The brain stem is an extension of the spinal cord. The structure of the trunk includes the medulla oblongata, the pons, parts of the midbrain and the cerebellum. The brainstem also includes the third ventricle, quadrigeminal tract, and thalamic nuclei. The trunk departments are responsible for:
- innervation of the muscles of the face and swallowing;
- distribution and synchronization of muscle tone;
- sensory information processing;
- activation of the cerebral cortex;
- respiratory and cardiovascular activity;
- the act of defecation and urination;
- support of the body in space;
In addition, this part of the brain acts as a transit between the higher parts of the nervous system and the spinal cord, that is, it ensures the functioning of the pyramidal system, which is responsible for fine coordination.
What is a brain stem tumor
The structure of the brain stem includes: the base, where the head trunk itself is located, consisting of two substances: gray and white. The trunk itself is small - only 7 centimeters in length. The spinal cord is on one side, and the diencephalon is on the other. Its components: medulla oblongata, pons, midbrain. All nerve nuclei are located in it. There are also centers responsible for: breathing, cardiac function, nerve endings, swallowing, coughing, chewing, salivation, gag reflex. The pons is responsible for the functioning of the eyes, facial muscles, tongue, neck, limbs and torso. Thanks to the work of the nerve nuclei of the medulla oblongata, the work of the muscles of the larynx and pharynx, gastrointestinal tract, hearing and speech of a person is regulated.
Given the importance of the brain stem, any damage or formation entails symptoms that affect health and sometimes life.
Treatment of brain tumors
Surgery
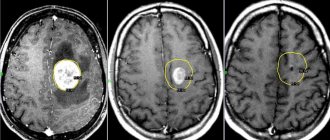
Surgical removal is the main treatment option for primary brain tumors. For low-risk neoplasias, this is usually the only treatment.
During surgical resection, the tumor can be completely or partially removed. In the second option, the positive effect is that the pressure on nearby brain structures is reduced and neurological symptoms are alleviated.
Surgical resection has also become the standard treatment for single metastases larger than 3 cm and in noncritical sites.
Surgical resection is more effective than radiosurgery. The survival rate of patients after surgery is almost twice as high as with radiosurgery. Only 13% of patients treated with surgery showed local recurrence, whereas 39% of patients treated with radiosurgery showed local disease progression.
Innovative cranial surgery techniques used in Belgium
- Intraoperative neuronavigation uses an advanced MRI system to map areas of the brain responsible for important functions. This visual map allows the operation to be performed accurately, without damaging important areas of the brain.
- Intraoperative electrophysiological mapping (motor mapping or language mapping) is like GPS navigation for the brain. Small electrodes are placed on the outer layer of the brain to stimulate the areas around the tumor. This helps to accurately determine the boundaries of an area, for example, responsible for speech or movement.
- Biofluorescence . The patient is given an injection of 5-aminolevulinic acid before surgery. This compound is actively absorbed by atypical cells. As a result, they begin to glow, which makes it possible to remove them as completely as possible.
- Laser ablation allows you to remove tumors without a large-scale opening of the skull (craniotomy). This ensures a faster return of the patient to normal life.
- Robotic surgery . Minimally invasive endoscopic surgeries using neurosurgical robots make it possible to remove tumors in the most critical areas. The movements of the robot's manipulator are 100 times more accurate than the movements of the surgeon's hands. This allows tumors to be removed literally cell by cell without resorting to craniotomy.
Multimodal surgery in clinics in Belgium
Intraoperative chemotherapy (BCNU) is the direct application of chemotherapy to the tumor area during surgery, which helps reduce the side effects associated with systemic chemotherapy, such as nausea and vomiting.
Another treatment option was intraoperative radiotherapy (IORT). With this technology, the tumor resection area is irradiated directly during surgery, helping to avoid damage to adjacent normal structures, especially the scalp and meninges.
Radiation therapy and radiosurgery
Radiation therapy (WBRT) is usually used to prevent relapses. Its effectiveness in the treatment of brain tumors is controversial, since it has been proven that, despite a decrease in the number of relapses, overall survival does not improve. For neoplasias that are well localized in the brain, conformal radiation (spot therapy) is recommended. This is radiation delivered strictly to the tumor and a small surrounding area.
However, irradiation of the entire brain is sometimes recommended when there are multiple tumors in the brain.
Stereotactic radiosurgery is also available for brain tumors in Belgium. This is high-intensity radiation that is very precisely aimed at a small area.
Clinics in Belgium use the most advanced options for stereotactic radiosurgery (SRS).
- Advanced Linear Accelerators, or LINACs, provide up to five times greater accuracy than previous generation sources, allowing for finer adjustments. LINAC can also be used to successfully target small lesions or deep, previously inaccessible tumors.
- Frameless Neurosurgical Stereotactic Radiotherapy (CyberKnife) - Unlike the outdated Gamma Knife technique, the new one no longer requires a frame to hold the head in place for highly focused radiation therapy, making surgery easier, more precise and with better protection of surrounding brain tissue for neurological improvements results.
- Stereotactic fractional radiosurgery (SBRT) is a high-intensity form of radiation where the total dose is divided into fractions. Several procedures are carried out throughout the week. This method provided more than 90 percent pain reduction and more effectively controlled tumor growth after one year of treatment.
Chemotherapy
Chemotherapy is usually given to patients with high-grade brain cancer as maintenance therapy. It can be used alone or in combination with other treatments, including surgery and/or radiation therapy.
Chemotherapy drugs can be given orally in tablet form or injected into a vein.
In Belgium, methods of injecting chemotherapy (and biological) drugs directly into the cerebrospinal fluid (CSF) or into the brain are being investigated. These methods increase the concentration of drug at the tumor site while reducing the side effects typically associated with systemic chemotherapy.
Biological therapy
Targeted therapy targets specific pathways or abnormalities in tumor cells. Targeted therapy is often combined with other treatments such as chemotherapy. This treatment is often an option for patients whose tumors recur after repeated treatments. The main drugs used in 2021 for brain tumors are bevacizumab and larotrectinib.
Immunotherapy is carried out in Belgium using modified T cells and dendritic cells. These methods are still at the stages of clinical trials and there are no approved protocols for their use.
Types of tumors
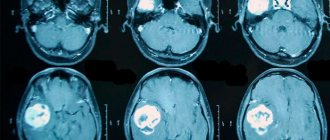
There are two types of tumors: primary and secondary. Disruptions in brain activity caused by harmful factors will ultimately lead to the chaotic division of damaged cells until they are completely replaced by healthy ones. This is how a primary tumor of the brain stem appears in children and older people. It is based on glial cells. Brain stem cancer can start and develop in one part of the organ. A common place for oncology to appear is the bridge (about 60%). Slightly less - in the midbrain and medulla oblongata. Brain stem tumors occur in the plural.
Secondary are those that appear in one place and continue to grow on the brain stem. Moreover, in only 5% of cases, metastases occur in the trunk, penetrating from other organs. A brain stem tumor is a parastem formation (para – about).
Common types of tumors are gliomas, which develop from glial cells.
- Astrocytomas account for about 60% of diseases. There are multiforme, pilocytic, anaplastic and fibrillary. Benign ones include pilocytic and fibrillary. Pilocytic forms occur in children. Glioblastoma (multiforme) is considered aggressive, which occurs most often in men under 50 years of age.
- Ependymomas account for 5% of all tumors. Most often it is benign.
- Oligodendrogliomas occur in 8% of diseases. Large tumor sizes. There are 4 degrees of malignancy.
Classification
Based on histological characteristics, tumors are divided into:
- Astrocytoma of the brain . It can be benign (fibrillary, pilocytic) and malignant (anaplastic, multiforme).
- Ependymoma . It is presented in a benign form, so hydrocephalus and intracranial hypertension are distinctive features. Occurs in children.
- Oligodendroglioma . An expansive-infiltrating form is characteristic. Malignancy varies from grade 2 to grade 4.
It is generally accepted to divide entities into:
- Benign . In the first case, slow growth is observed. The period for development exceeds a 15-year period. In 40 - 50% of patients, benign formations are diagnosed, which can turn into malignant.
- Malignant . The second case is malignant formations, which account for the majority of deaths.
The localization principle involves dividing tumors into:
- Primary . They are formed from a new growth of the trunk. Types: exophytic-stem and intra-stem.
- Secondary . Occur in the area of the fourth ventricle or cerebellar tissue. Other primary sources are kidneys, spine, spinal cord.
- Parastem . Find expression through stem deformation.
More than 1/2 of the tumors of the trunk are presented on the bridge. The remaining formations are diagnosed in the middle (no more than 20%) and medulla oblongata (no more than 25%).
The growth characteristics of formations predetermine the following development:
- Expansive . Occurs due to its own cells. As it grows, other tissues are pushed aside.
- Infiltrating . Microscopic examination does not reveal the boundaries of the formation. A diffuse tumor of the brain stem is characterized according to this principle.
Based on the type of growth, the following formations are distinguished:
- Nodal . The preservation of boundaries and areas of healthy tissue is inherent. Removed surgically.
- Diffuse . They make up the majority among other species (80%). Microscopically it is impossible to detect tumor-like boundaries. There is an ingrowth of defective cells into healthy areas of tissue with replacement. Surgery is accompanied by complications.
- Infiltrative (pseudonodular). Macroscopically, the boundaries are clearly defined. The microscopic method reveals the destruction of the nervous tissue around the formation. Infiltrative growth is present.
Symptoms
When gliomas appear, the destruction of brain stem tissue begins. Depending on the affected area, focal symptoms of the disease appear. Unfortunately, with the appearance of a tumor, other organs also suffer - the tumor, increasing in size, impairs blood circulation and increases intracranial pressure.
Brain stem tumor symptoms to look out for include:
- Headache. 90% of patients complain about it. The tumor puts pressure on the nerve endings, membranes, and blood vessels of the brain. It can appear both locally and be felt throughout the head. The intensity varies - from strong to dull. It occurs suddenly, most often in the morning.
- Nausea, sometimes with vomiting. Appears in the morning.
- Incorrect position. The patient prefers to hold the head in a manner that does not irritate the nerves in the neck and skull.
- Mental disorders. This symptom can be observed both locally and generally. Such disorders include deafness, irritability, and changes in consciousness. The patient feels lethargic, apathetic, does not want to talk, and does not react to anything.
- Epilepsy.
- Decreased visual acuity, which appears due to intracranial pressure. The fundus of the eye changes - the discs swell, their color changes.
- Bulbar syndrome.
- The structure of the skull changes - the seams diverge, its walls become thinner.
Focal symptoms include:
- Damage to motor functions, loss of orientation, tactile and visual perception disappears, gait changes.
- Hearing and sensitivity decrease.
- Paresis and tremors appear.
- Blood pressure surges.
- A facial disorder (distorted smile) appears.
- The clinical picture of brainstem tumors includes delayed onset of intracranial pressure and accumulation of cerebrospinal fluid in the brain (hydrocephalus).
There are many structures in the brain stem that can be affected. When central paresis is affected, tremor appears, dizziness occurs, problems with hearing and vision appear, strabismus may develop, and difficulty swallowing appears. Paresis in the limbs may occur. With the progression of tumor growth, these symptoms increase, and new ones appear - nausea, headache, vomiting. The patient dies due to malfunctions of the cardiac, vascular centers and respiratory organs.
Symptoms
Signs of a brain stem tumor include:
- Headache. The root cause is pressure on elements of the circulatory and nervous systems in the brain. Localization – local or general. Intensity ranges from negligible to unbearable. The nature of the manifestation is sudden or constant. Prerequisites: anxiety, physical activity. The consequences are tinnitus, loss of balance.
- Vomiting and nausea.
- Unnatural head position.
- Psychoneurological disorders.
- Epileptic seizures.
- Visual dysfunction. Present in 70% of cases. The root cause is pressure, which leads to compression of the optic nerve.
- Bulbar syndrome. The consequences are impaired speech and swallowing function.
- Changes in cranial structure.
- Disorders of the cardiovascular and respiratory systems.
Tachycardia and cardiomyopathy are diagnosed. Dysphagia and respiratory failure may also appear.
A feature of cancer development is the influence of a tumor from one part of the brain on other areas. The reason lies in the growth of the tumor, compression of blood vessels and increased pressure inside the skull.
Focal symptoms include:
- Gait disturbance, deterioration of motor functions.
- Blood pressure surges.
- Twitching of the muscles of the hands and eyes.
- Pathologies of the middle ear.
- Disorders of facial expressions.
Brain stem tumors in children are asymptomatic for a long time. The main symptom is lack of coordination. There is a decrease in activity, loss of appetite, and changes in behavior.
Stages of the disease
In medicine, there is a classification of oncological diseases. It is expressed in degrees:
- The first degree is benign. They grow slowly, up to ten years.
- The second degree is borderline.
- The third and fourth are the highest, having an indicator of malignancy. The growth of tumors is rapid - a person with similar degrees can live from a couple of months to several years.
Unfortunately, benign tumors can eventually develop into malignant tumors.
Focal symptoms
Some disorders do not appear in all patients. Their development is associated with focal brain lesions. The list of such symptoms includes:
- decreased sensitivity of the hearing organs (sometimes to the point of deafness);
- paresis and twitching of the eye muscles;
- motor disorders, in particular, problems with coordination, orientation in space, changes in gait;
- disturbances of visual and tactile perception;
- hand tremors;
- disturbances in facial expressions associated with weakness of the facial muscles (for example, asymmetrical smile);
- frequent and sudden jumps in blood pressure.
It is worth noting that as the tumor grows, the patient’s condition worsens - tachycardia, cardiomyopathy, dysphagia, and respiratory failure develop.
Causes of pathology
Oncology can occur for various reasons. Doctors call the most common heredity, genetic predisposition, exposure to chemicals, and radiation.
Deviations in genetics include the following syndromes: Turco, Li-Fraumeni, Gorlin, tuberous sclerosis, Von Recklinghausen's disease, Burkitt's tumor.
Unfortunately, medicine has not yet found the exact causes of cancer in humans. Therefore, to date, no remedy has yet been found to help prevent cancer.
Chemotherapy
A few weeks after surgery, additional radiation therapy may be used. Its standard types bring more negativity, so they usually resort to radiotherapy, which minimizes the harmful effects of radiation on tissues that are not damaged by the disease. For this, doctors select the optimal doses. During a course of therapy, the patient undergoes from 10 to 30 procedures, and the total volume of radiation is 70 Gy.
Skull cancer
Chemotherapy is most often used in conjunction with radiation. To increase effectiveness, several drugs are prescribed (carmustine, cisplatin and others). Before starting therapy, it is necessary to conduct tests to identify sensitivity to medications.
Diagnosis of a brain tumor
In order for the doctor to make a diagnosis, he must first collect an anamnesis. It is very important to answer all questions about symptoms as accurately as possible. If neurological abnormalities are observed, the patient must be sent to a neurologist.
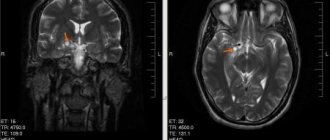
At his appointment, he undergoes an examination and various tests that reveal motor dysfunctions. The doctor will definitely check whether all reflexes are present and whether there is tactile and pain sensitivity. An examination by an ophthalmologist is required, where the patient's fundus is measured. If necessary, the patient is referred to an otoneurologist for a hearing test. After collecting anamnesis, the neurologist will be able to make a diagnosis. If necessary, a neurologist can prescribe CT and MRI, which help detect tumors of minimal size, determine the location of the tumor, and the type.
Additional studies include craniography (x-ray of the skull), which can show whether there is a change in the bones of the skull, encephalography (determining changes in the brain), echoencephaloscopy (ultrasound diagnostics), radioisotope scanning, angiography.
A biopsy is not performed for brain stem cancer. Histology is carried out solely on the basis of data on location, symptoms, and the age of the patient.
Types of neoplasms
According to the ICD (International Classification of Diseases) classifier, there are more than 120 types of brain tumors.
Primary tumors form in brain cells and are classified by cell type, or where they first develop. For example, astrocytomas form in star-shaped cells called astrocytes.
Most brain tumors are secondary . They are metastatic tumors that have spread from another area in the body. Lung cancer most often metastasizes to the brain, followed by breast cancer.
Are these neoplasms malignant?
More than 60% are malignant. For example, more than half of all gliomas diagnosed in adults are glioblastomas (a very aggressive brain cancer). Ependymomas and oligodendrogliomas can also be malignant.
But not all brain tumors are like this. Many meningiomas, craniopharyngiomas, and pituitary tumors are benign.
It is important to understand that even benign tumors can damage brain tissue and cause side effects such as headaches, fatigue, or blurred vision. Even if the tumor is benign, timely and appropriate treatment can be decisive for your health.
Astrocytomas
Astrocytomas are the most common tumor of the central nervous system. Occur anywhere in the brain and develop from small star-shaped cells called astrocytes.
gliomas are a type of astrocytoma that forms in the brain stem and controls many vital functions such as body temperature, blood pressure, breathing, hunger and thirst. Tumors in this area are difficult to treat. Most gliomas are high-grade astrocytomas.
Glioblastoma multiforme or grade IV astrocytoma is a fast-growing, aggressive type of malignant tumor of the central nervous system. Glioblastomas can appear in any lobe of the brain, but most often develop in the frontal and temporal lobes.
In addition to astrocytomas, there are other primary tumors that arise from glial cells. These include:
- Ependymomas, which usually arise in the lining of the ventricles or in the spaces of the brain. Although ependymomas can develop at any age, they are most common in children and adolescents.
- Oligodendrogliomas develop in cells that produce myelin, the covering that protects nerves. They are very rare, grow slowly and do not spread to surrounding tissues. Oligodendrogliomas most often occur in middle-aged adults and have a more favorable prognosis than astrocytomas.
- Mixed gliomas have two types of tumor cells: oligodendrocytes and astrocytes.
Nonglial neoplasias
There are a number of tumors that do not start in glial tissue.
Meningioma develops in the cells of the membranes that surround the brain. Meningiomas account for 15% of all intracranial neoplasias. Most of these neoplasms are benign. Some meningiomas may not require immediate treatment and may go undetected for many years. Most meningiomas are diagnosed in women aged 30 to 50 years.
Craniopharyngiomas develop in the area near the pituitary gland. These neoplasias are usually benign. However, they can create pressure or damage the hypothalamus and affect vital functions.
Germinoma is the most common type of embryonal malignant neoplasia in the brain. In addition to the brain, germinomas can form in the ovaries, testicles, breasts and abdomen. Most of these neoplasms occur in children.
Pineal neoplasias occur in or around the pineal gland, a small organ located in the center of the brain. They can be slow-growing (pineocytoma) or fast-growing (pineoblastoma).
Medulloblastomas are fast-growing neoplasias that develop from cerebellar neurons. The cerebellum controls movement, balance and posture. They are usually found in children or young adults.
Primary CNS lymphomas develop in the lymphatic tissue of the brain. This type of neoplasia usually occurs in people who have a compromised immune system.
Pituitary tumors
The vast majority of pituitary neoplasias are pituitary adenomas, benign growths that do not spread beyond the skull. Although these tumors are benign, they often cause problems because they can cause the pituitary gland to produce excess hormones.
Treatment
The most effective methods include operations that are aimed at removing tumors.
During the operation, the doctor cuts off the largest part of the formation. To perform the operation, the patient needs to open the skull. In some cases, surgery is not performed on the brain stem, since there is a high probability that vital centers may be affected. The decision on the need for surgery is made based on the size of the tumor and location. The tumor is cut off using endoscopic or laser removal. The laser option cauterizes the edges of the tissue and stops bleeding. The operation is performed using a robotic system, minimizing all kinds of complications.
Radiosurgery is radiation therapy that is based on the use of a single exposure to a high dose of radiation. Used for relapses and metastases.
HIFU therapy, which uses high-intensity ultrasound.
Cryodestruction – freezing with liquid nitrogen. To perform this you need a cryoprobe. The photo below describes the mechanism of action of cryotherapy. The mechanism in the brain is similar.
What types of tumors are there?
Any person knows that tumors can be malignant and benign. This classification is quite fair for a number of organs, but is completely unsuitable for the brain. Here, tumors are usually classified according to the type of tissue from which they developed.
Most often, brain tumors develop directly from brain tissue. These tumors are called neuroepithelial tumors and account for about 60 percent of all cases. The most common glioma in humans is a tumor that develops from glial cells, the supporting tissue of the brain.
Related links
- Opera singer Dmitry Hvorostovsky was diagnosed with a brain tumor
- “Brilliant” star: singer Zhanna Friske passed away
Gliomas can be either benign or malignant, in which case they are classified as glioblastomas. The latter type is practically untreatable. The main difficulty is that glioblastomas grow into surrounding tissues, often reaching vital centers, which in no case should be affected during surgery.
The second most common is meningioma, a tumor that develops from the meninges. Meningiomas are benign, grow slowly and are often completely asymptomatic. For this reason, it is very difficult to detect such a tumor at an early stage. As a rule, meningiomas can be removed.
"Lifestyle": What are the symptoms of a brain tumor
Tumors of the pituitary gland and cranial nerves, as well as metastases from other organs where neoplasms arose, are less common.
Radiation and chemotherapy
After the operation, radiation therapy is prescribed 14-21 days later. Doctors use radiotherapy (external beam radiation). The course ranges from ten to thirty procedures. Radiation dose – up to 70 Gy. If there are many metastases and malignant astrocytomas, it is necessary to irradiate the head. Radiation dose – up to 50 Gy. This treatment is suitable for inoperable patients who have a diffuse type of oncology.
Chemotherapy is carried out along with education. Treatment for diffuse brainstem tumor is a course of several drugs. The duration of treatment with chemotherapy should be from 1 to 3 weeks. After a break, repeat. During treatment, tests are taken that will show whether chemotherapy needs to be continued or whether it will be cancelled.
Causes of tumor formation
Why does a brain stem tumor form? The reasons, unfortunately, are not always clear, because the mechanisms of cancer development are not fully understood. Scientists have been able to identify some risk factors.
- There is genetic inheritance. Statistics show that most often patients with a brain stem tumor had relatives with one or another cancer.
- Risk factors also include some genetic diseases, in particular, tuberous sclerosis, Turco syndrome, Recklinghausen disease, Gorlin syndrome, etc. The presence of such pathologies increases the likelihood of developing brain cancer.
- Long-term exposure to chemicals, particularly mercury, arsenic, and lead, is potentially dangerous.
- There are certain age groups at risk - children aged 5 to 7 years old, as well as older people 65-70 years old, are at risk.
Of course, poor ecology, poor nutrition, bad habits, and a weakened immune system contribute to the development of cancer, but only if the prerequisites are present.
Forecast
Unfortunately, the prognosis is disappointing. Even after a complex of treatment, the survival rate is 60%. If a patient is contraindicated for surgical intervention or has an advanced disease, he or she is less likely to live 5 years (the patient is one of 30-40% of people).
People with the most aggressive forms of cancer live no more than one year. Unfortunately, some survive only a few months. Children, due to their growing bodies, have a better chance of surviving than adults or older people.
People with certain diseases: non-Hodgkin's lymphoma, brain stem cavernoma, sarcoma tumor, HPV, lymphoma tumor, unfortunately, will not be able to live long.
Stages of disease development
A brain stem tumor, like almost any other neoplasm, grows and develops in several stages.
- The first stage is accompanied by the formation of a small tumor - its diameter does not exceed three centimeters. It has clear edges and does not spread to nearby tissue. Unfortunately, this stage is rarely accompanied by any symptoms, so the disease is rarely diagnosed at the first stage.
- The second stage is characterized by the growth of the tumor - its size already exceeds 3 cm. However, the tumor retains clear edges. The first symptoms appear, but patients very often write everything off as a common malaise.
- At the third stage, the tumor grows into nearby structures, for example, into the ventricles of the brain.
- Stage four is no longer just a brain stem tumor. At this stage, the disease is accompanied by the rapid formation and growth of metastases throughout the body. During this period, the disease is practically untreatable.
Tumors of the cerebral hemispheres
In the clinic of brain tumors, three groups of symptoms are distinguished: general, or cerebral, focal, and symptoms at a distance (secondary focal).
The complex of general cerebral symptoms that occur with tumors due to increased intracranial pressure is called hypertension syndrome.
Symptoms of increased intracranial pressure include: headache, vomiting, dizziness, changes in pulse, psyche, epileptic seizures, damage to the cranial nerves, changes in the skull bones, liquor-containing spaces and cerebrospinal fluid, as well as changes in the fundus.
Headache —
the most common symptom of a brain tumor.
Local headache, felt in a certain part of the head, can occur due to irritation by the tumor of the cranial nerves (branches of the trigeminal, glossopharyngeal, vagus nerves), the walls of the venous sinuses, the adjacent membranes, large meningeal and cerebral vessels. In addition to local headache, brain tumors also cause general headache. The pathogenesis of general headache is associated with increased intracranial pressure. A general headache can be deep, tearing, bursting, and very intense. Headache due to brain tumors is rarely constant and progressively increasing; more often it occurs in the form of separate attacks. The appearance of a headache in the morning is especially typical; it often appears during excitement and especially during physical stress (when coughing, sneezing, lifting something heavy, etc.). Headache may depend on the position of the head and body in space. Forced head position
with tumors occurs reflexively due to irritation of the cranial nerves and upper cervical roots, due to the effect of the tumor on the movement of cerebrospinal fluid and irritation of the labyrinth.
Vomiting usually occurs easily and unexpectedly, without preceding nausea, and morning vomiting that occurs on an empty stomach is especially common. Vomiting is very often provoked by a change in head position. For the most part, vomiting occurs at the height of the headache. Pathogenetically, vomiting in brain tumors is associated with increased intracranial pressure, but it can also be a focal symptom if the tumor is localized subtentorially.
Dizziness manifests itself in the form of apparent rotation of oneself or surrounding objects in a certain direction (“systemic” dizziness), as well as in the form of a feeling of instability, swaying, lightheadedness, sudden weakness, darkening of the eyes, loss of balance. Dizziness is often accompanied by nausea, vomiting and is usually not constant, but periodic. Dizziness most often occurs with tumors affecting the vestibular part of the VIII pair or its pathways in the brain stem and cerebellum. It is less common in hemispheric tumors.
Changes in fundus and visual acuity —
one of the most important objective symptoms of a brain tumor. Changes in the fundus of the eye manifest themselves in the form of stagnation and atrophy of the optic discs and hemorrhages in the peridiscal regions of the retina. The occurrence of congestive discs in brain tumors is associated with mechanical compression of the optic nerve and blood vessels due to increased intracranial pressure. As a result of stagnation of venous blood, swelling and protrusion of the optic disc and the surrounding retina occurs. It is possible that intoxication phenomena also play a role in the origin of congestive discs in brain tumors. Stagnant discs are characterized by a change in color, they become grayish-red, the boundaries of the disc disappear, the edematous retina surrounding the disc becomes cyanotic, dilated veins are lost in it, the disc increases in size and protrudes forward. Hemorrhages appear along the vessels. The final stage of stagnant discs is their secondary (white) atrophy.
With brain tumors, atrophy of the optic nerves can also be primary, gray, if the tumors affect the optic nerves, optic chiasm or optic tracts.
Stagnant discs are usually bilateral, but sometimes asymmetry occurs. A peculiar phenomenon is observed when the tumor is localized at the base of the frontal lobe: primary atrophy develops on the side of the tumor, and a stagnant disc (Foster-Kennedy syndrome) develops on the other side.
Subjective signs accompanying congestive discs are a short-term weakening of vision in the form of a feeling of fog or a veil before the eyes. With the onset of optic nerve atrophy, a persistent decrease in vision appears.
Mental changes quite often accompany brain tumors and can be observed in tumors of any location. The pathogenesis of mental disorders in brain tumors is very complex. In some cases, mental disorders are caused by hypertension syndrome, in some cases they represent a focal symptom.
The most common mental disorders associated with brain tumors include disorders of consciousness. They can occur paroxysmally, in the form of attacks, but more often they develop gradually, when stupor turns into stupor, then into a coma, from which the patient cannot be brought out. Impairments of consciousness such as stunning are observed in the later stages of the disease, against the background of hypertension syndrome. Patients cannot follow the course of the conversation; they speak slowly, with stops; they are lethargic, indifferent, silent, and stop responding to speech addressed to them.
Epileptic seizures. The expression of hypertension syndrome in brain tumors is convulsive seizures. They can occur with tumors of various locations (usually tumors of the temporal and frontal lobe). Focal, Jacksonian seizures have topical and diagnostic significance.
Damage to the cranial nerves
occurs in hypertension syndrome due to increased pressure on their nuclei located in the area of the midbrain aqueduct and at the bottom of the fourth ventricle, due to pressing of the intradural segments of these nerves to the bones of the skull base, due to compression of the roots and nuclei of the nerves due to protrusion of parts of the brain into the foramen of the cerebellar tentorium, Bichat's fissure, or into the foramen magnum.
The function of the group of oculomotor and bulbar nerves is especially often impaired. It should be remembered that damage to the cranial nerves is often a focal symptom of the tumor. Changes in pulse and respiration are observed in the later stages of the tumor. They manifest themselves in bradycardia and tachycardia, often replacing each other. Bradycardia is common, accompanying headache and vomiting. In the terminal stage of the disease, tachycardia is observed. The appearance of persistent tachycardia, especially after bradycardia, is an unfavorable prognostic sign. Changes in breathing, like the pulse, can be expressed in slowing down, speeding up, or rhythm disturbances. Impaired breathing, especially slowing it down, indicates an alarmingly serious condition of the patient.
Changes in cerebrospinal fluid. Cerebrospinal fluid pressure is most often elevated, but with tumors that disrupt the communication between the ventricles and the subarachnoid space, it can decrease. A change in the composition of the cerebrospinal fluid is expressed in an increase in protein, usually 2-3 times compared to normal. Sometimes the content of cellular elements increases due to lymphocytes. Tumor cells are rarely found. Among other changes in the cerebrospinal fluid, xanthochromia deserves attention.
Changes in the skull bones,
caused by an increase in intracranial pressure, are expressed in the general thinning of the flat bones of the skull, in the deepening of digital impressions, in the divergence of sutures. In addition, some parts of the skull that are particularly sensitive to increased intracranial pressure change - the back of the sella turcica, the sphenoid processes, the small wings of the main bone, the openings through which nerves exit the cranial cavity.
With tumors, local changes in the bones also occur in the immediate vicinity of the tumor (eatenness, exostoses, etc.).
Changes in the liquor-containing spaces of the brain.
With an increase in intracranial pressure, the size and position of the ventricles of the brain and subarachnoid spaces change. These changes depend on the accumulation of cerebrospinal fluid in the ventricles, the mass and location of the tumor. With tumors in the posterior fossa, cerebrospinal fluid accumulates in the lateral and third ventricles. Changes in the ventricles with intraventricular tumors depend on the location of the latter. With tumors of the cerebral hemispheres, the part of the lateral ventricle of the same name in which the tumor develops is first compressed, deformed and displaced. The subarachnoid space disappears as intracranial pressure increases;
The brain cisterns also decrease.
Focal symptoms
of brain tumors depend on the location of the tumor.
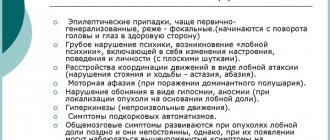
They are extremely diverse. For tumors of the frontal lobes
a mental disorder occurs. Inertia and inhibition of mental processes are especially characteristic. Patients are spontaneous, lack initiative, lack criticism of their condition, and become unkempt. When the tumor is localized in the lower parts, the phenomena of disinhibition, aggressiveness, a tendency to flat jokes, and moria predominate. Inertness of mental processes is combined in patients with motor inertia, and frontal or premotor apraxia occurs. Tumors of the frontal lobes are characterized by epileptic seizures. Seizures often begin with a combined rotation of the head and eyes in the direction opposite to the tumor. When the process is localized in the left hemisphere, motor aphasia and agraphia occur. Frontal ataxia may develop on the side opposite the tumor. Paresis of the limbs appears when the tumor is located in the posterior part of the frontal lobe. Pathological reflexes of oral automatism and grasping phenomena are characteristic. With basal localization of the tumor, the sense of smell is impaired, and Foster-Kennedy syndrome appears.
Tumors of the precentral gyrus
begin with Jacksonian seizures. Initially, cramps are limited to a small group of muscles corresponding to the location of the tumor. Gradually they acquire a tendency to spread to neighboring muscles, and then the seizures, starting with focal ones, become generalized. As the tumor grows, seizures begin to be accompanied by muscle weakness. Paresis is initially transient, then becomes persistent and gradually turns into paralysis.
Tumors of the postcentral gyrus
are characterized by sensory Jacksonian seizures, which are gradually joined by persistent sensitivity disorders on the side opposite the tumor.
Tumors
parietal lobes are characterized by the presence of sensory disorders. First of all, complex types of sensitivity are impaired (sense of localization, discrimination, two-dimensional spatial sense, stereognosis). Patients lose orientation in their own parts of the body (violation of the body diagram). Parietal apraxia occurs, patients lose the ability to perform usual actions. When the parietal lobe of the left hemisphere is damaged, reading, writing, and counting suffer, while oral speech is preserved.
For tumors of the temporal lobes
characterized by epileptic seizures. Sometimes there are olfactory, gustatory or auditory auras or hallucinations. Temporal ataxia often occurs. When the left temporal lobe is damaged, speech (sensory, semantic aphasia) and associated reading and writing are impaired. Due to the impact of the tumor on neighboring areas of the brain, brainstem symptoms (Weber syndrome) and signs of damage to the subcortical nodes (parkinsonism) may appear.
Tumors of the occipital
lobes are accompanied by central homonymous hemianopia. When the cortex is irritated, photopsia occurs (a feeling of flickering sparks, spots, etc. before the eyes). Formal visual hallucinations are rare. Metamorphopsia and visual agnosia may occur.
Tumors
thalamus causes sensitivity disorders, hyperpathy and thalamic pain. Due to the proximity of the internal capsule to the conducting pathways, the functions of all analyzers are often disrupted and pyramidal disorders occur.
For brain stem tumors
cranial nerves are affected. Alternating syndromes are typical and gradually progress as the tumor grows (70).
Tumors of the cerebellopontine angle.
These are usually neuromas of the vestibulocochlear nerve or meningiomas. The first symptom of a tumor is tinnitus, which is accompanied by hearing loss. Damage to the vestibulocochlear nerve is accompanied by paresis of the facial muscles and impaired sensitivity on the corresponding side of the face. When the vestibular part of the VIII pair is involved, nystagmus and dizziness are observed. As the tumor grows, cerebellar symptoms appear on the side of the same name and pyramidal symptoms on the opposite side.
For cerebellar tumors
the main focal symptom is ataxia, dysmetria, adiadochokinesis, decreased muscle tone. All these symptoms in tumors of the cerebellar hemisphere are expressed on the affected side; in tumors of the vermis they are bilateral. Worm tumors are accompanied by particularly severe disturbances in balance and gait. Pyramidal pathology is usually mild.
Pituitary tumors.
Pituitary adenomas are characterized by the early appearance of bitemporal hemianopsia, primary atrophy of the optic nerves and an increase in the size of the sella turcica, which can be completely destroyed in large tumors. Disorders of carbohydrate and water metabolism (polydipsia, polyuria) are often observed. Eosinophilic adenoma is characterized by acromegaly, chromophobic adenoma is characterized by adiposogenital dystrophy, and basophilic adenoma is characterized by Itsenko-Cushing syndrome.
Symptoms at a distance.
In addition to the primary focal symptoms, caused by the location of the tumor and its direct effect on the brain tissue, there are also secondary focal symptoms, or symptoms at a distance. These include symptoms nearby and distant.
Neighborhood symptoms are dysfunctions of areas of the brain or cranial nerves located close to, but outside the parts of the brain directly affected by the tumor. These include, for example, paralysis of the oculomotor nerve with a tumor of the temporal lobe or signs of damage to the medulla oblongata with tumors of the cerebellum.
Distant focal symptoms —
These are dysfunctions of parts of the brain or cranial nerves significantly removed from the location of the tumor. Examples of long-term symptoms include Jacksonian seizures or bitemporal hemianopia due to posterior fossa tumors. Symptoms at a distance usually appear later and are less pronounced than the primary ones.
Diagnostics
If a brain tumor is suspected, only a neurologist can prescribe an examination. First, he will examine the patient, check his reflexes and vestibular functions. Then he will refer you for examination to related specialists: an ophthalmologist (he will examine the fundus of the eye), an ENT doctor who will evaluate your hearing and sense of smell. Electroencephalography will be performed to determine the focus of convulsive readiness and its degree of activity. Simultaneously with assessing the damage, it is necessary to make a diagnosis by identifying the location and volume of the tumor. The following methods will help with this:
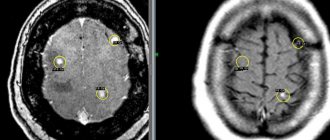
- Magnetic resonance imaging is a method that can be used by persons without metal parts in the body (pacemaker, joint replacements, fragments of explosive devices).
- CT scan. It is not as effective as MRI in diagnosing a brain tumor, but can be performed if the first method is not possible.
- Positron emission tomography helps to clarify the size of the tumor.
- Magnetic resonance angiography is a method that allows you to examine the vessels feeding the tumor. This requires the introduction of a contrast agent into the bloodstream, which will also color the capillaries of the neoplasm.
All these methods can only “give” an idea about the histological structure of the tumor, but accurately determining it in order to draw up a treatment plan for a brain tumor and prognosis is only possible with the help of a biopsy. It is performed after constructing a 3D model of the brain and the tumor in it in order to insert the probe strictly into the pathological area (stereotactic biopsy).
In parallel with the diagnosis, other research methods are performed to determine the stage of the tumor: instrumental diagnostics of those cavitary organs into which the brain tumor could metastasize is performed.