Posterior spinocerebellar Flexig – see page 19
Synapse
3. Posterior spinocerebellar Flexig – see page 19
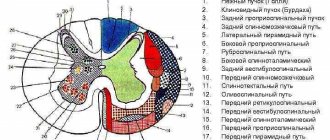
4.Anterior spinocerebellar Goversa - tractus spinocerebellaris anterior, lies ventral to the previous one, as part of the lateral cord. Formed by the axons of the cells of the nucleus of the dorsal horn of the opposite side and the axons of the cells of the intermediate medial nucleus on its side. Ends in the cerebellum. Together with the Flexig path, it provides unconscious coordination of movements.
5. Spinal-tegmental - tractus spinotectalis, adjacent to the medial side and anterior part of the anterior spinocerebellar tract, being part of it. It ends on the nuclei of the tegmentum (quadrigeminal) of the midbrain, providing functions similar to pathways 3 and 4.
6. Spino-thalamic lateral – tractus spinothalamicus lateralis. It lies in the lateral cord, adjacent on the medial side to the anterior spinocerebellar cord, located behind the spinocerebellar tract. Formed by axons of the own nucleus of the dorsal horn of the opposite side. It ends on the lateral nuclei of the thalamus of the diencephalon. Conducts: in the dorsal part of the tract - temperature, and in the ventral - painful irritations.
7. Spinal-thalamic anterior - tractus spinothalamicus anterior s. ventralis, is located in the middle part of the anterior cord in the projection of the posteromedial nucleus of the anterior horn. Formed by axons of the own nucleus of the dorsal horn of the opposite side. It ends on the lateral nuclei of the thalamus. Conducts impulses of tactile sensitivity (touch, touch).
Descending motor pathways of the spinal cord:
They are divided into 2 groups: pyramidal and extrapyramidal. Topographically, they differ in that the pyramidal tracts begin from the cells of the cerebral cortex, and the extrapyramidal tracts begin from the subcortical structures. Functional differences: pyramidal ones provide voluntary contractions of skeletal muscles, and extrapyramidal ones provide involuntary (automatic) contractions.
Lateral corticospinal – see page 19
2. Monakov’s red nucleus-spinal cord - tractus rubrospinalis, passes in the lateral cord, ventral to the previous one. Formed by the axons of the cells of the red nucleus of the midbrain, it provides impulses for the unconscious regulation of movements and muscle tone, ending on the motor neurons of the anterior horns.
3. The olivo-spinal cord of Bechterew-Hellweg - tractus olivospinalis, passes in the lateral cord ventral to the anterior spinal cerebellar tract, located in its lower part along the periphery, near the anterior cord. Formed by the axons of the inferior olives of the medulla oblongata, it ends there. Carries impulses from an intermediate center of balance.
4. Thalamospinal – tractus thalamospinalis. Lies in the lateral funiculus medial to the lateral spinothalamic tract. Formed by axons of cells of the nuclei of the thalamus and hypothalamus of the diencephalon. Provides regulation of unconscious movements and autonomic reactions, ends on the motor neurons of the anterior horns and the lateral sympathetic nucleus of the lateral horns.
5. Reticular-spinal tract – tractus reticulospinalis anterior. Lies in the middle part of the anterior funiculus. Formed by the axons of the cells of the reticular formation of the brain stem of the opposite side. Provides unconscious regulation of movements, ends on the motor neurons of the anterior horns.
6. Held’s vestibulospinal tract – tractus vestibulospinalis. It lies along the periphery of the anterior funiculus on its border with the lateral funiculus. Medially, like the reticulospinal tract, it borders on the anterior corticospinal tract. Formed by axons of the vestibular nuclei of the brain stem, conducting impulses from the vestibular apparatus.
7. The anterior corticospinal cord (pyramidal not crossed) - tractus corticospinalis (pyramidalis) anterior, forms a common pyramidal system with the lateral corticospinal cord. Located in the anterior cord, medial to the reticulo- and vestibulospinal tracts. Formed by the axons of giant pyramidal cells of the cerebral cortex, providing conscious, targeted movements of the neck and torso. It ends on the motor neurons of the anterior horns.
8. Tectospinal tract – tractus tectospinalis. Occupies the most medial position in the anterior funiculus. Formed by axons of cells of the nuclei of the roof (quadrigeminal) of the midbrain. Conducts impulses that provide reflexive protective movements to sudden auditory and light stimuli. This tract is also called the visual-auditory reflex tract.
It is necessary to firmly understand that the anterior cords contain mainly motor pathways, and the posterior cords contain sensory pathways (muscular-articular sense and tactile sensitivity). In the lateral ones there are both sensory and motor pathways.
A significant morphological feature of the conductive tracts of the posterior cords is that they are formed by the axons of sensory neurons of the spinal ganglia, while the other cords contain axons of intercalary neurons from various nuclei and parts of the central nervous system.
Control questions
1. At what level and where does the spinal cord end in the spinal canal?
2.What is the filum terminale and what does it consist of?
3.Name the physiological thickenings of the spinal cord, their location and what they correspond to.
4. How and what is the substance of the spinal cord divided into?
5. How and what is the white matter of the spinal cord divided into?
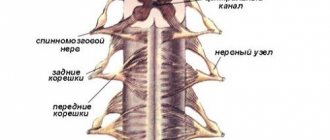
6.What are the anterior roots of the spinal cord formed by?
7.What are the dorsal roots of the spinal cord formed by?
8. What processes and what neurons form the trunk of the spinal nerve?
9.Where is the spinal ganglion located and how is it formed?
10.List the main systems of nerve fibers of the white matter and describe them.
11.What is the spinal cord's own apparatus represented by?
12. Define a segment of the spinal cord.
13.Name the function of the segmental apparatus of the spinal cord.
14.What pathways pass in the posterior funiculi of the spinal cord?
15.List the pathways of the lateral funiculi.
16.List the pathways of the anterior funiculi.
17.What forms the gray matter of a segment of the spinal cord?
18.List the nuclei of the dorsal horn.
19.List the nuclei of the anterior horn.
20. In which segments of the spinal cord are the lateral cords most developed?
21.List the nuclei of the lateral horns.
22.What is the thin Gaulle bundle formed by?
23.What is the wedge-shaped bundle of Burdach formed by?
24.What is the posterior spinocerebellar tract of Flexig formed by?
25.What is the anterior spinocerebellar tract of Gowers formed by?
26.What are the lateral and anterior spinothalamic tracts formed by?
27.What is the posterior intrinsic bundle formed by?
28.What is the anterior intrinsic bundle formed by?
29.What is the lateral intrinsic bundle formed by?
30.Which pathway provides unconscious regulation of movements?
31.Which pathway provides conscious, purposeful movements of the upper and lower extremities?
32.Which pathway provides conscious, purposeful movements of the neck and torso?
33.Which path is called the visual-auditory reflex tract?
Situational tasks
The patient's x-ray revealed the growth of bone tissue in the area of the intervertebral foramina, which led to compression of the spinal nerve cords. What dysfunctions will be revealed during examination of the patient as a result of this pathology?
The patient has a wound of the spinal column in the lumbar region with damage to the posterior horns of the spinal cord. What disorders will be detected in the patient during examination?
The patient developed paralysis (lack of movement) of the left arm. There is also no muscle tone and reflexes in the affected arm. Which part of the central nervous system is damaged?
With age-related changes in the spinal column, compression of the dorsal roots of the spinal cord often occurs. What will be the manifestations of this pathology?
A tumor of the dura mater of the spinal cord led to compression of the posterior cords of the spinal cord. What will be the neurological manifestations of this disease?
The doctor needs to take cerebrospinal fluid for examination. What tissues will the needle penetrate during puncture during the manipulation process?
It is necessary to obtain cerebrospinal fluid for examination. Between which vertebrae should the needle be inserted to obtain it?
In cases of spinal column injury, profuse venous bleeding was noted. Spinal cord function is not impaired. Which interstitial space will venous blood penetrate into?
As a result of a traffic accident, the driver received an injury to the cervical spine with damage to the lateral cord of the spinal cord on the left. What symptoms of the consequences of the injury allowed us to determine the location of the spinal cord injury?
The spinal cord tumor resulted in damage to the anterior white commissure of the spinal cord at the level of the fourth thoracic segment. Based on what signs was the location of the spinal cord lesion determined?
Fig.4. Blood supply to the spinal cord. Diagram of the arteries of the spinal cord.
The main sources of nutrition of the spinal cord are a.spinalis anterior et aaspinales posteriores.
Aaspinales anteriores arise from the vertebral arteries (a.vertebralis dextra et sinistra) in the cranial cavity. At the upper end of the spinal cord they merge into the unpaired a.spinalis anterior (1), running along the fissurae medianae anterioris.
Aaspinales posteriores (2) originate from the vertebral arteries slightly below the anterior arteries. They do not merge and run along the sulci posteriolateralis.
The anterior and posterior spinal arteries anastomose with each other, forming the arterial vascular crown (vasocorona (3)). Branches extend from it, feeding the white matter and most of the posterior horns. The anterior 4/5 of the diameter of the spinal cord receives blood mainly from the a.spinalis anterior system (aasulci (4)).
Rrspinales (5) (depart: in the cervical region from a.vertebralis, in the thoracic region - from a.a.intercostales posteriores, in the lumbar region - from a.a.lumbales, in the sacral region - from a.sacralis lateralis), entering the spinal canal through the corresponding intervertebral foramina, they give radicular branches (a.a.radicularis anteriores (6) et a.a.radicularis posteriores (7)), which anastomose with the anterior and posterior spinal arteries throughout the entire length of the spinal cord.
The veins of the spinal cord drain into the anterior and posterior internal vertebral venous plexuses.
Fig.5. Shells and intershell spaces of the spinal cord.
The spinal cord is covered with three membranes of mesenchymal origin: hard (dura mater, pachimeninx), arachnoid (arachnoidea) and soft (pia mater). The last two together are called leptomeninx.
Dura mater spinalis (1) is formed by dense fibrous connective tissue with a large number of elastic fibers. In the spinal canal, the dura mater is thin and does not adhere to either the surface of the brain or the surface of the spinal canal. On top of the dura mater spinalis there is a dense connective tissue membrane, which adjoins the arches and vertebral bodies and intervertebral cartilage, forming the so-called external sac of the spinal cord. It simultaneously forms the periosteum and, in appropriate places, the perichondrium of the spinal canal. This inner lining is the outer lamina of the dura mater of the spinal cord that separates during development. Arachnoidea spinalis (2) consists of several layers. On the outside, it is represented by a cellular layer consisting of 5-8 layers of densely packed cells - meningocytes. Below is a thin collagen-fibrous layer that forms the basis of the arachnoid membrane and trabeculae connecting it to the pia mater. The inner layer of arachnoidea is represented by flat single-layer epithelium, derived from ependymal glia. The arachnoid membrane is thin, transparent, avascular, durable, and practically impermeable to biological substances.
Pia mater spinalis (3) is represented by a thin endothelial layer of mesodermal cells. It is tightly fixed to the surface of the spinal cord by means of the marginal glycol membrane; rich in blood vessels and nerves.
Ligamentum denticulatum (4) along the entire length of the spinal cord frontally connects the dura and pia mater to each other, fixing the spinal cord. The ligament lies between the anterior and posterior roots and has 20-30 teeth.
Cavum epidurale (5) is the space between the two layers of the dura mater; filled with fatty tissue and internal vertebral venous plexuses (anterior and posterior).
Cavum subdurale (6) is a slit-like space bounded by the dura and arachnoid membranes; contains a small amount of clear liquid, which allows the arachnoid membrane to slide relative to the hard one.
Cavum subarachnoidale (7) is located between the arachnoid and pia mater; performed with cerebrospinal fluid.
The subdural and subarachnoid spaces of the spinal cord are direct continuations of the intracranial interthecal spaces.
Taking into account the specifics of training students of the pediatric faculty, it is necessary to dwell on some issues of the pediatric anatomy of the nervous system.
central nervous system
The nervous system of a newborn is the least developed of all organs and systems. However, the oldest phylogenetic sections: the spinal cord, medulla oblongata, pons, midbrain, and striatum, are more developed than the new sections - the cerebral cortex. Function precedes morphological maturation, and this is especially noticeable at the analyzer level. The organ of balance operates from the time of intrauterine development; the auditory, visual, taste and skin analyzers begin to function immediately after birth. Neuronal differentiation occurs before 3 years of age and is completely completed at 8 years of age. The process of myelination takes place in a certain order: skin receptors, balance organs, olfactory and auditory organs are myelinated in the first two months of life, the last ones are visual receptors. Afferent fibers undergo the process of myelination later than efferent fibers, with the exception of motor fibers belonging to the cranial nerves and the anterior pyramidal tract, which are partially myelinated at birth. The fibers of the lateral pyramidal tract begin to myelinate at the age of 4-6 months, and this process ends simultaneously with the end of the myelination process of the spinal nerves in a child aged 3 to 7 years.
Spinal cord.
In the embryonic period, the spinal cord fills the spinal canal along its entire length, starting from the third month of intrauterine development, the rate of growth of the spine in length accelerates in such a way that the spinal cord, which has a slow growth rate, leaves part of the canal free. In a newborn, the spinal conus is located at the level of the second lumbar vertebra. The cervical and lumbar thickenings are well defined; they appear at the 3rd month of intrauterine development, simultaneously with the development of the limbs. The external structure of the spinal cord does not differ from that of adults. The spinal cord pathways are proportional in size and located as in an adult.
Answers to situational problems
The patient will experience segmental disorders of motor and sensory innervation.
The patient will experience impaired skin sensitivity of the lower torso and lower limbs.
In this case, the patient has lesions in the anterior horns of the lower cervical and upper thoracic segments of the spinal cord on the left.
Damage to the dorsal roots of the spinal cord is accompanied by loss or reduction of all types of sensitivity in accordance with the zones of innervation of the corresponding segments of the spinal cord.
Damage to the conductive pathways of the posterior cords will lead to loss of muscle-articular sensation on the corresponding side.
When obtaining cerebrospinal fluid, the needle sequentially passes through the skin, subcutaneous fat, interspinous ligament, dura mater and arachnoid mater.
The puncture must be done between the Ш and 1Y lumbar vertebrae.
In this case, blood will penetrate into the epidural space.
This injury led to disruption of the lateral pyramidal tracts with the development of diffuse paralysis of half the body on the side of the injury and ascending pathways of pain and temperature sensitivity on the opposite side.
The localization of the lesion was determined on the basis of bilateral symmetrical loss of pain and temperature skin sensitivity, the innervation of which is associated with the function of the 1Y thoracic segment of the spinal cord.
Synapse
Information about the work “General neurology. Morphology of the spinal cord"
Section: Medicine, health Number of characters with spaces: 42999 Number of tables: 0 Number of images: 6
Similar works
Diary of a neurology intern
64821
11
1
... conferences and reviews of patients, presence at pathological-anatomical autopsies (2 times). 13.04.03.-25.04.03. 1. As part of the internship program, I worked at State Inspectorate No. 30 named after. S.P. Botkin as an intern at the neuroinfection department. (43 patients covered) 2. Continued participation in the creation of the scientific work “Vegetative dystonia in young people with initial ...
Infusion of implantation of synthetic macroporous hydrogel and transplantation of olfactory cibulin cells during the process of regeneration of the spinal cord after a traumatic injury in the experiment
56186
0
0
... investigation, its statistical processing, as well as interpretation of morphological material). ABSTRACT Medvedev V.V. – “Infusion of implantation of synthetic macroporous hydrogel and transplantation of olfactory cibulin cells during the process of spinal cord regeneration after traumatic injury in the experiment.” - Manuscript. Dissertation for the development of the scientific level of a candidate of medical sciences in this specialty...
Human brain and memory: molecular aspect
32732
0
0
... will change. The use of devices that make it possible to obtain a “map” of the metabolic activity of various parts of the brain, as well as the use of molecular genetic approaches should deepen our knowledge of the processes occurring in the brain. Chapter 2: “Human Memory” Memory, the ability to reproduce past experiences, is one of the main properties of the nervous system, expressed in ...
Neurology Cheat Sheet
99102
12
0
y (period of residual effects). The acute period is characterized by general cerebral symptoms. The disease begins during the day, acutely, without warning, with the apoplectiform development of a comatose state, characterized by complete loss of consciousness, lack of active movements, loss of response to external stimuli and disorder of vital functions, as well as sensitive and reflex...
Anatomy of the nervous system pathways
Content
Three of them are localized in the ampoules of the semicircular ducts and are called ampullary ridges, another two are located in the uterus and sac and are called spots. Both ampullary ridges and spots are formed by a cluster of special sensory hair cells of an epithelial nature, participating in the lining of the ampullae, spherical and elliptical sacs and associated with sensory nerve endings.
The conductor of the vestibular analyzer is a chain of three neurons. The body of the first neuron is located in the vestibular node, located deep in the internal auditory canal and formed by bipolar neurons.
Both peripheral and central processes of these ganglion cells participate in the formation of the vestibular part (vestibular nerve) of the vestibulocochlear nerve. The peripheral processes form synaptic contact with receptor hair cells, and the central processes in the pontocerebellar angle (behind the middle cerebellar peduncles) “enter” the substance of the pons, are divided into ascending and descending and “approach” the vestibular nuclei (ascending - to the superior nucleus, and descending ones - to the lateral, medial and inferior nuclei). The body of the second neuron is localized in the lateral and medial vestibular nuclei. The axons of the second neurons at the level of the bridge make a “transition” to the opposite side and end in the median nuclei of the thalamus, where the bodies of the third neurons are located. Their axons form a thalamocortical tract, “passing” through the middle of the posterior limb of the internal capsule and ending in the cerebral cortex.
The cortical end of the vestibular analyzer, according to most authors, is located in the cortex of the parietal and (or) temporal lobes. At the same time, versions are expressed in favor of the superior parietal lobule, supramarginal and postcentral gyri, as well as the superior, middle and inferior temporal gyri.
Diseases and lesions of the organ of balance and the vestibular nuclei of the pons lead to imbalance, deviation of the body to the side, dizziness, rhythmic twitching of the eyeballs (nystagmus) and autonomic disorders (nausea, vomiting, constriction of the pupils, decreased pulse, decreased blood pressure and cold extremities, increased sweating, increased intestinal motility). The clinical picture of damage to the cortical end of the vestibular analyzer is complemented by a violation of orientation in space.
2.2. Proprioceptive pathways to the cerebellum
These pathways relate to the pathways of unconscious proprioceptive sensitivity, which may have served as the main factor in the formation of such an ancient center of balance in the evolutionary sense, which is the cerebellum. Within the central nervous system, direct projections from the spinal cord to the cerebellum and those mediated through the reticular formation and the olive nucleus of the medulla oblongata are distinguished.
The most important are the direct projections, called the “anterior and posterior spinocerebellar tracts.” They transmit proprioceptive information from skeletal muscles, bones, joint capsules and ligaments, allowing the cerebellum to assess the state of the musculoskeletal system of the torso, neck and limbs and regulate muscle tone and coordinate movements aimed, in particular, at maintaining balance. The posterior spinocerebellar tract is more differentiated in a functional sense, as it carries information from each individual muscle. The anterior spinocerebellar tract transmits more general information about the state of a particular group of synergistic muscles. The spinocerebellar tracts originate in skeletal muscles, bones, and bone joints with proprioceptors.
Posterior spinocerebellar tract (bundle of Flexig)
The dorsal (posterior thoracic) nucleus, localized at the base of the dorsal horn, is clearly expressed in the spinal segments C7–L2. Within the spinal cord tr. spinocerebellaris posterior, receiving fibers segment by segment, thickens to the level of C7. Both in the lateral funiculus of the spinal cord and in the inferior cerebellar peduncle (Fig. 5), the Flexig bundle occupies a superficial dorsolateral position.
Rice. 5. Posterior spinocerebellar tract: 1 - muscle, 2 - spinal ganglia (I), 3 - dorsal (posterior thoracic) nucleus of the spinal cord (II), 4 - posterior spinocerebellar tract, 5 - inferior cerebellar peduncle, 6 - cortex of the lower part of the vermis (III)
The path ends in the lower part of the worm, in its bark, both on its own and, according to some authors, on the opposite side.
Anterior spinocerebellar tract (Gowers bundle)
The difference between this pathway is the localization of the body of the second neuron in the nucl. intermediomedialis, located in the central intermediate substance of the spinal cord. Most (90%) of the neurons in this nucleus send their axons through the commissure alba to the opposite side (Fig. 6).
Rice. 6. Anterior spinocerebellar tract: 1 - muscle group, 2 - spinal nodes (I), 3 - intermedial nucleus of the spinal cord (II), 4 - white commissure, 5 - anterior spinocerebellar tract, 6 - superior medullary velum, 7 - superior cerebellar peduncle, 8 - cortex of the superior part of the vermis (III)
A smaller part (10%) is sent to the Govers beam of its side. Thus, in every tr. spinocerebellaris anterior there are fibers from its own and the opposite side, and the latter predominate quantitatively.
The Govers' bundle in the spinal cord is located superficially in the ventrolateral part of the lateral funiculus, with fibers from the overlying segments added on the lateral side. In the medulla oblongata tr. spinocerebellaris anterior occupies a place between the olive and the inferior cerebellar peduncle, and then “passes” into the lateral part of the pontine tegmentum. Near the rostral border of the pons, the Gowers bundle “shifts” dorsally and through the superior medullary velum, the fibers that crossed in the spinal cord “return” to their side and through the superior cerebellar peduncle reach their end point in the cortex of the upper part of the vermis. Thus, unconscious proprioceptive sensitivity is transmitted to the cerebellum on the same side of the body.
Common to the described proprioceptive pathways is the localization of the body of the first neuron in the spinal ganglion, the second in the nuclei of the spinal cord, and the third in the cortex of the cerebellar vermis.
2.3. Pathway of conscious proprioceptive sensitivity (“motor” analyzer)
The proprioceptive field (a set of proprioceptors), the path of conscious proprioceptive sensitivity and the area of the cerebral cortex into which the receptive field of the musculoskeletal system is projected were previously united under the name “motor analyzer”. This name is clearly unfortunate, since it contradicts the very idea of I.P. Pavlov, who described the analyzer as an exclusively sensory, sensitive system. Therefore, if we use the term “motor analyzer,” it should be interpreted as an analyzer whose receptor field is located in the structures of the musculoskeletal system, including skeletal muscles. It would be more correct to call this analyzer proprioceptive, but so far this term has not become widespread.
The “motor” (proprioceptive) analyzer evaluates muscle tone, the position of body parts in space, the presence of gravity and vibration.
Receptors are localized in skeletal muscles, bones, and bone joints.
The conductor is a chain of three neurons. The body of the first pseudounipolar neuron is found in all spinal ganglia. Peripheral processes participate in the formation of spinal nerves and their branches that innervate the organs of the musculoskeletal system (Fig. 7).
Rice. 7. “Motor” (proprioceptive) analyzer: 1 - muscles of the neck, upper torso and upper limbs, 2 - muscles of the lower torso and lower extremities, 3 - spinal nodes (I), 4 - thin fasciculus of Gaulle, 5 - wedge-shaped fasciculus Burdakha, 6 - thin nucleus (II), 7 - cuneate nucleus (II), 8 - internal arcuate fibers, 9 - medial lemniscus, 10 - ventrolateral nuclei of the thalamus (III), 11 - thalamocortical pathway, 12 - precentral gyrus, postcentral gyrus , superior parietal lobule (IV)
VK
Buffer