Why can coma occur after a TBI?
With TBI affecting the central nervous system, the response to external stimuli is lost, which leads to a disturbance in the psycho-emotional state. Suppression of large areas of the brain deprives the victim of reflex function, putting him in a comatose state. After an injury, a person stops feeling pain, does not react to loud sounds, and his pupils lose sensitivity to bright light.
Depending on the duration of loss of consciousness, there are:
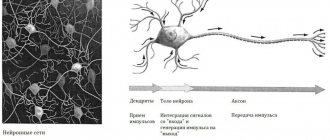
- Severe traumatic brain injury. It is accompanied by intracranial pressure, which disrupts the functionality of the brain and interferes with the work of nerve impulses. The injury is accompanied by a long coma.
- Moderate injury. Loss of consciousness lasts from 2 hours to 2 days.
- Minor injuries. With bruises, consciousness is impaired for a few seconds or remains normal.
Symptoms of coma during stroke
Hemorrhagic stroke is characterized by a predominance of cerebral symptoms in the initial period of the disease. Next, focal neurological symptoms rapidly develop, often leading within a few minutes to a state of coma. This is especially common with hemorrhage in the cerebellum and brain stem. The following symptoms are characteristic of a hemorrhagic stroke of the subarachnoid hemorrhage type:
- relatively young age of the patient;
- sudden onset of the disease during vigorous physical activity;
- severe headache with loss of consciousness;
- emotional arousal;
- rise in blood pressure, and subsequently body temperature;
- often absence of focal neurological symptoms.
In 100% of cases, blood is found in the cerebrospinal fluid of patients.
Coma after a stroke is characterized by the following symptoms:
- lack of consciousness;
- spontaneous urination and defecation.
- lack of response to external stimuli - light, touch, sounds, pain.
In a coma as a result of a hemorrhagic stroke, the patient suddenly loses consciousness, the face becomes cyanotic, breathing is noisy, the pupils are of different sizes, and they react sluggishly to light. In the case of coma that develops in the presence of an ischemic stroke, loss of consciousness, a sharp decrease in blood pressure, slowing of the pulse, and cardiac arrhythmias are observed. The patient is pale, covered in cold, sticky sweat, and has shallow breathing.
Doctors distinguish 4 degrees of coma after a stroke:
- Grade I is characterized by minor brain damage. The patient experiences lethargy or complete loss of consciousness. Reflex functions are preserved. The prognosis is encouraging;
- II degree: noisy intermittent breathing, deep sleep in the absence of the slightest reaction to pain, loss of skin reflexes, convulsions;
- III degree: loss of consciousness, drop in blood pressure and decrease in body temperature;
- IY degree is considered incompatible with life due to the death of a significant part of the brain.
Types of coma and their symptoms
Coma that occurs due to traumatic brain injury is divided into 3 types, differing in the severity of symptoms:
- deep;
- actual coma;
- superficial.
Superficial coma
After a traumatic brain injury, the victim remains in a state of deep sleep. The person reacts to others by opening his eyes, slightly moving his limbs, and is able to carry on conversations with sluggish speech.
Interesting: Symptoms, treatment features and consequences of TBI in a child
Actually coma
If with a superficial loss of consciousness the patient reacts to external stimuli, then in the case of an ordinary coma the reaction is spontaneous. The sudden opening of the eyes, the utterance of sounds and the contraction of limbs are not controlled by the patient, so for his safety, doctors can limit the mobility of the body using restraints.
Deep coma and vegetative state
Traumatic brain injury is accompanied by impaired reflex function. The victim, who is in a deep coma, requires a device to maintain respiratory function. The person does not respond to light and pain.
Impaired consciousness: mechanism of occurrence
After damage to the central nervous system due to a traumatic brain injury, a person loses the ability to respond to any external stimulus. The psycho-emotional state is completely disrupted, the victim cannot contact the people around him. Coma sets in.
Coma due to TBI is characterized by the immersion of a person in a specific state, which is associated with inhibition of certain areas of the central nervous system. The victim does not respond to pain, bright light and loud sound, and has no reflexes.
Consciousness is impaired when certain parts of the brain that are responsible for speech, thinking, wakefulness, and reasoning are damaged. Based on the degree of damage, loss of consciousness can have different durations:
- mild traumatic brain injury (for example, bruise): loss of consciousness does not occur or lasts no more than 5 seconds;
- moderate injury (for example, open head injury): duration of disturbance of consciousness – 2 hours-2 days;
- severe injury: deep coma and vegetative states occur.
Coma after TBI is not a separate disease, but only a consequence of damage to the central nervous system. If there is a severe general condition that threatens a person’s life, he may be placed in an artificial coma. This condition allows you to cause a controlled decrease in the activity of reflexes and vital functions.
An artificial coma involves the introduction of special medications into the body. In this case, the respiratory function is performed by a ventilator.
Determination of the depth of coma
The depth of coma is determined using the Glasgow scale, consisting of 3 tests for:
- motor activity, assessed from 1 to 6 points;
- speech reaction, rated from 1 to 5 points;
- eye opening reaction, graded from 1 to 4 points.
With a maximum number of points (15), consciousness is clear, and with a minimum score (3), brain death is registered.
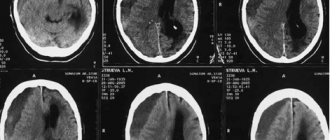
In addition to the Glasgow scale, the following are used in the diagnosis of TBI:
- CT and MRI scans that determine the location of tumors or hematomas compressing parts of the brain that control the heart rhythm and respiratory system.
- An EEG, which records the electrical activity of brain cells and the degree of damage to the functions of the central nervous system.
- Lumbar puncture for TBI. Analysis of the cerebrospinal fluid allows you to understand the cause of the coma.
- X-ray to track injuries to the spine and skull.
Treatment during coma
The main task in the treatment of TBI is to preserve the function of the cerebral vessels responsible for blood circulation.
Normalization of breathing and support of the circulatory system after a traumatic brain injury is carried out using a ventilator and drugs that normalize heart rhythm, circulating blood volumes and blood pressure levels.
Further therapy for traumatic brain injury depends on the condition of the brain, prescribed after a thorough diagnosis and including:
- Drug treatment of TBI. The drugs used prevent genitourinary infections and thrombosis, eliminate symptoms caused by injury, and support kidney and liver function. To eliminate the causes of the coma, surgery is performed, but if possible, adhere to medication.
- Physiotherapy. Exercise therapy is aimed at maintaining muscle tone and joint flexibility. Equally important is the prevention of bedsores formed under the pressure of a stationary body.
Interesting: Classification, symptoms, treatment and consequences of TBI
Characteristic symptoms
Coma after traumatic brain injury is primarily characterized by impaired consciousness. All symptoms of this condition can be divided according to the degree of its severity:
- Superficial disturbance of consciousness. The person falls into deep sleep. When trying to talk to the victim, he may open his eyes and sometimes start a conversation. Speech with punctuation. The patient can make slight movements of the limbs.
- Ordinary coma. The patient is able to make sounds, unintentionally open his eyes and make sudden movements with his hands. The doctor can fix the victim’s limbs with special devices to prevent physical harm.
- Deep coma. Reflexes, mobility and respiratory function are completely absent. There is no reaction to pain, just like there is to the light of the pupils.
How does one recover from a coma?
Regardless of the severity of the traumatic brain injury, the patient is required to undergo a mandatory course of rehabilitation measures.
The primary task when recovering from a coma is to restore brain function.
Memory and attention deteriorate in all victims, and in some cases amnesia of varying duration develops. Confused consciousness and loss of spatial orientation make independent movements difficult. During the rehabilitation period, the patient is helped not only to move, but also to maintain a sitting position.
The procedure for further rehabilitation is individual and lasts from several months to several years.
Consequences of TBI after recovery from coma
Coma is one of the most severe consequences that occurs after a traumatic brain injury.
Let's consider the types of comatose state after TBI and how to determine its depth, and also talk about treatment methods and rehabilitation measures used after the return of a conscious state.
Why can coma occur after a TBI?
With TBI affecting the central nervous system, the response to external stimuli is lost, which leads to a disturbance in the psycho-emotional state. Suppression of large areas of the brain deprives the victim of reflex function, putting him in a comatose state. After an injury, a person stops feeling pain, does not react to loud sounds, and his pupils lose sensitivity to bright light.
Depending on the duration of loss of consciousness, there are:
- Severe traumatic brain injury. It is accompanied by intracranial pressure, which disrupts the functionality of the brain and interferes with the work of nerve impulses. The injury is accompanied by a long coma.
- Moderate injury. Loss of consciousness lasts from 2 hours to 2 days.
- Minor injuries. With bruises, consciousness is impaired for a few seconds or remains normal.
Types of coma and their symptoms
Coma that occurs due to traumatic brain injury is divided into 3 types, differing in the severity of symptoms:
- deep;
- actual coma;
- superficial.
Superficial coma
After a traumatic brain injury, the victim remains in a state of deep sleep. The person reacts to others by opening his eyes, slightly moving his limbs, and is able to carry on conversations with sluggish speech.
Interesting: Providing first aid for TBI
Actually coma
If with a superficial loss of consciousness the patient reacts to external stimuli, then in the case of an ordinary coma the reaction is spontaneous. The sudden opening of the eyes, the utterance of sounds and the contraction of limbs are not controlled by the patient, so for his safety, doctors can limit the mobility of the body using restraints.
Deep coma and vegetative state
Traumatic brain injury is accompanied by impaired reflex function. The victim, who is in a deep coma, requires a device to maintain respiratory function. The person does not respond to light and pain.
Determination of the depth of coma
The depth of coma is determined using the Glasgow scale, consisting of 3 tests for:
- motor activity, assessed from 1 to 6 points;
- speech reaction, rated from 1 to 5 points;
- eye opening reaction, graded from 1 to 4 points.
In addition to the Glasgow scale, the following are used in the diagnosis of TBI:
- CT and MRI scans that determine the location of tumors or hematomas compressing parts of the brain that control the heart rhythm and respiratory system.
- An EEG, which records the electrical activity of brain cells and the degree of damage to the functions of the central nervous system.
- Lumbar puncture for TBI. Analysis of the cerebrospinal fluid allows you to understand the cause of the coma.
- X-ray to track injuries to the spine and skull.
Treatment during coma
The goal in the treatment of TBI is to preserve the function of the cerebral vessels responsible for blood circulation.
Normalization of breathing and support of the circulatory system after a traumatic brain injury is carried out using a ventilator and drugs that normalize heart rhythm, circulating blood volumes and blood pressure levels.
Further therapy for traumatic brain injury depends on the condition of the brain, prescribed after a thorough diagnosis and including:
- Drug treatment of TBI. The drugs used prevent genitourinary infections and thrombosis, eliminate symptoms caused by injury, and support kidney and liver function. To eliminate the causes of the coma, surgery is performed, but if possible, adhere to medication.
- Physiotherapy. Exercise therapy is aimed at maintaining muscle tone and joint flexibility. Equally important is the prevention of bedsores formed under the pressure of a stationary body.
Interesting: Tablets for concussions in adults
How does one recover from a coma?
Regardless of the severity of the traumatic brain injury, the patient is required to undergo a mandatory course of rehabilitation measures.
The primary task when recovering from a coma is to restore brain function.
Memory and attention deteriorate in all victims, and in some cases amnesia of varying duration develops. Confused consciousness and loss of spatial orientation make independent movements difficult. During the rehabilitation period, the patient is helped not only to move, but also to maintain a sitting position.
The procedure for further rehabilitation is individual and lasts from several months to several years.
Rehabilitation after traumatic brain injury
During the initial period of rehabilitation, a patient with a TBI is helped with self-care, restoring memories of lost skills.
The rehabilitation course is carried out under the guidance of:
- a psychologist who normalizes the psyche and allows you to re-enter society;
- a neurologist and physiotherapist responsible for carrying out massage procedures and exercise therapy that restore muscle tone;
- a neurospeech therapist who helps restore speech function;
- occupational therapist developing memory, speech and motor skills.
During rehabilitation after TBI, it is important to maintain consistency and frequency. The first improvements are an indicator of treatment effectiveness, but not effectiveness. Cancellation of restorative measures occurs only after agreement with the attending physician.
Complications
The main complications of traumatic brain injury include:
- partial or complete paralysis of the limbs;
- chronic cephalgia;
- breathing, hearing, speech and vision disorders;
- development of epilepsy;
- problems with memory, including complete amnesia, and concentration.
Long-term forecasts
Depending on the degree of damage to the central nervous system, the patient after TBI is diagnosed with the level of depression of consciousness:
- Stupor. Superficial coma, accompanied by a reaction to external stimuli, is treatable. With timely assistance, the victim comes out of a coma with minimal deviations.
- Sopor. Movements are carried out at the level of reflexes, and there is a violation of brain impulses. A rapid deterioration of symptoms is dangerous due to the transition to stage 3 damage to the central nervous system, but timely treatment and high-quality rehabilitation leave a high chance of a full life.
- Severe degree of central nervous system depression. The patient is in a vegetative state and needs hardware assistance. Disability cannot be avoided even with successful treatment.
- Death. Irreversible disorders in the central nervous system lead to extensive hemorrhages or hemorrhagic stroke.
The prognosis worsens when the coma is protracted, lasting for several years.
If the coma lasted several weeks or months, and after the return of consciousness there is a gradual restoration of lost functions, then the prognosis is favorable. Such patients are able to return to their normal lives without complications.
To normalize the patient’s condition, it is important to follow the actions recommended by the doctor throughout the entire period, even if its duration is more than a year.
( 1 rating, average 5 out of 5 )
Rehabilitation after traumatic brain injury
During the initial period of rehabilitation, a patient with a TBI is helped with self-care, restoring memories of lost skills.
The rehabilitation course is carried out under the guidance of:
- a psychologist who normalizes the psyche and allows you to re-enter society;
- a neurologist and physiotherapist responsible for carrying out massage procedures and exercise therapy that restore muscle tone;
- a neurospeech therapist who helps restore speech function;
- occupational therapist developing memory, speech and motor skills.
During rehabilitation after TBI, it is important to maintain consistency and frequency. The first improvements are an indicator of treatment effectiveness, but not effectiveness. Cancellation of restorative measures occurs only after agreement with the attending physician.
Complications
The main complications of traumatic brain injury include:
- partial or complete paralysis of the limbs;
- chronic cephalgia;
- breathing, hearing, speech and vision disorders;
- development of epilepsy;
- problems with memory, including complete amnesia, and concentration.
In some cases, the consequences of TBI are reversible. If a person loses the ability to self-care after emerging from a coma, then he has a chance of recovery during the rehabilitation period. Interesting: Providing first aid for TBI
Traumatic brain injury: coma after head injury – Izvilina
Head injuries themselves pose a health hazard to the victim and can lead to serious complications. In case of serious damage to the structure of the brain substance, the patient may fall into a coma.
With it, the patient loses consciousness, does not respond to stimuli and is literally between life and death. Coma after a traumatic brain injury can manifest itself differently depending on the degree of damage to the cerebral tissue.
The lack of timely professional assistance threatens the death of the victim or the development of severe disability.
After a TBI, the victim may go into a coma.
The mechanism of coma during TBI
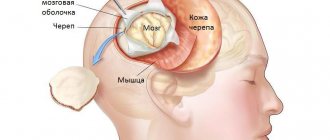
The development of coma affects the general condition of the patient, but the central nervous system is primarily affected.
A disorder of its functions leads to changes in consciousness, dulling of reflexes, lack of response to external factors and the ability to contact others.
The pathological phenomenon in its quality resembles very deep sleep, which is caused by inhibition of the work of certain parts of the brain.
Coma due to TBI is not an independent disease, but a consequence of a malfunction of the nervous system.
It is important to understand the mechanism of its development in order to properly treat and eliminate risks to the victim’s life.
Coma occurs as a result of extensive damage to the brain matter, as well as vital centers of the central nervous system.
This causes damage to the transmission pathways of nerve impulses to all organs and systems, disruption of processes that are the key to the normal functioning of the body.
Such consequences result from changes in tissue structure and circulatory disorders in certain areas. The loss of communication between the higher parts of the nervous system and functional centers is aggravated by local or general cerebral edema.
In coma, the transmission of nerve impulses to organs is disrupted.
Types and symptoms of coma
Regardless of the cause of coma and its form, the main symptom of the pathological condition is impaired consciousness. Dysfunction of individual areas of the brain can manifest itself in different ways.
Often, the clinical picture of the disorder helps doctors make a preliminary diagnosis and select the best first aid options.
Symptoms that may accompany coma with different types of traumatic brain injury:
- speech disorders;
- inability to perform purposeful actions with the upper and/or lower extremities;
- sudden cramps, involuntary muscle contractions;
- rapid rhythmic movements in the knee and/or ankle joints;
- varying degrees of decrease in consciousness up to its complete shutdown and absence of reflexes;
- paralysis;
- breathing problems;
- fixation of pupils;
- heart rhythm disturbance.
In coma, the heart rhythm is disrupted.
The degree of brain damage is determined using a special Glasgow scale. To use it, you need to evaluate a number of indicators, calculate the points obtained and check which diagnosis their number corresponds to.
Determination of the level of coma
Restoration of impaired or lost functions of the central nervous system is possible only after establishing the cause of the coma and its type. The first assessment of the victim’s condition is carried out before emergency care is provided.
Restoration of the central nervous system is possible only after establishing the type of coma.
Diagnosis of a patient with TBI in a coma includes:
- collecting anamnesis - interviewing the victim’s relatives, witnesses of the accident, collecting data from the patient’s medical record;
- physical examination - examination of the skin and mucous membranes, assessment of the functioning of the respiratory and circulatory system, checking the fundus of the eye and the reaction of the pupil to light. Additionally, the likelihood of spinal injuries is determined, and certain types of palpation and percussion of the body are used. They are necessary to exclude pathological enlargement of organs and the presence of internal bleeding;
- neurological tests - include checking the level of unconsciousness, eye reaction, establishing the degree of motor activity and tendon reflexivity. Muscle tone is assessed, asymmetry of the facial areas is excluded;
- laboratory and hardware tests - X-ray of the skull, MRI, CT, EEG, angiography, lumbar puncture, measurement of intracranial pressure.
If necessary, the attending physician may prescribe additional diagnostic tests. The manipulations are repeated regularly to monitor the dynamics of the patient’s condition.
To diagnose the patient, a lumbar puncture is performed.
How does one come out of a coma?
Depending on how the brain tissue responds to the treatment, the victim's return to consciousness may manifest itself in different ways. Regardless of the specifics of the case, recovery from a coma after a TBI requires increased attention and a number of rehabilitation measures.
Doctors must take measures to restore the functionality of damaged tissues. After restoration of consciousness, the patient may experience amnesia, decreased quality of attention, and memory impairment. This is accompanied by loss of the ability to sit and walk without assistance for any period of time.
The picture is often complemented by confusion and loss of orientation in space.
Rehabilitation period
Depending on the individual and general reactions of the body, the recovery period takes place under the supervision of a neurologist, physiotherapist, or psychologist.
Sometimes a speech therapist, occupational therapist, or physical therapy doctor is involved in the work. The main thing is to avoid significant mental or physical stress in the first days of emerging from a coma.
Rehabilitation after a coma due to TBI can take several months or even years.
The main thing during rehabilitation after a coma is not to overload the brain.
Brain coma and its consequences
Coma, from ancient Greek, means deep sleep, drowsiness. It is characterized by a lack of consciousness, motor activity and reflexes, inhibition of the vital processes of breathing and heartbeat. A patient in a coma is deprived of an adequate response to external stimuli, for example, touch or voice, or pain.
Why does consciousness disorder occur?
The normal functioning of the central nervous system (CNS) is ensured by balancing excitation and inhibition. In the case of an unconscious state, the inhibitory influence of individual brain structures on the cortex predominates. Coma always occurs as a result of extensive damage to brain tissue.
Causes
The causes of unconsciousness are quite varied. Brain coma can occur when:
- infections of the nervous system, meningitis of a viral and bacterial nature;
- injuries to the head and brain matter;
- ischemic strokes or as a result of cerebral hemorrhage;
- toxic damage to the nervous system caused by overdose of drugs, alcohol, as well as exposure to drugs and toxic substances;
- tumors of the central nervous system;
- impaired metabolism (diabetic comas with high or low blood sugar levels, adrenal dysfunction with hormonal imbalance, accumulation of waste metabolic products with depressed liver and kidney function).
Symptoms
When coma develops, disturbances of consciousness always come to the fore.
There are three main types of coma depending on the severity of the patient:
- superficial;
- actual coma;
- deep.
In the superficial form, the patient resembles a deeply sleeping person. Verbal appeal to him is accompanied by opening of the eyes, sometimes the ability to answer questions. Speech disorders manifest themselves in sluggish and incoherent speech. Minimal movements in the limbs are maintained.
While in a state of normal coma, a person may make sounds, suddenly open his eyes and become agitated. Doctors sometimes even have to restrain such patients with special means so that they do not cause physical harm to themselves.
Deep coma is characterized by a complete absence of movements and reflexes. In this state, the patient does not swallow saliva and does not breathe. There is a complete absence of reaction to pain, and the pupils react poorly to light.