chronic subdural hematoma
Eventually the subdural hematoma becomes hypodense and may reach ~0 HU, it may be isodense to the CSF and may simulate a subdural hygroma.
Repeated acute hemorrhage in a chronic subdural hematoma
Repeated acute hemorrhage into a chronic subdural hematoma is an episode of acute hemorrhage into a pre-existing chronic subdural hematoma. It appears as a hypodense accumulation with levels. May occur in patients with bleeding disorders or taking anticoagulants [2].
Magnetic resonance imaging
Manifestations are usually caused by the biochemical properties of hemoglobin, which vary depending on the timing of the hematoma. The most sensitive is the FLAIR sequence.
Hyperacute subdural hematoma
- T1: isointense signal relative to the signal from the gray matter of the brain
- T2: signal intensity varies from iso- to hyperintense
- FLAIR: hyperintense signal relative to the CSF signal
Acute subdural hematoma
- T1: signal intensity varies from iso- to hyperintense, relative to the signal from the gray matter of the brain
- T2: signal hypointense relative to gray matter
- FLAIR: hyperintense signal relative to the CSF signal
Subacute subdural hematoma
May have a biconvex shape in the frontal plane rather than the crescent shape that is typical in the axial plane
- T1: usually has a hyperintense signal due to the presence of methemoglobin
- T2: usually hyperintense signal
- FLAIR: hyperintense signal
Chronic subdural hematoma
- T1: isointense signal, relative to the signal from the CSF
- with repeated bleeding or infection may have a hyperintense MR signal
- isointense signal, relative to the signal from the CSF
Differential diagnosis
See also the article Differential diagnosis of subdural and epidural hematomas
The main nosologies for differential diagnosis include [1-2]:
- expansion of subarachnoid spaces due to brain atrophy may look similar
- no volumetric effect
- vessels pass through spaces rather than being displaced towards the brain
- CT contrast aids in visualization by highlighting the course of the vessels as well as demonstrating the enhancing "capsule" of the subdural hematoma/empyema
- has similar manifestations on non-contrast images
- differential diagnosis for small sizes is sometimes difficult
- may be indistinguishable on CT from a chronic subdural hematoma