Rathke's pouch cyst is a benign formation located inside the sella turcica of the skull base. They are epithelial-lined intrasellar cysts that are thought to develop from residual structures of Rathke's pouch. They usually appear as round, ovoid or dumbbell-shaped formations. They are common, affecting 13-33% of people, and sometimes cause compression of underlying structures, leading to symptoms such as headaches, visual disturbances, or pituitary hormone deficiency.
Studies have shown that cysts identified using radiation methods do not change over time or slightly decrease in size; this suggests that in the absence of compression symptoms, a conservative treatment approach is preferable.
Imaging has improved significantly with the introduction of computed tomography (CT) and magnetic resonance imaging (MRI) into clinical practice.
Get an MRI of the pituitary gland in St. Petersburg
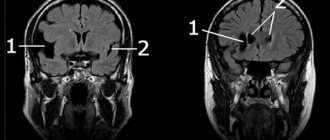
In the images below you can see how a Rathke's cyst looks in the picture.
MRI: Rathke's pouch cyst. A precontrast T1-weighted sagittal image shows a well-defined mass in the sella region extending into the suprasellar cistern. There is a homogeneously high signal intensity in the formation compared to the brain parenchyma.
T2-weighted axial image (same patient as previous image).
T2-weighted axial image: cortical isointense mass (same patient as in previous image).
Why does a Rathke's pouch cyst form?
As established by Voelker et al., according to the most generally accepted theory of origin, these formations develop from the true residual structures of Rathke's pouch that existed in the prenatal period.
Rathke's pouch appears approximately on the 24th day of embryonic development in the form of a dorsal diverticulum of the oral fossa; this formation is lined with epithelial cells of ectodermal origin. Around the same time, the pituitary funnel is formed in the form of an outgrowth of the neuroepithelium from the diencephalon. By the fifth week it grows to the funnel and becomes obliterated at the buccal-pharyngeal membrane. During the sixth week it separates from the oral epithelium. Then the distal part of the pituitary gland develops from its anterior wall. The posterior wall does not proliferate and remains in the form of a poorly visible intermediate part of the pituitary gland.
The residual lumen of the pocket is reduced to a narrow gap, which, in most cases, disappears. It is believed that persistence and widening of this fissure leads to the development of a Rathke cyst.
Diagram of the development of a cyst from Rathke's embryonic pouch.
Some authors adhere to other theories regarding the formation of these cysts: in particular, according to some theories, the source of development is the neuroepithelium or endoderm, or their development is assumed to be through metaplasia of the cells of the anterior pituitary gland.
Anatomy
During pathological examination, the size of the cysts varies from 2 to 40 mm. Its capsule is often thin and can be transparent, bluish, gray, white, yellow, pink, brown or greenish. The cystic fluid inside is usually thick or jelly-like (colloidal), but can also be watery, serous, or similar in consistency to motor oil. Most often the liquid is yellow, but whitish, clear, gray or greenish contents are sometimes described.
On histologic examination, cysts typically consist of vascularized connective tissue stroma and three types of epithelial cells: ciliated epithelium, nonciliated epithelium, and mucus-secreting cells. Non-ciliated epithelium is represented by a single layer of flat cells or in the form of several rows of columnar epithelium. Fager and Carter concluded that the presence of ciliated epithelium and mucus-secreting cells in the pituitary tissue is pathognomonic for this type of cyst.
In a retrospective analysis, Shin et al found that all those examined were intrasellar in origin at their original location. Due to their cystic nature, most of those studied in this work penetrated the suprasellar cistern through a gap in the diaphragm of the sella turcica. According to Voelker, based on the results of a retrospective analysis of 155 symptomatic clinical cases, cysts were characterized by an intrasellar and suprasellar location in 71% of patients. The area of the sella turcica was expanded in 80%.
Symptoms
In 80% of cases, there are no symptoms and the pathology is discovered accidentally during a CT or MRI. The vast majority of cysts are less than 2 cm in diameter. They are rare but may enlarge and cause compression of the pituitary gland, pituitary shaft, optic chiasm, or hypothalamus.
Symptomatically, they are very different in clinical manifestations. In a symptom study of 11 by Rao et al, 8 patients developed visual symptoms. In another study by Eguchi et al, visual signs were present in 47% of patients. These included decreased visual acuity, optic atrophy, visual field impairment, and chiasmal syndrome. The Eguchi study included 19 patients, 4 of whom had diabetes insipidus, 3 of whom had amenorrhea and/or galactorrhea, and 2 of whom had panhypopituitarism. During systematic endocrinological examination, pituitary dysfunction of varying degrees was observed. Other disorders included headaches and, less commonly, epilepsy.
In a study by Voelker et al, the most common finding was hypofunction of the pituitary gland with multiple endocrinopathies. In younger patients, aged 4 to 22 years, signs of hypopituitarism were observed from an early age and were accompanied by developmental delay. The second most common symptom was visual impairment, which included visual field impairment due to compression of the optic chiasm. Another common symptom was headache, frontal in 57% of cases. Shin et al also described impotence or decreased libido as the most common endocrinological pathology in men; Women most often had hyperprolactinemia. In addition to the symptoms described above, endocrinological symptoms develop secondary to pituitary adenoma. Rare or unusual findings associated with the study included pituitary apoplexy, hypophysitis, giant cysts, extensive frontal extension and unusual cyst shapes, aseptic meningitis, intracystic abscess, sphenoiditis, and empty sella syndrome.
Possible consequences and complications
Failure to treat a cyst on the pituitary gland of the brain can lead to it becoming malignant. Another rare, but with serious consequences, danger is the rupture of the walls of the cyst, penetration of fluid into the pituitary gland, and the development of acute sepsis.
In women, cysts prevent pregnancy.
The growth and development of education causes changes in hormonal balance and disrupts the functioning of many organ systems: genitourinary, nervous, endocrine. It is dangerous due to possible loss of vision. In women, cysts in the pituitary gland and the changes in hormonal balance it causes prevent pregnancy.
A cystic tumor of the pituitary gland is most often discovered by chance while investigating the causes and symptoms of other pathologies. For a long time it may not manifest itself in any way. Over time, vision and the nervous system begin to suffer, and sexual desire disappears. Medicinal, surgical methods, and traditional medicine are used for treatment.
Diagnostic methods
The method of choice for diagnosis is MRI of the chiasmatic-sellar region (pituitary gland). Thin sections should be obtained in the sagittal and coronal planes through the sella turcica. The study must be accompanied by contrast enhancement. CT scans may also be helpful in their evaluation. CT findings are particularly useful in diagnosing associated bone changes and calcification deposits.
Limitations of Methods
MRI is superior to CT in the quality of visualization and assessment of the size of the Rathke cyst. Sagittal and coronal MRI images provide reliable information about the relative position of the formation and the optic nerves, optic chiasm and hypothalamus. MRI in the coronal projection also allows us to identify the lateral spread of the cyst beyond the sella turcica and evaluate its location relative to the internal carotid arteries and cavernous sinuses. The Magnetic Resonance Imaging method is superior to CT in terms of multiplanar imaging capabilities and contrast resolution.
The advantage of CT is better display of small calcifications. This advantage is significant because the presence of calcifications may indicate an alternative diagnosis, such as craniopharyngioma, although small calcifications are sometimes found in this disease. CT is also superior to MRI in assessing associated bone remodeling.
What is important to know
It is important not to confuse Rathke with cystic pituitary adenoma. In the case of adenoma, complaints include symptoms of hormonal disorders, visual disturbances and headaches. Often the diagnosis of adenoma is made when the patient has Rathke, and vice versa. To reliably distinguish between these two conditions, expert MRI interpretation by an experienced neuroradiologist can be useful. A second opinion helps make an accurate diagnosis.
Treatment
The choice of treatment method depends on the type of cyst, its size, and the patient’s condition:
- Therapeutic. It is prescribed for damage to the adenohypophysis, which produces 95% of all hormones in the human body. To reduce the size of the tumor and hormone replacement, medications are prescribed.
- Surgical. Surgery to remove the cyst is indicated if conservative therapy does not produce positive results. The procedure is carried out under general anesthesia for several hours, after which the patient requires long-term rehabilitation.
- Homeopathic. It is selected individually and has a complex and lengthy dosage regimen. This technique helps stop the growth of formation, but is not able to relieve complications.
- Ethnoscience. Herbal decoctions and tinctures are used to improve metabolism when the condition is stable and there are no contraindications.
- Radiation therapy. It is performed extremely rarely for those patients who have contraindications to surgery: age, heart failure, asthma, and also when the cyst has degenerated into a malignant tumor. But this method is ineffective.
Small cysts are subject to watchful waiting. Regular examination of the patient and taking hormonal drugs in 20% of cases stabilize his condition for the rest of his life.
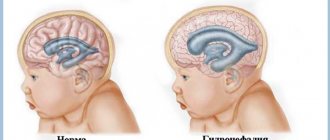
Cystic formation of the pituitary gland in newborns is subject to long-term observation. A small benign tumor often resolves on its own within the first year of life. Surgery is performed only for large tumors using bypass surgery and endoscopic procedures.
It is necessary to treat a tumor in cases where it tends to grow, causing neurological and systemic disorders.
X-ray of the sella turcica
Pocket cysts do not usually cause enlargement of the sella turcica on plain cranial x-rays. In patients with symptomatic cysts, plain x-rays usually show an unusual configuration of the sella turcica, ranging from mild asymmetry of the sella floor to massive bony erosions. Some patients have intra- or suprasellar calcifications.
The reliability of diagnostic data obtained from standard radiography is quite low. The detected changes are nonspecific: they may correspond to other frequently occurring changes in the area of the sella turcica, for example, anomalies in the configuration of the sella turcica or a pituitary adenoma.
CT scan for Rathke cyst
On CT, the cyst usually appears as a well-circumscribed hypodense sella turcica, sometimes extending into the suprasellar space. Due to their different contents, they can be isodense or hyperdense relative to the brain parenchyma.
They are usually characterized by a thin wall that can accumulate contrast. Significant differences in the contrast enhancement of different cysts on CT images may reflect squamous metaplasia of the wall or peripheral displacement of pituitary tissue in the form of a rim. Extravasation of cyst contents can cause inflammation of the underlying structures, which leads to the accumulation of contrast.
Calcifications are rare. Complex cysts may have internal septations. Large ones can cause restructuring of bone tissue, expansion of the sella turcica, and osteoporosis of its back.
CT images are not enough to confirm the diagnosis, since the data obtained do not allow us to clearly exclude other pathology. Simple cysts may be indistinguishable from arachnoid or epidermoid cysts. More complex ones can be difficult to distinguish from craniopharyngioma or pituitary adenoma. Therefore, the diagnosis must be made based on a combination of clinical, biochemical, pathological and radiological data.
Treatment of pituitary cysts “the old fashioned way”
In order to improve the general well-being of the patient in the absence of exacerbation of the disease, they resort to treatment with folk remedies. Treatment methods using herbal decoctions and tinctures have found very widespread use among people.
Bedbug has established itself as an ideal assistant in the fight against cystic formations, in particular in the brain. It is enough to add 10 drops to a glass of water and a 10% alcohol solution of bedbugs will gradually reduce the cyst, and the disease will recede.
Hemlock. Traditional medicine advises using this remedy with extreme caution. Oil solutions of this product are very toxic and are instilled into the nose, which has an additional effect on the entire body.
In order to improve metabolism, traditional medicine recommends taking decoctions of string and oregano. Additionally, pharmacies sell herbal teas that have antitumor effects. But in order to avoid complications, it should be remembered that any treatment has its contraindications.
Even before starting herbal therapy, you should get qualified advice from your doctor. Treatment of a pituitary cyst involves a long course of the disease, most often hidden, and an equally long recovery period after the operation. But before you go to see an endocrinologist, you should know that if the diagnosis is confirmed, then the patient’s card will record it as “adenoma” - the scientific name of the cyst.
MRI for Rathke's pouch cyst
The MR picture can be very different (see images below). Although no specific MRI features have been identified, most can be divided into the following two groups:
1) With low signal intensity on T1-weighted images and high signal intensity on T2-weighted images
2) With high signal intensity on T1-weighted images and variable signal intensity on T2-weighted images
T1-weighted sagittal image obtained before contrast enhancement shows a well-defined cyst in the area of the sella turcica, isointense to the cerebrospinal fluid. There is a normal high signal intensity of the posterior lobe of the pituitary gland from behind.
On a T1-weighted coronal image, it is visible just under a centimeter in size at the central part of the sella turcica. Slightly hyperintense compared to cerebrospinal fluid.
On this T2-weighted image, it is isointense to the cerebrospinal fluid.
The large one is hyperintense compared to the cerebrospinal fluid on axial proton-weighted image. There is an expansion of the sella turcica with a lateral deviation of the slightly obscured but patent cavernous part of the internal carotid artery.
Get an MRI of the pituitary gland in St. Petersburg
The contents of the first group resemble cerebrospinal fluid (CSF). In the second group, increased signal on T1-weighted images is associated with high levels of mucopolysaccharides, which is believed to be a consequence of an increase in the number of mucin-secreting cells in the wall, as well as increased activity of these cells.
Rare cases of high signal intensity on T1-weighted images and low intensity on T2-weighted images are associated with a combination of various factors, including the presence of mucopolysaccharides, old hemorrhage, significant cholesterol or cellular debris from the cyst wall. They are almost always homogeneous in signal intensity, while other pathological formations, such as craniopharyngiomas and hemorrhagic adenomas, are more often characterized by heterogeneity in signal intensity.
They have a thin wall that can be contrasted when injecting gadolinium-based contrast agents. Various patterns of gadolinium enhancement may reflect squamous metaplasia of the wall or pituitary tissue displaced to the periphery in the form of a rim.
Data on the relationship between signal intensity and its clinical manifestations are very rare. In 1997, Takeichi and colleagues studied 78 patients, including 9 of their own patients, and reported that cerebrospinal fluid signal intensity was slow growing, large in size, and often caused visual symptoms. Symptomatic ones with different signal intensities were smaller in size.
The DWI-SSFSE mode with ICD values can also be used in the differential diagnosis of craniopharyngiomas and hemorrhagic pituitary adenomas.
How reliable is MRI?
There is not a single characteristic MRI sign that could be used for a reliable differential diagnosis of Rathke's pouch cysts and other cystic formations of the sellar or suprasellar region. Simple cysts may be indistinguishable from arachnoid or epidermoid cysts. More complex ones may be difficult to distinguish from craniopharyngiomas or pituitary adenomas.
Cystic pituitary adenomas may resemble the former in the absence of a solid contrast-enhancing component on MRI. Features such as the presence of a fluid-liquid level, a hypointense rim on T2-weighted images, internal septa, and a location lateral to the midline are more often consistent with pituitary adenomas, while the presence of an intracystic nodule may be more often associated with the research topic.
Due to the significant variability in CT and MRI findings, preoperative diagnosis requires a combination of clinical, biochemical, and radiographic findings. Differential diagnosis is very important because the treatment and surgical approach differ significantly from those for other possible pathologies. If you are in doubt about the diagnosis, you can get a second opinion with an MRI of the pituitary gland.
Causes and symptoms of different types of adenomas
Pituitary adenoma is not classified as a hereditary disease and is not explained by genetic predisposition - this type of tumor develops spontaneously. At the moment, the exact reasons for the development of pituitary adenoma are not clear. However, there are predisposing factors for the appearance of a tumor:
- traumatic brain injuries;
- infectious diseases of the brain;
- uncontrolled use of hormones and hormonal drugs;
- exposure during fetal development.
But these same reasons can also influence the development of another type of tumor, for example, cysts of the intermediate velum of the brain. The symptoms of adenoma development are also very ramified. Depending on the type of tumor, symptoms are determined.
The presence of a hormonally active adenoma is indicated by:
For prolactinoma:
- cessation of menstruation;
- reduction in breast milk production during lactation;
- frigidity;
- decreased testosterone levels;
- weakening libido.
For a tumor that produces growth hormone:
- acromegaly (adult);
- gigantism (children);
- disproportionate development of hands and feet;
- diabetes;
- other visible changes in proportions.
For a tumor that produces adrenocorticotropic hormone:
- causeless weight gain;
- hematomas;
- hair growth on the face and body;
- diabetes;
- muscle weakness.
For thyrotropinoma:
- sudden weight loss;
- increased sweating;
- arrhythmia;
- hand tremors;
- insomnia.
If a microadenoma develops practically asymptomatically, then a macroadenoma, especially at the stage of active growth, is detected due to the following signs:
- sharp deterioration in vision (adenoma puts pressure on the optic nerve);
- deterioration of peripheral vision;
- decreased visual acuity;
- doubling in the eyes;
- disturbance of color perception (dimming of the brightness of shades).
Additionally observed:
- chronic headache (due to pressure on brain tissue);
- general signs of pituitary failure.
In addition, it is the development of macroadenoma that leads to complications such as:
- hydrocephalus;
- critical increase in intracranial pressure;
- blindness;
- hemorrhages into the cyst tissue (adenoma);
- cystic adenoma.