Causes of subdural hematoma
A subdural hematoma is usually called one of the types of blood accumulation in the brain.
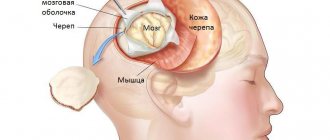
The name “subdural” means that the localization of the hematoma is limited to the dura mater and arachnoid mater. In addition, epidural, intracerebral and intraventricular intracranial hematomas are distinguished. It is intracranial hematomas that are the most common cause of compression of the brain during traumatic brain injury. They are also a consequence of that same traumatic brain injury. Among the next most popular causes of subdural hematomas are cerebral vascular pathologies and medications. Among vascular pathologies, special attention is paid to hypertension, arterial aneurysms, arteriovenous malformations; Of the medications, the most unfavorable are anticoagulants (used to prevent blood formation and change the activity of the blood coagulation system).
Among victims with TBI, acute subdural hematoma accounts for 1-5%, reaching 9-22% if severe TBI occurs. Among the variety of hematomas, it is subdural ones that take first place, and isolated ones account for up to 2/5 of the total number of intracranial hemorrhages. Among men, this pathology is three times more common than among women. Although injuries and the resulting pathology occur among any age-related pathologies, people over 40 years of age are at greater risk.
The basis for the formation of a subdural hematoma is head trauma of varying severity. For the formation of an acute subdural hematoma, the TBI must be quite severe, and for chronic and subacute injuries, relatively mild injuries are sufficient. It is noteworthy that a subdural hematoma (as opposed to an epidural) can form not only directly in the injured area of the head, but also on the opposite side. There are several mechanisms for the formation of subdural hematomas:
- homolateral
- due to the impact of a traumatic agent with a small application area on a stationary or sedentary head; local contusion of the brain and rupture of pial or cortical vessels in the area of injury occurs.
- due to displacement of the brain when the head, which is in relatively rapid motion, hits a massive stationary or inactive object (fall from a relatively high height, from a moving vehicle onto the pavement, collision with cars, motorcycles, falling backward, etc.); there is a rupture of the bridge veins flowing into the superior sagittal sinus.
- due to the impact of a traumatic agent with a wide area of application on a fixed head (impact from a log, a falling object, a block of snow, the side of a car, etc.); What occurs is not so much a local deformation of the skull as a displacement of the brain, rupture of the veins flowing into the sagittal sinus.
Often, different mechanisms are simultaneously involved in the formation of subdural hematomas, which explains the significant frequency of their bilateral location.
The clinical picture with the development of subdural hematomas consists of general cerebral, local and secondary brainstem symptoms. This is due to compression and dislocation of the brain with the development of intracranial hypertension. In understanding the symptoms of this pathology, special attention should be paid to the presence of a “light” gap. This is the period after injury in which there are no clinical manifestations of subdural hematoma. Its duration varies within very wide limits - from several minutes and hours (with acute development) to several days (with subacute development) and weeks, months, years (with chronic development). The onset of pronounced clinical manifestations is provoked by a variety of factors:
- additional, secondary trauma,
- surges in blood pressure.
With subdural hematomas, undulation and gradual changes in the state of consciousness are usually pronounced. However, there are cases when patients suddenly fall into a coma, as with epidural hematomas. Often the development of symptoms with a subdural hematoma occurs in three phases, but not always. These are the following three phases:
- primary loss of consciousness after injury,
- its restoration for some period,
- subsequent re-shutdown.
Unlike epidural hematomas, in which disturbances of consciousness occur mainly of the stem type, with subdural hematomas, especially subacute and chronic ones, disintegration of consciousness according to the cortical type is often noted with the development of:
- amental, oneiric, delirium-like conditions,
- memory impairment with features of Korsakov's syndrome,
- “frontal psyche” with a decrease in criticism of one’s condition,
- spontaneity,
- euphoria,
- behavioral disorders.
In the clinical picture of subdural hematomas, psychomotor agitation is often noted, epileptic seizures are possible, and generalized convulsive paroxysms predominate. Plastic changes in muscle tone, general stiffness and slowness of movements, reflexes of oral automatism and a grasping reflex are detected.
A constant symptom of pathological development is headache; it has a shell-like hue (irradiates to the eyeballs, the back of the head, occurs with eye movements, and is accompanied by photophobia). Cephalgia, among other things, is characterized by local pain upon percussion of the skull, a diffuse hypertensive nature, and a feeling of “fullness.” The period of increased headaches with subdural hematoma is often accompanied by vomiting.
Among the focal signs of subdural hematomas, the most important role is played by unilateral mydriasis with a decrease or loss of the pupil’s reaction to light. Dilation of the pupil on the side opposite the hematoma is noted much less frequently; it is caused by a bruise of the opposite hemisphere or pinching of the cerebral peduncle opposite the hematoma in the foramen of the cerebellar tentorium. In acute subdural hematoma, extreme dilatation of the homolateral pupil with loss of its reaction to light predominates. In subacute and chronic subdural hematomas, mydriasis is often moderate and dynamic.
Pyramidal hemisyndrome in acute subdural hematoma, in contrast to epidural hematoma, is inferior in diagnostic significance to mydriasis. If pyramidal hemisyndrome reaches the degree of deep paresis or paralysis, there is reason to suspect a concomitant brain contusion. The bilaterality of pyramidal and other focal symptoms may be due to the bilateral location of subdural hematomas. Sensitivity disorders are significantly inferior in frequency to pyramidal symptoms. The proportion of extrapyramidal symptoms in subdural hematomas, especially chronic ones, is relatively large.
The classic variant of subdural hematoma is rare, but it is described in detail. At the time of TBI, a short loss of consciousness is noted, during the recovery of which only moderate stupor or its elements are observed. The light period lasts 10-20 minutes, and sometimes several hours, extremely rarely 1-2 days. Patients may experience headache, nausea, and dizziness. Along with the relative adequacy of behavior and orientation in the environment, rapid exhaustion and slowdown of intellectual-mnestic processes are noted. Focal neurological symptoms are absent or minimal. The next phase is characterized by deepening stupor and the appearance of increased drowsiness and psychomotor agitation. The patient's inadequacy becomes noticeable, the headache sharply intensifies, and repeated vomiting occurs. Focal dislocation symptoms are clearly manifested in the form of homolateral mydriasis, contralateral pyramidal insufficiency and sensitivity disorders. Along with the loss of consciousness, a secondary brainstem syndrome develops with bradycardia, increased blood pressure, changes in breathing rhythm, bilateral dysfunction of the vestibular apparatus and oculomotor reflexes, and tonic convulsions.
A variant of a subdural hematoma with an erased “light” space is typical for a hematoma due to severe brain contusions. Here, the primary loss of consciousness can easily develop into a cerebral coma. Focal and brainstem symptoms caused by primary brain damage are pronounced. Subsequently, a partial restoration of consciousness is noted. In a victim who has emerged from a coma, psychomotor agitation and a search for antalgic poses are sometimes noted. It is often possible to detect a headache and meningeal symptoms. This period lasts from several minutes to a day, and is replaced by repeated switching off of consciousness to the point of stupor or coma with the development of dislocation stem symptoms.
Option without a “light” gap. A very common variant of subdural hematoma, typical of multiple severe brain injuries. Stupor (and more often coma) from the moment of injury to surgery or death of the patient does not undergo any significant positive dynamics.
Chronic subdural hematomas are characterized by the formation of a certain capsule that exists autonomously with the brain and determines all subsequent pathophysiological and clinical dynamics.
Forms
Depending on how long the clear interval lasts and the presence of the clinical picture, a subdural hematoma of the brain can be of different types:
- Spicy. Its development occurs within three days after injury. The problem arises when the brain has been exposed to severe and severe stress.
- Sub-acute. This pathological process develops over a period of four days to two weeks. In this situation, a small vessel is damaged as a result of a mild traumatic effect. Therefore, the amount of blood that pours into the space between the brain and the skull is not much and the increase in volume occurs slowly.
- Chronic. Occurs over several weeks or months. The development of pathology can even take years. The role of trauma in this case is secondary. Typically, chronic forms occur with cerebral vascular diseases.
Depending on the form of the disease, appropriate treatment methods are selected.
How to treat subdural hematoma?
Treatment of subdural hematomas can be carried out using conservative and surgical methods. The choice of tactics is determined individually, taking into account the volume of the hematoma, the phase of its development and the patient’s condition.
The absolute indications for surgical treatment of subdural hematomas are:
- acute subdural hematoma, causing compression and displacement of the brain; the sooner the subdural hematoma is removed, the more favorable the prognosis for recovery;
- subacute subdural hematoma with increasing focal symptoms and/or signs of intracranial hypertension.
Any other circumstances may be grounds for surgery only at the discretion of the attending physician, taking into account the totality of clinical and radiological data.
Drug treatment of subdural hematoma is relevant:
- for victims in clear consciousness:
- if the hematoma thickness is less than 10 mm,
- when the midline structures are displaced by no more than 3 mm,
- without compression of the basal cisterns;
Resorption of a planar subdural hematoma usually occurs within a month.
In some cases, a capsule forms around the hematoma, which means the process becomes chronic. If dynamic observation indicates a deterioration in the patient’s condition or an increase in headaches, or congestion occurs in the fundus, this turns out to be an indication for surgical intervention, or more precisely for closed external drainage.
What diseases can it be associated with?
In approximately half of the cases with subdural hematomas, bradycardia is recorded. Congestion in the fundus is a common component of compression syndrome. In the chronic course, there is a decrease in visual acuity and elements of optic disc atrophy. It should be noted that due to severe concomitant brain contusions, subdural hematomas, especially acute ones, are often accompanied by brainstem disorders in the form of respiratory disorders, arterial hyper- or hypotension, early hyperthermia, diffuse changes in muscle tone and reflex sphere.
Often, a change in pupil diameter with a subdural hematoma is accompanied by ptosis of the upper eyelid on the same side; this is combined with limited mobility of the eyeball and most often indicates a craniobasal radicular genesis of oculomotor pathology.
Symptoms of the problem
The symptoms of a subdural hematoma are highly variable and depend on a combination of different factors. Among the signs of this condition in adults are :
- difficulty with balance when walking;
- headache;
- drowsiness;
- nausea and vomiting;
- loss of consciousness;
- numbness in the limbs;
- panic attacks;
- speech problems;
- vision problems.
In children, manifestations may be as follows::
- bulging fontanelle;
- refusal to eat;
- coordination problems;
- increase in head circumference;
- drowsiness and lethargy;
- irritability;
- vomit.
Doctors say that often the symptoms of a subdural hematoma resemble a stroke. If a person experiences any of these conditions—decreased cognitive ability, a headache that lasts several hours, an inability to speak, or slurred speech—they should seek help as soon as possible.
Risk factors for the development of such a hematoma are:
- anticoagulants;
- long-term alcohol abuse;
- poor nutrition, which contributes to blood thickening and blood clots;
- smoking;
- obesity;
- diabetes;
- atherosclerosis, etc.
Treatment of subdural hematoma at home
Surgical treatment of a subdural hematoma should be carried out as soon as possible after the injury or with clinical observation of the patient during conservative treatment if the latter has no effect.
When conservative treatment is chosen, hospitalization will not be superfluous, since it is in a hospital setting that it is easiest to meet all the conditions for a successful recovery:
- bed rest,
- long-term use of medications that resolve hematomas (and they can cause a number of complications),
- maximum control by medical personnel, because there is a considerable risk of deterioration of the neurological status.
Diagnostics
According to ICD-10, subdural hematoma is defined as “traumatic subdural hemorrhage” and has code S06.0. This formulation is very often used by specialists, and the diagnosis can be described in the medical record in this way.
First of all, the doctor interviews the patient, finding out his complaints, existing symptoms, time of injury and clinical course of the disease. If a person is unconscious, all data should be clarified from eyewitnesses of the incident. An external examination is also very important, during which characteristic signs of a traumatic brain injury are identified.
For a more reliable diagnosis, instrumental methods are used that can be used to visualize hemorrhage and determine its nature. These methods include computed and magnetic resonance imaging, electroencephalogram, and X-ray of the brain.
Treatment of other diseases starting with the letter - s
| Treatment of salmonellosis |
| Treatment of cutaneous sarcoidosis |
| Treatment of pulmonary sarcoidosis |
| Treatment of Kaposi's sarcoma |
| Treatment of uterine sarcoma |
| Treatment of Ewing's sarcoma |
| Treatment of type 2 diabetes mellitus |
| Treatment of type 1 diabetes mellitus |
| Treatment of seborrhea |
| Treatment of sepsis |
| Treatment of heart failure |
| Treatment of anthrax |
| Treatment of Budd-Chiari syndrome |
| Treatment of Guillain-Barré syndrome |
| Treatment of Gilbert's syndrome |
| Treatment of Parhon's syndrome |
| Treatment of polycystic ovary syndrome |
| Treatment of empty sella syndrome |
| Treatment of irritable bowel syndrome |
| Treatment of Sjögren's syndrome |
| Treatment of sinusitis |
| Treatment of systemic lupus erythematosus |
| Treatment of systemic scleroderma |
| Treatment of systemic sclerosis |
| Treatment of syphilis |
| Treatment of scoliosis |
| Treatment of somatoform disorders |
| Treatment of spinal stroke |
| Treatment of spondylosis and spondyloarthrosis |
| Treatment of laryngeal stenosis |
| Treatment of tracheal stenosis |
| Treatment of stenosing ligamentitis |
| Treatment of tetanus |
| Treatment of stomatitis |
| Treatment of ringworm |
| Treatment of subarachnoid hemorrhage |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.