More useful information about other diseases starting with the letter “K” here: Causalgia, Brain cyst, Cluster headache, Tick-borne encephalitis, Kozhevnikov epilepsy, Colloid cyst of the third ventricle, Coma, Compressive myelopathy, Balo concentric sclerosis, Radicular syndrome, Corticobasal degeneration, Craniovertebral anomalies, Craniospinal tumor, Craniopharyngioma, Myasthenia gravis crises, Hemorrhage into the ventricles of the brain.
What does hemorrhage into the ventricles of the brain mean?
Hemorrhage into the ventricles of the brain is a disease that is one of the forms of malfunction of the circulatory system of the brain. The presented disease is most often diagnosed in modern medicine. Neurologists say that the disease is caused by arterial hypertension (the treatment of which has been neglected for a long time), bad habits (smoking, alcoholic beverages, drugs) and the use of pharmacological agents that can lead to poor blood clotting. To establish a conclusion, the doctor conducts a detailed conversation with the patient, finds out existing complaints and problems, and also prescribes a certain list of tests for a final affirmative diagnosis. Therapeutic treatment helps eliminate the formed edema, stabilize lung function and normalize blood pressure.
Classification
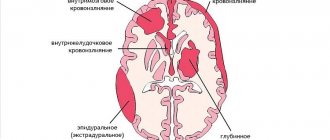
Blood from the vessels can pour directly into the brain tissue, ventricles or under the membranes. Mixed variants with the formation of several lesions are possible. Thus, according to localization, intracerebral hemorrhage occurs:
- Parenchymal (damage to brain tissue).
- Into the ventricles.
- Subarachnoid (under the arachnoid membrane).
- Subdural (under the dura mater).
- Epidural (blood accumulates under the bones of the skull, above the hard shell).
- Mixed.
Brain
Parenchymal intracerebral hemorrhage can also be divided into types:
- damage to the frontal, temporal, parietal, occipital lobes;
- subcortical (in the hemispheres);
- damage to the stem region.
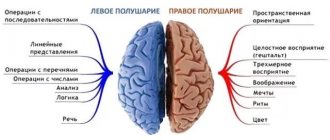
The localization of cerebral hemorrhage directly affects the characteristics of symptoms and the severity of consequences. The stem section, for example, contains centers responsible for vital functions, so damage to this area can result in death.
Intracranial hemorrhage is extremely dangerous, especially when a hematoma forms in the area of vital centers or blood flows into the ventricles. This condition may be accompanied by compression or dislocation of brain structures, which leads to serious consequences (coma, death).
Brief information
In neurology, a similar disease of hemorrhagic type is classified as stroke. The anomaly has different names. According to surveys and average statistical information received from practicing doctors, the described deviation from the norm ranks first in the number of deaths of patients around the globe. Based on publicly available information, such a process can cause death within 48 hours of onset in 60% of cases. The risk increases significantly during the recovery period after a stroke. People who survive a critical attack have a 90% chance of bleeding.
Basically, the largest number of recorded pathologies is observed in the population of retirement age, whose age has exceeded the mark of 50 years. However, in addition to this, danger threatens not only people with arterial hypertension, but also any other abnormalities that have absolutely nothing to do with the level of pressure.
Causes, risk factors
There are always reasons that caused this or that disease. Hemorrhage is no exception and does not occur just like that. There are always factors that increase the risk of developing the disease.
Causes
The problem has been well studied by doctors. Therefore, they were able to accurately compile a list of possible reasons why people bleed. However, even this knowledge does not provide guaranteed ways to protect yourself in the future. Cerebral hemorrhage has the following causes:
- Inflammation of blood vessels;
- Vascular aneurysms;
- Arteriovenous malformations;
- Dystrophic changes in the walls of blood vessels;
- Cerebral atherosclerosis;
- Arterial hypertension;
- Blood diseases;
- Blood clotting disorders in other diseases;
- Liver cirrhosis with blood clotting disorders;
- Hemorrhages occurring inside the brain tumor;
- Taking anticoagulants, antiplatelet agents, fibrinolytics;
- Traumatic brain injuries, blows to the head (for example, in an accident);
- Birth injury.
None of the above reasons is a guarantee that a person will have a hemorrhage. However, you should pay special attention to your health.
Risk factors
There are not only main reasons, but also predisposing ones. They can have minimal negative effects over a long period of time without causing any problems. However, hemorrhage can occur unexpectedly at any time. Risk factors:
- Alcohol abuse;
- Smoking;
- Taking drugs;
- Frequent stress;
- Obesity;
- Sedentary lifestyle;
- Increased amount of cholesterol;
- Diabetes;
- Heredity;
- Elderly age.
By eliminating as many risk factors as possible from your life, other than age, you can increase your chances of good health.
A healthy lifestyle reduces the risk of hemorrhage.
Types of hemorrhage
The compilation of classes of the described disease was created in the late 90s, as a result of which the list was included in international medical documents on the classification of diseases. Based on the source in the form of ICD-10, the presented pathological process is divided into several forms:
- Subependymal (SEC).
- SEC with damage to the extreme parts.
- SEC with progression to areas and substance of the brain.
In addition, there are additional differences between IVH, which differ in location:
- Changes in the lateral structures - begins from nearby soft cavities and manifests itself as a gradual filling of the entire volume with further leakage into other areas. In the case of the formation of a surplus, the size of the main organ begins to increase, as a result of which symptoms of a neurological nature progress (if only one object is filled, the specialists’ prognosis is positive, since this process is similar to a parenchymal disorder).
- Location in the third ventricle - the medial zones of parenchymal disorders become the culprit.
- The focus of inflammation in the 4th lobe originates from the dorsal perimeter of the brainstem or cerebellum.
Magnetic resonance imaging (MRI) in St. Petersburg
The following brain tumors can be located inside the ventricles: ependymoma, subependymoma, choroid plexus papilloma, central neurocytoma, meningioma, giant cell tumor.
Most of these tumors are localized in the lateral ventricles. The optimal method for diagnosing intraventricular tumors is MRI of the brain.
Ependymoma accounts for 2-9% of intracranial tumors and 6% of gliomas. Of the ependymal tumors in adults, subependymoma occurs. It makes up about 8% of ependymal tumors and is located near the ventricular wall. The peak incidence of ependymoma itself occurs at the ages of 5 years and 34 years. The tumor originates from ependymocytes. These are usually benign forms. In 60-70% of cases, the tumor is localized infratentorially in the region of the fourth ventricle and in 5-8% in the cerebellar hemispheres. Much less commonly, supratentorial localization of ependymoma is detected: in the hemispheres near the ventricles (on coronal MRI sections it looks like a “cauliflower”), in the region of the third ventricle. Benign ependymomas have an expansive growth pattern. The internal structure is heterogeneous due to cysts (43-83% of cases) and calcification (50% of cases). Contrast enhancement is observed in a third of cases. Anaplastic ependymoma (grade III) metastasizes along the cerebrospinal fluid pathways.
Meningioma is the most common non-glial brain tumor and belongs to the meningeal tumors. In the area of the choroid plexuses of the ventricles they are extremely rare and may be a manifestation of neurofibromatosis type 2. Intraventricular meningiomas occur in 20% of children, while in adults they are 10 times less common. Meningiomas have typical features on MRI , usually homogeneous, with a clear contour, and are well contrasted.
Benign formations of the lateral ventricles include ependymal cysts. They represent the lacing of the lining of the ventricle. On MRI , they have a cerebrospinal fluid signal, are normal, have a clear contour and are not contrasted.
Ventricular choroid plexus tumors overall account for approximately 3% of pediatric brain tumors. In the first year of life their frequency reaches 20%. They are usually localized in the lateral ventricles (80%) and rarely in the IV and III ventricles, as well as the cerebellopontine angle. In adults, on the contrary, they are usually found in the fourth ventricle. Bilateral tumors have been described.
Papillomas are benign tumors. Their frequency is 0.4-0.6% of all brain tumors in all age groups and 1.5-6% of brain tumors in children. In the first 2 months. 40% of papillomas are observed in life. Clinically, the tumor manifests itself in the form of developmental delay, epilepsy and manifestations of mass effect (hydrocephalus, loss of visual fields, etc.). MRI within the ventricle reveals a low signal intensity mass on T2-weighted images and iso- or hypointense on T1-weighted images. On the side of the tumor, the lateral ventricle is sharply dilated, and a high-intensity signal is observed around it, which is associated with transependymal fluid resorption. The formation protrudes from the ventricle, infiltrating its edges, and passes into the paraventricular white matter. Edema around the tumor is pronounced. The internal structure of the tumor may be heterogeneous due to calcification (about a third of cases). Contrast enhancement is good.
Carcinomas, which make up about 20% of choroid plexus tumors, disseminate throughout the ventricular system and subarachnoid spaces, invading brain tissue and bone. On T2-weighted tomograms they are brighter than papillomas and are clearly heterogeneous. MRI reveals a hypointense or isointense mass inside the ventricle on T1-weighted tomograms. On T2-weighted tomograms the tumor has low signal intensity. On the part of the tumor, pronounced hydrocephalus and a high signal around the ventricles themselves are determined due to transependymal fluid resorption. The mass protrudes from the ventricle, infiltrating its edges with transition to the periventricular white matter. Swelling around the tumor is pronounced. The internal structure is often heterogeneous due to calcification (about a quarter of cases). Contrast enhancement is good. Carcinomas are brighter on T2-weighted tomograms and are markedly heterogeneous.
Central neurocytoma accounts for 0.25-0.5% of brain tumors and belongs to neuroglial tumors. Has gradation II. The prognosis is favorable.
A giant cell tumor is also typically located in the 3rd ventricle. Giant cell astrocytoma is one of the characteristic manifestations of tuberous sclerosis, a disease from the group of phakomatoses. In addition, this is a typical site for a colloid cyst of the 3rd ventricle, which is a developmental anomaly and requires differential diagnosis with intraventricular tumors. Unlike a colloid cyst, it has a heterogeneous structure on MRI and CT due to calcifications.
In the 4th ventricle, papillomas of the choroid plexus are rarely found in adults. Epidermoid and dermoid cysts may also be located there. Metastases and hemangioblastomas are initially localized in the brain stem or cerebellar hemispheres, but can spread to the 4th ventricle. Tumors of the 4th ventricle are optimally examined using MRI , since it, unlike, does not produce artifacts. All tumors are well contrasted. In children, tumors of the 4th ventricle are much more common than in adults. These are astrocytomas (usually pilocytic), medulloblastomas and ependymomas. Pediatric stem tumors can also grow towards the 4th ventricle.
Medulloblastoma is a primitive neuroectodermal tumor. It accounts for 15-20% of all brain tumors in children and over a third of tumors of the posterior cranial fossa in this age group. In approximately 75% of cases, medulloblastoma is found in children in the first 10 years of life. The sex ratio is M:F as 2-4:1. The tumor is malignant and grows rapidly in the midline along the cerebellar vermis, obstructing the fourth ventricle and causing occlusive hydrocephalus. Going down, the tumor can pass through the foramen magnum into the cistern magna. Medulloblastoma metastasizes along the cerebrospinal fluid pathways and in 5% of cases hematogenously to the lymph nodes, bones and liver. Clinical manifestations consist of nausea, vomiting, diplopia, and ataxia. MRI usually reveals a homogeneous midline mass in the inferior cerebellum that is hypointense on T1-weighted scans . It is usually hyperintense on T2-weighted MRI The internal structure of the tumor is usually homogeneous. Calcifications, areas of necrosis and cysts are observed in 10-15% of cases. The contrast is good and uniform. Hydrocephalus is present in almost all patients. Leptomeningeal metastases are common.
Cerebellar astrocytoma is usually benign (grade I) of the pilocytic subtype. Peak frequency occurs at ages 5-9 years. The diffuse fibrillary subtype is much less common, usually in adolescents. It is characterized by infiltrative growth and an unfavorable prognosis. The primary source of astrocytoma is the cerebellar vermis. The tumor is located in the midline, but can also grow in the cerebellar hemisphere. Only 10% of tumors are purely solid, the rest have a cystic necrotic center or consist almost entirely of a cyst with tumor tissue inside its wall. Clinical manifestations include weakness, ataxia and tremor.
On MRI , the tumor is hypointense on T1-weighted MRIs and hyperintense on T2-weighted MRIs . It can be very difficult to distinguish a cystic component from a solid one, since the cyst contains a lot of protein. Contrast helps, in which the solid part is enhanced. The node can be round or flat. The walls of the cyst are not contrasted. Unlike a cyst, the walls of the necrotic cavity are contrasted. Occlusive hydrocephalus is often observed.
Ependymoma accounts for 9-16% of CNS tumors in children, with 60-70% of them localized infratentorially. In children, ependymoma most often occurs before the age of 5 years. A rare embryonic variant is ependymoblastoma, a very malignant tumor. The degree of differentiation of ependymomas can be different; a benign subtype is more often observed. Being initially located inside the IV ventricle, it tends to grow into the trunk, move to the spinal cord, or, less commonly, to grow through the foramina of Luschka into the cerebellopontine angle. Clinical manifestations consist of nausea, vomiting, ataxia, diplopia, and loss of cranial nerve function.
On MRI , ependymoma is almost indistinguishable from medulloblastoma or astrocytoma. It is usually inhomogeneous due to microhemorrhages, calcification, small cysts and vessels. CT helps confirm the presence of calcifications (over 40% of cases), which are noticeably less common in medulloblastoma. The cystic component occurs in 20% of cases. In some cases, the “melted wax” symptom helps: the tumor seems to flow along the edges of the fourth ventricle, enveloping the trunk and without causing a noticeable mass effect. In 90% of cases, the tumor is well contrasted.
During MRI in St. Petersburg, we carry out differential diagnosis of tumors of the posterior cranial fossa in children with vascular malformation, abscess, epidermoid and dermoid. These tumors and other formations are better visible in high fields, somewhat worse in low-field open MRIs. Examination of children by MRI in St. Petersburg makes it possible in specialized children's institutions, which is preferable.
Leave feedback.
MRI in St. Petersburg USA
Main factors of appearance and symptoms
There are two stages of bleeding - primary and secondary. PIH is associated with arterial problems in the body or amyloidosis in the cerebral vessels, so they are diagnosed in rare situations. Based on some data, such an anomaly occurs once in 300 patients. The second version of FFM is formed due to the incorrect use of certain medications (for example, antiplatelet substances or fibrinolytic drugs), the presence of a neoplasm capable of breakthrough, or cancerous tumors.
With such an illness, the patient experiences a rapid increase in depression of thinking. Usually, a coma appears after a stroke in the first hours. Only with a gradual progression of the disease and, most importantly, a minimum amount of fluid released, the consciousness of the individual remains stable for a long time and decreases gradually.
Often, bleeding occurs along with:
- meningeal manifestations and gag reflexes.
- Extreme sweating.
- Trembling, similar in nature to chills.
- Change in skin color.
- Abnormal accumulations of blood cells in the vascular ducts, occurring in the face, torso, arms and legs.
- An initial decrease in body temperature, and as a result a rapid jump reaching above 40 degrees.
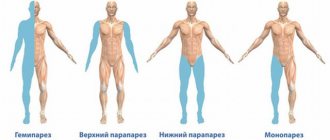
A typical symptom of such a disorder in the body is a decrease in the tone of muscle tissue, which manifests itself in the form of hormetonic syndrome or an irreversible stage of coma. In the first method, an attack of increased muscle activity in the inflamed area begins. This symptom appears due to external conditions. In the second, deformations develop exclusively in the extensor layers. The patient takes a supine position and arches his back, while tilting his head. The upper limbs are clasped and the forearms are facing inward. Also, it may be accompanied by paresis in the opposite extremities from the pathology, the formation of reflexes in the tendons, the presence of anomalies and lack of action in the abdominal region, disruption of the performance of the pelvic region and its organs.
During the disease, which is localized in the third compartment, difficulties arise in breathing and in the functioning of the circulatory system, and hormetonia syndrome has a bilateral effect. With a deviation located in the fourth ventricle, hiccups and problems with swallowing saliva are caused, uncontrolled movements are not observed, and signs of hormetonia are less noticeable. If the described process continues for a long time in a patient, then an increase in the amount of fluid begins, which provokes an increase in VD, swelling and compression of the nerve areas responsible for the life support of the entire body. The supplement favors disorders of the heart and vascular system.
Diagnostic techniques
To establish a correct conclusion, experts will need to conduct an evaluative check of the person’s medical history, that is, find out the presence of blood diseases, previous hemorrhagic strokes, what medications the patient took that contributed to poor clotting, etc. In addition, doctors conduct a standard examination and prescribe additional tests to create a full picture.
You need to understand that if an anomaly is likely to develop, you should urgently go to the nearest medical center to provide professional clinical care. Also, experts do not exclude the possibility that the patient will have to undergo resuscitation measures on the way to the hospital. In the inpatient building, doctors write out directions for the following procedures:
- MRI scan or computed tomogram, depending on the presence of contraindications.
- Donation of blood cells for analysis, during which there will be a report on the number of platelets in the body.
- Coagulogram examination.
- Electrocardiogram.
- Check blood pressure readings.
If doctors do not have the opportunity to perform magnetic resonance or computer diagnostics on a person due to a coma, then echo-encephalography is prescribed. At certain points, it may be necessary to perform a lumbar puncture in order to distinguish hemorrhage, which provokes the entry of fluid into the spinal substance, from an ischemic stroke.
Symptoms and diagnosis
As a rule, strokes occur more often during the daytime, when a person is alert.
At the moment of defeat, the patient experiences a severe headache and suddenly loses consciousness.
Before this, the following symptoms may appear:
- Frequent attacks of headache;
- Dizziness, general weakness, constant feeling of drowsiness;
- Vomiting, after which there is no relief;
- Numbness of parts of the body, all limbs, face;
- Redness of the face and neck;
- Weakness of the limb muscles on one side;
- Impaired vision and image perception;
- Intermittent or rapid pulse.
The attack is evidenced by:
- Sudden loss of consciousness or state of stupor;
- Change in breathing in any direction (more often or less often);
- Convulsions;
- Facial distortion;
- Dilation of the pupils, gaze directed in one direction;
- Inability to turn or tilt your head.
Diagnostics requires the following manipulations:
- Lumbar puncture. Using a thin long needle, the longitudinal canal of the spinal cord is pierced to collect cerebrospinal fluid. The seized fluid is taken for laboratory analysis to detect blood;
- CT or MRI. This is a more accurate diagnostic tool that allows not only to identify the presence of a stroke, but also to determine the exact size, location and extent of damage;
- Angiography. A diagnostic method in which a contrast agent is injected into the vessels, resulting in an accurate picture of the vessels of the head.
Useful video on the topic:
Treatment Options
The first point for medical staff is the prompt provision of first emergency aid and the immediate implementation of basic level treatment - stabilization of the functions of the heart and lungs, as well as monitoring of blood pressure levels and regulation of the constant flow of internal processes of the body.
In addition, doctors prescribe therapy to get rid of symptoms: intravenous injections that have an anticonvulsant effect, as well as help resolve swelling and normalize blood pressure (in addition, a drug can be used to stop vomiting). To fully stop bleeding, a treatment plan is currently being developed by the most qualified scientists. The pathogenic option involves maintaining optimal blood pressure levels and pumping out excess blood through surgery. Such procedures include:
- The use of agents that have a neurotrophic effect and increase metabolism.
- Taking antioxidants (including vitamin E) and substances that block calcium ducts.
The surgical procedure is selected on an individual basis.