Brain toxoplasmosis is a parasitic disease caused by Toxoplasma gondii. The microorganism is a protozoan. In appearance they resemble the lobes of an orange.
The parasite is capable of infecting all internal organs and systems: the brain and spinal cord, liver, heart, spleen, etc. In many cases, toxoplasmosis is chronic and difficult to treat.
What to do in such a situation? To get started, we recommend reading this article. This article describes in detail methods of controlling parasites. We also recommend that you consult a specialist. Read the article >>>
Toxoplasma gondii
Causes of toxoplasmosis
In nature, Toxoplasma is the causative agent of a dangerous brain infection and is quite widespread. However, the simplest microorganisms can reproduce only in the body of a warm-blooded host - cats, cows, birds.
Infection with toxoplasmosis can occur in different ways:
- through direct contact with an already infected animal - for example, children are typically infected when playing with cats, putting particles of their excrement into their mouths, or infection due to scratches;
- during excavation work - replanting plants in the garden, the soil in which contains contaminated biomaterial from animals;
- upon contact with raw meat from an animal infected with toxoplasmosis;
- due to consumption of animal products - for example, raw milk, eggs that have not undergone sufficient heat treatment.
Less frequently recorded are cases of brain infection by protozoa transferred through the bloodstream during the transfusion of its components if the donor had toxoplasmosis. It is extremely rare that infection occurred when poorly treated medical instruments were used.
A congenital form of cerebral toxoplasmosis is possible when the infection passes from an already infected woman to her baby during its intrauterine development. Children are born with various anomalies and defects - both from the structures of the skull and other internal organs.
Pathogenesis of brain damage
Entering the body through the digestive tract, Toxoplasma is released from the membrane and penetrates the lymph nodes.
They then reach the brain through the bloodstream. In the substance of the brain, toxoplasma accumulates in certain areas, forming granulomas. Under normal conditions, the process stops here and granulomas can exist in the brain for a long time. If the body's defenses are reduced, the parasite is activated and an inflammatory process develops.
After Toxoplasma enters the human intestine, the microorganism spreads throughout the body through the blood and lymph. It has a certain affinity for the nervous structures of the brain. During normal functioning of the human immune system, the infectious process in tissues is limited to the formation of specific granulomas.
At the same time, Toxoplasma itself does not die; it can remain dormant for a long time. Decreased immunity leads to activation of toxoplasma. They are released from granulomas and cause the development of an inflammatory process in the brain. A decrease in immune status occurs under the influence of several factors.
The first reason is congenital weakness of the immune system, caused by changes in the functional activity of certain genes. The condition develops already in childhood. Depending on the extent of gene changes in congenital immunodeficiency, cerebral toxoplasmosis can be severe.
The second reason is acquired immunodeficiency, which is more pronounced in HIV, AIDS (infection with a specific virus). Less commonly, a decrease in immunity, causing the development of cerebral toxoplasmosis, can occur:
- with prolonged intoxication of the body caused by nicotine, alcohol or narcotic substances;
- for chronic infections;
- with insufficient or improper nutrition;
- with regular lack of sleep.
Depending on the cause of decreased immunity, the treatment of cerebral toxoplasmosis is determined.
Classification
To facilitate the diagnosis of toxoplasmosis and timely detection, a simple classification of the infection has been developed:
According to the mechanism of infection: congenital toxoplasmosis, acquired type of disease.
According to the nature of the infection: acute toxoplasmosis, latent form, chronic course of the disease.
By age criterion:
- toxoplasmosis of newborns;
- infection in preschool children;
- adolescent toxoplasmosis;
- infection in people 20-55 years old.
In addition to all of the above, some experts identify a special subgroup of toxoplasmosis - a secondary hidden variant of the disease.
The diagnosis is made based on the presence of residual manifestations of toxoplasmosis - calcifications, scars on the brain tissue.
Acute acquired toxoplasmosis
Pathology in the acute form begins suddenly - within 8–10 hours after the protozoa penetrates the bloodstream, and from there into the brain. The patient complains of symptoms of general intoxication of the body:
- temperature is high, can reach 39-40 degrees, while fluctuations can reach a significant range throughout the day;
- weakness – growing quickly, a person literally does not have enough strength to carry a spoon of soup to his mouth;
- headache - diffuse, but more in the temporal, parietal region of the skull;
- discomfort in the muscles of the whole body - increases when trying to perform physical work, stiffness in the shoulder girdle;
- sleep disorders - difficulty falling asleep, intermittent dreams;
- appetite is reduced, up to complete absence.
Against the background of nonspecific symptoms of intoxication from the onset of infection, people will also experience specific manifestations of brain toxoplasmosis:
- generalized lymphadenopathy - an increase in size and severe pain in the nearest subgroups of lymph nodes;
- encephalitis – inflammation of brain tissue;
- meningoencephalitis - damage to the inflammatory process of the meninges;
- encephalomyelitis – infection of both the spinal cord and the brain.
The prognosis will be more favorable if a person seeks medical help in a timely manner - at the first signs of deterioration in health. The infection requires complex treatment with modern drugs that can suppress the activity of protozoan microorganisms.
Therapy
If the tests show a positive result for the presence of infection, you should immediately begin to fight the disease. How to treat toxoplasmosis? A doctor will be the best person to answer this question; it is only within his competence to prescribe adequate therapy, especially when it comes to the presence of infection in pregnant women or children.
The pathology is treated in acute form with medications; as a rule, they include a group of chemotherapeutic drugs, such as delagil or fansidar. Also antibacterial drugs, tetracyclines, antihistamines and, of course, restorative therapy with a complex of vitamins.
Treatment with folk remedies cannot completely replace traditional therapy, but you can still use some recipes.
Garlic with milk is one of the oldest folk remedies in the treatment of toxoplasmosis. You should open a few cloves of garlic in half a liter of milk and drink in small sips throughout the day. Treatment should be continued for ten days.
Another folk remedy provides the following fee:
- chamomile;
- sagebrush;
- tansy;
- gentian;
- buckthorn bark.
All herbs for this folk remedy should be taken in 50 grams, mixed and every day brew a tablespoon of the mixture in a glass of water. You need to leave the decoction overnight to infuse and drink it in the morning on an empty stomach.
Folk remedy made from pumpkin seeds. The seeds are crushed, poured with milk and drunk in the morning on an empty stomach.
Horseradish root is grated on a fine grater, mixed with a tablespoon of sour cream and eaten at lunch. This folk remedy should not be used by people with problems in the gastrointestinal tract.
Propolis tincture is also one of the folk remedies used in the treatment of toxoplasmosis. The tincture should be taken before meals, three times a day. When treating with this folk remedy, you should not drink milk.
Any of the listed folk remedies requires consultation with the attending physician and parallel drug treatment. After completing the course, you should take a re-test. Pregnant women should be especially careful about any experiments on their health.
Symptoms of chronic toxoplasmosis
Toxoplasmosis of the brain can occur latently for many years - with a gradual onset and periods of exacerbation / subsidence of unpleasant manifestations. A typical symptom of infection is prolonged low-grade fever - a slight rise in temperature to 37.5–37.7 degrees for 3-5 days or weeks.
At the same time lymphadenopathy is observed - an increase in the cervical, occipital, axillary lymph nodes, as well as a headache - diffuse, of moderate intensity.
Damage to the structures of the central nervous system by toxoplasmosis manifests itself in hypertension, as well as diencephalic syndrome:
- fluctuations in intracranial pressure;
- deterioration of vision and hearing;
- dizziness;
- sleep disorders;
- paresis/paralysis of varying severity;
- vomiting that does not bring relief;
- fluctuations in blood pressure and pulse;
- epilepsy attacks.
In the chronic course of toxoplasmosis, pathological changes affect not only the structures of the brain, but also other internal organs. Thus, patients note the appearance of muscle pain - in the limbs, which intensifies with exercise.
On the digestive side, toxoplasmosis provokes loss of appetite, nausea, and difficulty defecating. For women, toxoplasmosis can result in infertility due to the inflammatory process in the ovaries and fallopian tubes.
Brain toxoplasmosis in HIV
The cerebral form of the disease is common among people with immunodeficiency syndrome. In patients with HIV status, the infection is particularly severe. In this case, toxoplasmosis becomes the cause of death.
Basically, the pathology manifests itself in the form of meningoencephalitis with foci of extensive brain damage.
All this leads to partial or complete paralysis, loss of vision and mental disorders.
Manifestations of congenital toxoplasmosis
Congenital brain toxoplasmosis is an infection that develops in a child at the stage of intra-tubal growth and development . As with the acquired variant of damage to brain structures, acute as well as latent forms can be distinguished - in direct dependence on the time of infection, the degree of development of immunity in the baby and the woman who gave birth to him.
So, if agents of toxoplasmosis entered the child’s body shortly before the moment of birth, then the baby is born with a subacute version of the infection - the brain is slightly affected. This will be manifested by symptoms: sleep disturbance, increased tearfulness, rare seizures, loss of appetite.
With timely comprehensive treatment, negative symptoms are eliminated, and the child develops further according to his age.
However, infection with toxoplasmosis in early pregnancy threatens children with severe irreversible changes in the brain:
- hydrocephalus - an increase in the size of the ventricles due to the accumulation of intracerebral fluid;
- convulsions – epilepsy of varying severity;
- intellectual disorders, up to complete dementia.
Most children with congenital toxoplasmosis die in the first year of life, and those who survive become severely disabled and require lifelong care.
Symptoms
Signs of toxoplasmosis are varied, usually depending on which organ was affected. It is also important to note that in children the congenital form of the disease is much more complicated than that acquired in adults.
Acquired toxoplasmosis in women, men or children is in most cases barely noticeable, practically asymptomatic.
In the acute course of the pathology, the following signs may appear:
- high body temperature;
- chills and fever;
- muscle and joint pain;
- severe weakness;
- headache;
- enlarged lymph nodes and affected organs.
Chronic toxoplasmosis also proceeds practically without showing itself for a single year.
Over time, people may experience symptoms such as:
- increased fatigue;
- irritability;
- systematic causeless increase in temperature;
- frequent headaches;
- visual impairment;
- disturbances in the functioning of the organs where the infection occurred.
- Concomitant pathologies may develop:
- toxoplasmosis encephalitis with brain damage;
- myopia;
- impotence in men and disruptions in the menstrual cycle in women;
- endocarditis;
- flatulence, etc.
Symptoms of toxoplasmosis in pregnant women may not appear at all or may have the signs described above. The greatest danger belongs to the fetus, if a woman is infected in the early stages of pregnancy, spontaneous abortion often occurs, since the embryo undergoes certain mutational processes that are incompatible with its further intrauterine development. If the child continues to develop and is born, then he will be diagnosed with severe injuries to his internal organs. If toxoplasmosis during pregnancy occurs towards the end of the second or third trimester, the birth of a child is more likely, but in 60% of cases such children are born with complex pathologies, which, unfortunately, are not always compatible with life. When a woman is infected at the end of pregnancy, the pathology may manifest itself in the newborn in a latent, mild form. The severity of the injuries depends on the duration of the influence of the parasites on the fetus; for this reason, infection in the first trimester often provokes a miscarriage. Children who are nevertheless born are diagnosed with various diseases and pathological processes, these include:
- low muscle tone;
- encephalomyelitis;
- disturbances in the functioning of the brain and the entire central nervous system as a whole;
- pathological enlargement of the liver, spleen, gall bladder;
- yellowness and rash on the skin;
- strabismus, blindness and other developmental defects.
Diagnostics
Despite the presence of characteristic symptoms and signs of damage to the infectious process of the brain, it is possible to make the correct diagnosis of toxoplasmosis only after laboratory diagnostics:
- enzyme immunoassay of blood for the presence of igg or igm antibodies, or igg avidity - the strength of bonds between antibodies and antigens in the patient’s bloodstream;
- general and biochemical blood tests - to confirm the weakening of the body due to infection.
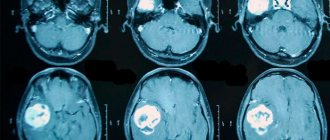
Of the instrumental methods for detecting toxoplasmosis in brain structures, computed tomography and magnetic resonance imaging are decisive. With their help, it is possible to diagnose the smallest foci of infection in the form of calcifications, scars, pathological enlargements, and cysts.
The specialist will make the final diagnosis of toxoplasmosis using a combination of information from laboratory and instrumental methods of examining the brain.
Self-diagnosis is unacceptable - for example, it is difficult for a person unfamiliar with medical terminology to understand between igg and igm antibody titers. Only a doctor can correctly interpret the analysis and select the optimal treatment regimen for the infection.
What would the attending physician want to know?
- Differential diagnosis with lymphoma, fungal infection and neurosyphilis
- Dynamic studies.
What specialties do doctors diagnose and treat meningeal toxoplasmosis?
— Infectious disease specialist (pathogen identification)
-Neurologist (determination of brain dysfunction)
— Functional diagnostics doctor (differential diagnosis with other diseases, confirmation of the disease)
Treatment tactics
Drug therapy for toxoplasmosis should begin immediately after laboratory tests have confirmed a high concentration of infectious pathogens in the bloodstream.
Main subgroups of medications:
- chemotherapeutic agents - for example, Delagil, Fansidar;
- antibacterial drugs - usually tetracycline;
- antihistamines - Zodok, Tavegil, Suprastin;
- restoratives - vitamin complexes with microelements.
In addition to the above subgroups of pharmaceutical drugs, the patient will be given recommendations for lifestyle modifications in order to increase the body's defenses. So, the doctor will recommend:
- eat right - the diet should contain more vegetables and various fruits;
- sleep more - the brain needs more time to recover;
- avoid contact with other infected patients so as not to additionally become infected with influenza or acute respiratory infections;
- give up bad habits – consumption of tobacco and alcohol products;
- reduce the severity of stress - take sick leave or days off as vacation and stay at home, so as not to conflict with anyone, let your body gain strength.
Both in acute toxoplasmosis and in its chronic course, the main emphasis in treatment tactics is aimed at raising immune barriers. Therefore, doctors recommend, in addition to drug therapy, also spa treatment, aromatherapy, and acupuncture.
Traditional medicine recipes also come to the rescue - various decoctions and infusions of medicinal herbs, which also have the ability to suppress the inflammatory process and strengthen the immune system. For example, garlic and chamomile, wormwood and gentian, and propolis tincture have proven themselves to be excellent.
Treatment of cerebral toxoplasmosis
The chronic form is difficult to treat. Mostly immunomodulatory drugs and vitamin complexes are prescribed. Among the medications, Levamisole, Cerebrolysin (nootropic drug) and other drugs are used.
The acute form is stopped with the help of medications: Pyrimethamine + Sulfadiazine, Trimethoprim with Sulfamethoxazole, Lincomycin hydrochloride, Rovamycin and others. The doctor prescribes the treatment regimen and dosage based on the patient’s condition, individual characteristics, etc.
Prevention
Any infection, including toxoplasmosis, is the result of pathogenic microorganisms entering the human body. To reduce the risk of infection, it is enough to follow a number of preventive measures:
- carefully observe personal hygiene - wash your hands after each contact with animals or land work;
- do not try raw meat, eggs;
- do not eat fruits and vegetables without first scalding them with boiling water;
- visit medical institutions where all instruments are sterilized.
Particular attention should be paid to the prevention of toxoplasmosis by women at the stage of planning pregnancy - to be tested in advance for the presence of toxoplasma microorganisms in the body, and at the entire stage of the baby’s intrauterine development to avoid situations where the infection can enter the body. Toxoplasmosis can be completely defeated if it is identified and treated in a timely manner.