Cavernous angioma is a benign neoplasm in the brain, which consists of pathologically developed blood vessels, which determines the nature of the course of the disease. In most cases, it is a congenital defect of the blood flow system. Unlike vascular malformations (improper connection of arteries and veins) of another type, the pathology is usually asymptomatic. Cavernous angioma is often discovered incidentally during an MRI or CT scan ordered for another reason.
What is this
It has already been said that cavernous angioma of the brain is a vascular neoplasm that is benign in nature. The pathology includes lymphatic or blood vessels. In children, pathology is more often diagnosed, because during fetal development their capillaries, veins and arteries can become intertwined.
The size of neoplasms can average from a millimeter to several centimeters or more. Large areas are rarely affected. The pathology consists of cavities, their surface is strewn with endothelial cells, and there is plasma inside. Often the pathology does not have clear symptoms, which makes it difficult to identify.
If a person notices signs of a brain cavernoma, then it is important to see a doctor immediately. Only a specialist will be able to make a diagnosis and decide what treatment to prescribe in a particular case. Inaction or improper therapy can lead to complications.
How is angioma treated?
It is very difficult to make a forecast about the danger of venous angioma for a person - it all depends on its location, size and tendency to grow.
With cavernous hemangiomas of small sizes, there is no need to undertake any manipulations at all - people can easily live with them into old age. In other cases, the treatment of cerebral angioma is only surgical. If the angioma is located under the bones of the skull, it is destroyed with a gamma knife. During the intervention, the flow of rays blocks the blood supply in the pathologically altered vessels and, as it were, glues them together.
When the tumor is localized in deeper structures - in the left or right temporal lobe, at the base of the brain - sclerotherapy is used.
This method involves the introduction into the cavernous plexuses of the tumor and cavities of a special chemical compound that has a pronounced irritating effect on the endothelium, which causes collapse of the vascular lumen and scarring.
After such manipulation, the brain angioma becomes empty - no blood flows into it and does not cause compression of the brain tissue.
Treatment of brain angiomas with tablets and droppers is impossible - not a single drug can reduce the size of a vascular tumor. It is possible to use drugs as a means of prevention, but their prescription does not change the fact that you will need to be regularly examined so as not to miss the moment if the tumor begins to grow.
Main features
The main danger of cavernous angioma is that only 40% of patients have significant symptoms. If signs appear, they can be confused with many other neurological diseases. Only with an examination will it be possible to clearly say what exactly a person is suffering from. For this reason, you should not postpone a visit to the doctor if changes in your health have been noticed.
A brain cavernoma has the following symptoms:
- A person is often bothered by headaches, which gradually increase and are not treated with medications.
- Seizures of epilepsy may occur, during which the muscles contract convulsively.
- There is ringing and noise in the ears.
- The patient suffers from an inability to concentrate and has memory problems.
- There is numbness in the limbs, and complete paralysis may even occur.
- Speech impairment may be observed; the patient is unable to pronounce some letters, or is unable to construct entire sentences.
- The gait changes because the person suffers from poor coordination.
Cavernous angioma is most often discovered during a routine examination, or when another pathology is suspected. If a person does not go to doctors and does not experience negative symptoms, he may not know about the presence of a problem for the rest of his life . Given the fact that the disease is considered unpredictable, it is impossible to say for sure whether a person will live long or will have complications.
Symptoms
Cavernomas formed in the brain are rarely accompanied by neurological symptoms. Neurological deficit (hemiparesis, impaired consciousness) usually occurs as a consequence of hemorrhages. The patient can live with a diagnosed benign tumor for a long time without experiencing discomfort. Signs of pathology:
- Epileptic and convulsive seizures.
- Focal hemorrhages in the subarachnoid space or in the cranial cavity, often recurrent.
- Occlusive hydrocephalus, which is characterized by impaired outflow of cerebrospinal fluid.
- Cerebral hypertension due to the accumulation of cerebrospinal fluid.
Due to the nonspecificity of the symptoms, difficulties arise in making the diagnosis of cavernous angioma. Focal tissue lesions that are observed on MRI or CT images are often mistakenly regarded as intracerebral tumors (gliomas). If the tumor is localized in the deep tissues of the brain, it is considered inoperable.
Reasons for appearance
The origin of cavernous angioma is most often congenital, so the pathology appears even inside the mother’s womb. Experts suspect that a gene mutation that occurs during pregnancy plays a major role. Otherwise, it is quite difficult to say exactly what exactly provokes the appearance of the disease. The fact is that the brain has not yet been studied enough. In particular, experts cannot say unambiguously what leads to a brain cavernoma.
It is noted that the presence of an oncological process increases the risk of pathology . A serious condition such as cirrhosis of the liver also contributes to the development of the disease. Even a healthy person is recommended to be examined in order to exclude the possibility of developing the disease. As already mentioned, symptoms do not appear in all cases, so it is extremely important to get examined not only when negative signs appear.
Causes and mechanism of development
Causes of development of cerebral hemangioma:
- Hereditary factors. There is a high probability of developing a tumor if the parents suffered from the same pathology.
- Environment: exhaust fumes, junk food, smoking and alcohol. These are not direct factors, but indirect ones - they provoke cell mutation.
- Traumatic brain injuries: bruises, fractures of the skull, concussion, compression of the brain, hemorrhages in the skull or brain.
- Neuroinfections: encephalitis, meningitis, myelitis, polio, rabies, neurosyphilis, cerebral malaria, leptospirosis.
- Purulent brain damage due to neuroinfection.
- Heart failure, cirrhosis and liver failure.
- Involutional changes in the body (aging).
- Already existing tumors.
- Many years of work in the chemical industry: working with vinyl chloride.
- Long stay in areas of increased radiation activity.
Angioma, before becoming a tumor, goes through several stages of development:
- Initiation. As a result of spontaneous mutation (the gene that controls the number of divisions “breaks”), some cells acquire the ability to reproduce endlessly. At this stage, tumor development depends on the body's immune system, age, hormones and hereditary factors.
- Formation of an angioma node. Development at the second stage depends on the action of secondary factors: smoking, alcohol, environmental pollution, stress - factors that do not directly affect the tumor.
- Progression of pathological tissues. Cells finally acquire the ability to endlessly divide, their growth goes beyond the control of the regulatory systems of the genetic apparatus. The body can no longer cope with a large number of newly formed cells, so many of them survive and form a tumor nucleus.
Varieties
Cavernous angiomas come in different types; they are classified depending on which area is affected by the pathology. This will determine the symptoms that the patient may experience. Determining the exact type is important because location affects subsequent treatment. Types of cavernous angiomas:
- Frontal lobe . It accounts for about 25% of cases of cavernous neoplasms. May cause mental disorders. The patient suffers from memory loss as well as involuntary movements of the limbs.
- Left frontal lobe . In this case, you can observe problems with speech, as well as with short-term memory. As the disease progresses, the person becomes apathetic and detached.
- Right frontal lobe . The main symptom is excessive speech activity. A person sometimes becomes too emotional, and often behaves inappropriately.
- Right temporal lobe . When this area is affected, disorientation occurs. A person may not recognize familiar sounds and voices of familiar people.
- Left temporal lobe . The person’s hearing becomes worse, memory lapses are observed, and the patient may repeat already spoken sentences several times.
- Parietal lobe . Intellectual function disorders occur, due to which a person loses the ability to build logical connections, as well as perform mathematical calculations.
- Cerebellar cavernomas . The patient experiences unexpected and uncontrolled movements of the limbs. A person cannot sit correctly and move independently in space. There may be seizures, as well as problems with speech.
When diagnosing cavernous angioma, the presence of a hereditary factor is often taken into account. If at least one of the parents had this disease, then there is a 50% chance that the children will also have a neoplasm. People who are at risk are recommended to be regularly monitored by doctors.
Diagnostics
Cavernous angioma cannot be detected without certain examinations. It is important for doctors to make sure that there is a tumor on the left, right frontal lobe, or in other places. It is also necessary to determine how quickly cavernous angioma develops, because the likelihood of complications depends on this. Research is carried out using the following procedures.
MRI. This is one of the most effective diagnostic methods, thanks to which it is possible to identify the cavernous angioma of the brain. This procedure will allow you to accurately determine whether a person has a pathology, as well as what size it is. If there is bleeding, then that too will be detected.
CT scan. With its help, it is possible to identify the occurrence of neoplasms, but making an unambiguous diagnosis will be difficult. This method is well suited for detecting bleeding of cavernous angioma.
Tractography . It is needed in situations where the pathology is deep, and it is necessary to plan the operation, as well as determine the dosage of the radioactive substance during the stereotactic method of therapy.
General tests such as blood and urine tests may also be needed. They are able to tell about the condition of the body, as well as the presence of other abnormalities. If a brain cavernoma is detected, then proper treatment will need to be started.
Drug therapy
When tumors do not show signs of growth, the attending physician may prescribe complex drug therapy rather than surgery. In this case, the following types of medications are used:
- Corticosteroids – Medrol, Prednisolone, Dexamethasone.
- Non-cardioselective beta-blockers or Timolol and drugs based on it - Anaprilin, Timadern.
- Cytostatics are antitumor drugs that interfere with the growth and development of angiomas.
To obtain a positive result from treatment, the doctor prescribes sclerotherapy. A medicine is injected into the tumor clot to reduce the growth. If there is no positive result from drug therapy, they resort to surgical intervention.
Methods of treating pathology
Benign neoplasms do not require surgical intervention in all cases. A brain cavernoma can remain with a person for the rest of his life if it does not bother the patient. However, there is a risk of complications, for this reason the doctor may decide to remove the pathology.
Treatment options:
- Steroid drugs . They can be prescribed in tablet form or injected directly into the cavernous angioma. The advantage of these drugs is that they help slow the growth of pathology.
- Sclerotherapy . Its essence is that special agents are injected into the tumor area, which reduce blood flow to the problem area. Due to this, the brain cavernoma decreases in size.
- Surgical intervention . If a cavernous angioma of the left temporal lobe or another location rapidly grows and expands, then surgery may be required. Much will depend on where exactly the pathology is located. Surgical removal of cavernous angioma is not possible in all cases.
Only a specialist, after diagnosis, can decide which treatment option is suitable for a particular patient. Hemangioma, although not malignant, can lead to negative consequences. There is no point in self-medicating, because it is not effective.
Cavernous angioma of the brain
Cavernous angiomas (cavernomas) are most often congenital vascular anomalies, represented by single, much less often multiple cavities, separated inside by septa (septa) and filled with blood. The blood supply to the cavity is carried out from small arterioles and capillaries, and the outflow of blood through venules is of the same order. Due to the small caliber of the feeding vessels, the blood pressure in cavernomas is low, so the draining veins do not hypertrophy and are not visible during SCT/MRI/Angiography. A special feature of cavernomas is a very thin, defective vascular wall, so thin that the cellular elements of the blood - red blood cells - “sweat” through it and settle in the adjacent medulla. This process is called “diapedetic hemorrhage.” The products of the natural breakdown of hemoglobin (hemosiderin), contained in red blood cells, form a zone of chronic, specific and very recognizable changes on MRI around the cavernoma.
Cavernomas can be localized in any part of the brain, mainly in the cerebral hemispheres, as well as in the brain stem, cerebellum, subcortical ganglia, corpus callosum and lateral ventricles. In approximately 30-40% of cases, cavernous angiomas are combined with another type of vascular malformation - venous angiomas. Venous angiomas are an anomaly in the development of venous vessels in the form of a “bundle” of small veins (“Gorgon’s head”) gathering into one large drainage vein.
The incidence of cavernous angiomas is several cases per million population.
What is the danger of having a cavernous angioma?
Cavernomas can remain asymptomatic throughout life. However, in a number of patients, clinical manifestations can be of two types, both individually and in combination:
- Hemorrhage. Sometimes, an increase in blood pressure inside a cavernoma leads to local destruction of the vascular wall and the formation of intracerebral hemorrhage. Unlike AVMs, hemorrhages from cavernomas are never massive and do not pose a threat to the patient’s life, with the exception of extremely rare cases of cavernomas located in the lower parts of the medulla oblongata, where the centers of cardiovascular and respiratory regulation are located. However, when the focus of hemorrhage is located in any functional area, even a small volume of hemorrhage can lead to the appearance of neurological symptoms (for example, the development of contralateral hemiparesis when the focus is located in the precentral gyrus of the frontal lobe).
- Epileptic syndrome . In some cases, due to the chronic presence of hemosiderin in the medulla or with the development of acute hemorrhage, a focus of pathological brain bioactivity may form, clinically manifested by epileptic seizures of various structures (convulsive, non-convulsive, absence seizures, vegetative, polymorphic and others).
Thus, cavernomas extremely rarely pose a threat to the patient’s life, but can have a significant impact on the quality of life
How to diagnose a cavernoma?
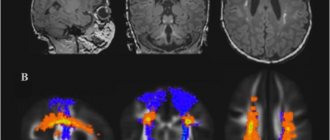
Magnetic resonance imaging (MRI) is the most informative method for diagnosing cavernomas. In T1 and T2 scanning modes, a cavity surrounded by a black rim of hemosiderin may be visible, with signs of acute and subacute hemorrhages. The most sensitive mode is T2* (“T2 with star”), which allows you to diagnose even small (1-2 mm) cavernomas that are not visible in other scanning modes
Computed tomography - its diagnostic value is limited, as a rule, to the acute period of hemorrhage (several days), when the image shows a focus of bleeding
Angiography is not informative in diagnosing cavernomas
How to get rid of a cavernoma?
In case of episyndrome formation and/or hemorrhage, two treatment methods are possible:
Surgical removal of cavernoma is a highly effective method that allows you to once and for all relieve the patient from the risk of repeated hemorrhages. Surgery is also effective if the patient has epileptic seizures, but its effectiveness is reduced in the case of a long history of epileptic syndrome
Radiosurgery is carried out according to the same principle as for arteriovenous malformations - the higher the dose, the better the effect. Therefore, cavernomas up to 1 cm in diameter are best treated, when the maximum permissible doses of radiation can be safely used. Morphological changes in this case are similar to those in arteriovenous malformations - the walls of the cavernoma and the mouths of the feeding vessels undergo hyalinosis, as a result of which the blood flow decreases, diapedetic hemorrhages stop, and the risk of repeated spontaneous intracerebral hemorrhages is reduced by 50-70%. Episodic attacks also become less frequent or disappear completely, but as in the situation with surgery, the longer the history of the disease, the less likely it is to completely recover from them
The generally accepted tactic for asymptomatic, incidentally detected cavernomas is observation.
Is it necessary to irradiate multiple cavernomas?
As in the case of single cavernomas, radiosurgical treatment is carried out only on the lesion that manifests itself clinically - hemorrhage or epileptic seizures
What to do with venous angioma?
The question often arises: how to get rid of venous angioma? Firstly, you should know that venous angiomas never manifest themselves as hemorrhages or epileptic seizures. Secondly, although they represent a venous network that is abnormal in structure, they nevertheless take full part in the local venous circulation of the brain. The only option for the appearance of clinical symptoms associated with venous angioma is the spontaneous development of thrombosis of the draining vein. This situation is more hypothetical than real. In this case, the patient will experience cerebral venous infarction with severe swelling at the site of impaired venous outflow. And only one way can help cope with such a situation - thrombolytic and anticoagulant therapy. Attempts to surgically or radiosurgically influence venous angiomas not only do not make any sense, but in a similar manner to thrombosis will lead to gross local disturbances of venous blood flow. Thus, the mere presence of venous angioma is not a reason for any treatment.
Which cavernoma treatment method is best?
From the point of view of preventing recurrent hemorrhages, the effectiveness of surgical treatment is higher. However, when cavernomas are localized in functionally important or hard-to-reach areas of the brain (for example, in the subcortical nuclei, brain stem), surgery itself has a high risk of residual neurological deficit, and radiosurgery can largely avoid these complications. Therefore, the decision on the optimal method of influence is made individually, taking into account all possible factors, incl. and taking into account the informed choice of the patient himself
Fig. 1 Result of radiosurgical treatment of brainstem cavernoma. On the left is a cavernous angioma of the lateral surface of the brain stem at the time of Gamma Knife radiosurgery. On the right - a significant reduction in the size of the cavernoma 3.5 years after radiosurgery. No recurrent hemorrhages
Possible consequences
After cavernous angioma is diagnosed, people worry about possible complications. The disease itself is not as terrible as its consequences. That is why patients should be regularly monitored by a specialist so that the condition can be monitored.
One of the most dangerous complications is bleeding . Tumors rupture, causing blood to flow into the brain. This phenomenon is difficult to stop and can cause neurological deficits. In the worst case, the person may fall into a coma, so it is important to treat the disease promptly.
Statistics show that the risk of complications is greatest in women under 40 years of age. Bleeding may also occur in those who have already had it. It is especially important for them to monitor changes in tumor size.
It is impossible to say with certainty how long a person with this pathology will live. Much will depend on his lifestyle, as well as the availability of treatment. You definitely shouldn’t let pathology take its course and hope that nothing will happen. You should listen to your doctor’s recommendations, because angioma is considered a dangerous disease that can lead to unexpected consequences.