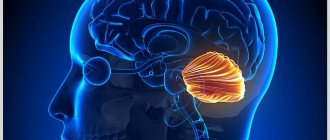
The amygdala is a specific part of the brain that visually resembles the shape of a regular amygdala. Its dislocation is located deep in the temporal lobe of the brain; in Latin, “lobe” is called Lobus temporalis. Each hemisphere of the brain has its own amygdala. The importance of these tonsils is difficult to overestimate, because they are involved in the formation of emotions and are an integral element of the limbic structure.
In humans and many species of animals, it is this part of the brain that is responsible for the production of positive and negative emotions - pleasure, fear, anger and others. The size of the cerebellar amygdala has a direct relationship with respect to aggressive actions. This part of the brain is sexually dimorphic. For example, if a man has been castrated, the cerebellar tonsils decrease in size by 30%.
Doctors have proven that many mental illnesses are associated precisely with disruption of the normal function of the cerebellar tonsils. In particular, the following diseases:
- increased anxiety;
- autism;
- schizophrenia;
- bipolar disorder;
- various phobias.
Reasons for appearance
Cerebellar dystopia, as a rule, is a congenital pathology. It occurs when an organ is displaced during the embryonic period. It occurs secondary only when frequent punctures are performed or with lumbar injuries. No other causes of this disease have been identified.
The tonsils of the cerebellum are very similar to those found in the larynx. In the normal position, they are located above the BZO of the skull. And deviations in their development and position can lead to not only dystopia. The most common occurrence is prolapse of the cerebellar tonsils below the level of the skull.
Until now, Chiari disease is a pathology, the causes of which neurologists have not come to a common opinion. Some are of the opinion that this anomaly occurs when the size of the fossa behind the cranial outlet to the spinal canal decreases. This often leads to such consequences during the growth of tissues that are located in the box. They exit into the occipital exit canal. Other experts believe that the disease begins to develop due to an increase in the volume of brain tissue in the head. In this case, the brain begins to push the cerebellum and its tonsils through the posterior cranial fossa into the occipital cranial foramen.
Arnold-Chiari syndrome
Low location of the cerebellar tonsils is a congenital condition; the brain structures of the head descend into the foramen magnum. The process usually involves the medulla oblongata and cerebellum. Arnold Chiari disease is detected in some people completely by accident, for example, during an examination due to another pathology. At the first stage, the course of the disease is mild and often unnoticeable. In this situation, Arnold-Chiari malformation does not pose a threat to the health of the body.
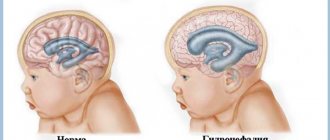
The pathology can be practically asymptomatic, but often this disease is combined with syringomyelia (the name of a disease of the gray matter of the spinal cord). Lack of treatment can provoke hydrocephalus (accumulation of fluid in the skull), cerebral infarction and other dangerous pathologies, and cases of disability have been reported. The defect can be identified immediately after birth or after 20-30 years. Chiari malformation can be one of 4 types.
Arnold Chiari malformation of the 1st degree - the structures of the posterior part are often infringed due to exit through the foramen magnum. This position leads to the accumulation of cerebrospinal fluid. Chiari syndrome of the first degree is a displacement of the cerebellar tonsils, they are located below the foramen magnum. Arnold-Chiari malformation is often detected in adolescence.
Arnold-Chiari syndrome stage 2
An anomaly of the second degree has more pronounced structural changes. The cerebellum, which is located in the foramen magnum, is involved in the process. Screening ultrasounds of the fetus can show some defects in the structure of the spine and spinal cord. In most cases, the prognosis for the baby’s life is favorable, but clinical signs of pathology will be present. This indicates the need for dynamic monitoring of the patient.
In this case, almost all formations of the cranial fossa are located below the foramen magnum (pons, 4th ventricle, medulla oblongata, cerebellum). Often they are found in a cervico-occipital cerebral hernia (when there is a defect in the spinal canal, in which the vertebral arches are not closed, the contents of the dural sac, which includes all the membranes and the spinal cord). With this type of anomaly, the foramen magnum has an increased diameter.
This is the most severe version of the disease. With this variant of Arnold Chiari syndrome, cerebellar hypoplasia and underdevelopment are observed. Often combined with congenital posterior fossa cysts, congenital cysts and hydrocephalus. When type 4 is diagnosed, the prognosis is unfavorable; in most cases, the disease ends in the death of the patient.
Types of anomalies
There are such types of abnormal deviations as dystopia and Chiari malformation.
In turn, Chiari disease is divided into four different types:
- Type I is characterized by the location of the tonsils below the level of the foramen magnum. This pathology is usually detected in adolescents and adults. It is often accompanied by an accumulation of spinal cerebrospinal fluid in the central canal, where the patient’s spinal cord is located.
- Type II is characterized by manifestation immediately after birth. In addition, in addition to the tonsils, in the second type of pathology, the cerebellar vermis with part of the medulla oblongata and the ventricle emerge into the foramen of the occipital part. The second type of anomaly is much more often accompanied by hydromyelia than with the pathology described in the first case. In most cases, this pathological deviation is associated with congenital hernias formed in various parts of the spinal cord.
- Type III is distinguished by not only the tonsils descending through the hole, but also the cerebellum along with the tissues of the medulla oblongata. They are located in the cervical and occipital regions.
- Type IV is an underdevelopment of cerebellar tissue. This pathology is not accompanied by their displacement in the caudal direction. But the anomaly is most often accompanied by a congenital cyst located in the cranial fossa and hydrocephalus.
Types II and III often appear in combination with symptoms of nervous system dysplasia, for example, heterotopia of the cerebral cortex tissue, foramen cysts, etc.
Symptoms
The most common among the anomalies is the pathology of the first type. With it, the manifestation of liquor-hypertension syndrome is often possible, as well as cerebello-bulbar and syringomyelic phenomena, disturbances in the functioning of nerve endings inside the skull.
Liquor-hypertensive syndrome is pain in the back of the head and neck muscles, which intensifies during sneezing, coughing or straining the neck muscle tissue. Often the pain is accompanied by vomiting that is not associated with eating. Many symptoms of the pathology appear depending on the position of the cerebellar tonsils relative to the opening that is located in the occipital fossa of the skull. Also observed:
- increased tone of the cervical muscles;
- speech dysfunction;
- deterioration of the organs of vision and hearing;
- deviations when swallowing;
- frequent dizziness accompanied by noise in the head;
- a feeling of rotation of the environment;
- brief fainting;
- pressure changes during sudden movements;
- tongue atrophy;
- hoarseness of voice;
- breathing problems and sensitivity of different parts of the body;
- attacks of numbness;
- disorders in the pelvic organs;
- weakening of the muscles of the limbs.
Anomalies of types II and III have similar symptoms, noticeable from the first moments after the birth of the baby. The second type is accompanied by noisy breathing, as well as unexpected attacks of respiratory arrest, neuroparesis of laryngeal tissues. Deviations in the swallowing process are also observed.
Signs of dystopia are rarely obvious. But neurological manifestations are still possible:
- attacks of “shooting” pain in the neck muscles with increased tension or coughing;
- frequent pain in the head area;
- attacks of dizziness and fainting.
If the prolapse of the tonsils is severe, sometimes there is a widening of the canal connecting the brain and spinal cord, and cavities form around the canal.
Diagnostic methods
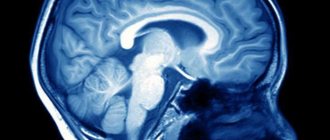
The main modern method for diagnosing dystopia is MRI. In this case, neither CT nor X-ray studies provide a complete picture of the pathology.
No standard methods such as EEG, EchoEG or REG are suitable for diagnosing Chiari syndrome, because they do not allow an accurate diagnosis. An examination by a neurologist will also not determine the anomaly. All these methods can only show suspicion of increased pressure inside the skull. X-rays of the skull should also not be done, since they only show abnormalities of bone tissue that may accompany pathology. Therefore, before the introduction of tomography into diagnostic practice, diagnosing this disease was problematic. Modern diagnostic methods make it possible to accurately determine the pathology.
In the case of high-quality visualization of the bone tissue of the vertebral junction, methods such as MSCT or CT do not provide a sufficiently accurate picture. The only reliable way to diagnose Chiari malformation today is MRI.
Since research with this method requires the patient to remain immobile, young children are put into artificial sleep with the help of medications. An MRI of the spinal cord is also performed. It is aimed at diagnosing any abnormal abnormalities in the functioning of the nervous system.
Treatment
Conservative treatment methods are possible only for very minor deviations. It all depends on what the patient’s condition is at the time of going to the doctor. In this case, treatment is aimed at relieving painful symptoms with non-steroidal medications or muscle relaxants. Correction of the regime is also necessary.
The only effective treatment for large deviations is surgery, which consists of widening the cranial fossa and plastic surgery of the dura mater tissue.
Indications for surgical treatment are:
- debilitating headaches that cannot be relieved by medications.
- an increase in brain manifestations leading to disability.
If the abnormal deviation occurs without any noticeable signs, no treatment is required. In cases of pain in the neck and back of the head, conservative therapy is carried out, which uses analgesics and aseptic drugs, as well as muscle relaxants.
When Chiari malformation is accompanied by neurological dysfunction or when a conservative course of therapy does not produce results, surgery is prescribed.
Often, during treatment courses for Chiari syndrome, the method of craniovertebral decompression is used. The operation involves widening the opening of the occipital part by removing part of the bone tissue, cutting off the cerebellar tonsils and parts of two vertebrae of the neck. Thanks to this, the turnover of cerebrospinal fluid in the brain tissue is normalized as a result of a patch made from an allograft or artificial material. Chiari syndrome is sometimes treated with a shunt, which allows cerebrospinal fluid to drain from the central canal. Through surgery, cerebrospinal fluid can be drained into the vessels of the chest or peritoneum.
Forecast
Chiari malformation type 1 can be asymptomatic throughout life. And the third type of pathology almost always leads to death if timely treatment is not carried out. In the event of the appearance of neurological signs of the disease of the first or last type, timely surgical treatment is very important, because the resulting lack of neurological functions will be poorly restored, even if the manipulations are successfully performed. According to various sources, the effectiveness of surgery is observed in approximately half of the episodes.
Pediatrician Anna Kolinko about the pathology of brain development, which can occur in 30% of the population
Chronic fatigue syndrome, dizziness and neck pain can be a consequence of Arnold-Chiari malformation (anomaly). After the widespread use of MRI, it became clear that the disease occurs in 14–30% of the population
Arnold-Chiari malformation (MAC) is a pathology of the development of the rhombencephalon: the medulla oblongata and hindbrain, the latter including the pons and cerebellum. With MAC, the posterior cranial fossa does not correspond to the brain structures located in this area: the cerebellum and medulla oblongata, due to their small size, descend below the foramen magnum, which leads to their pinching and disruption of cerebrospinal fluid dynamics. MAC belongs to the group of cranio-vertebral (craniovertebral) malformations.
In the pre-MRI era, the incidence of MAC was estimated at 3.3 to 8.2 observations per 100,000 population, and in newborns - 1 in 4-6 thousand. Today it is clear that the prevalence of Arnold-Chiari syndrome is much greater. Due to the asymptomatic course and as a result of taking into account different types of MAC, the numbers vary greatly - from 14 to 30%.
What functions do the tonsils perform?
Thanks to the cerebellar bodies, a person is able to quickly and permanently remember emotional reactions to various kinds of events. And since the amygdala is part of the limbic structure, a person has the ability to learn unconsciously. This feature distinguishes some types of animals.
The brain has a special structure, for this reason, incidents that are significant in terms of survival are recorded with the help of strong emotions. After all, the main job of the brain is to care about survival. Accordingly, such an emotion activates the internal mechanism necessary for a person not to forget this event. This information is located in long-term memory.
Unconscious learning can control the formation of conditioned reflexes. This learning occurs automatically and on an unconscious level. Because human reflexes are located in parts of the brain that are independent of thinking, they are difficult to rationalize. In carrying out its duties, the amygdala interacts with the hippocampus and basal ganglia. As a result of this interaction, incoming data is assimilated at a higher level.
Dystopia of the cerebellar tonsils is a specific descent of the cerebellar amygdala into the large foramen magnum. This pathology can be called Chiari malformation; it occurs when there is a caudal dislocation of the amygdala on the right or left side of the brain. The disease is characterized by decreased position of the amygdala.
Such standing of the tonsils in no way affects the patient’s life and does not cause concern. This disease is found extremely rarely in children; adults between 30 and 40 years of age are more susceptible to it. It is diagnosed by chance, during routine examinations or treatment of other problems.
Types of Malformations
Type 1 - descent of the cerebellar tonsils into the spinal canal below the level of the foramen magnum with the absence of spina bifida. In 15–20% of patients, this type is combined with hydrocephalus, and in 50% of patients with syringomyelia, a disease in which cavities form in the spinal cord and medulla oblongata. In 1991, it was proposed to subdivide type 1 Arnold-Chiari malformations into type A, with syringomyelia, and type B, without syringomyelia.
Encephalomeningocele is a congenital hernia of the brain and its membranes containing cerebrospinal fluid.
Spinal dysraphism is a developmental defect consisting in the absence of fusion along the midline of paired anlages of skin, muscles, vertebrae, and spinal cord
Type 2 - prolapse of the lower parts of the cerebellar vermis, medulla oblongata and fourth ventricle. A distinctive feature of this type is the combination with spina bifida in the lumbar region, progressive hydrocephalus, and often stenosis of the cerebral aqueduct. Among children with meningomyelocele, up to 90% of cases are accompanied by grade 2 Arnold-Chiari malformation.
Grades 0, 1 and 2 of Arnold-Chiari syndrome are the most common in the population. Types III and IV are usually incompatible with life.
Accompanying illnesses
Syringomyelia of the cervical spine occurs in ~35% (varies from 20 to 56%), hydrocephalus in 30% [1,3] of cases, in both cases these changes are considered to develop as a result of disturbances in the fluid dynamics of the central canal and around the spinal cord. B ~ 35% (23-45%) skeletal anomalies are detected [1, 3]:
- platybasia/basilar impression
- atlanto-occipital assimilation
- Sprengel deformity
- Klippel-Feil syndrome
Symptoms
Neurological symptoms of types 0 and 1 Arnold-Chiari malformation most often begin to bother people at the age of 20–40 years. The degree of dislocation of the cerebellar tonsils can increase under the influence of unfavorable factors. The most common complaints with MAC type 0 are headache, predominantly of the cervical-occipital localization, as well as pain in the neck. Arnold-Chiari malformation type 1 in adults is more often manifested by complaints of nystagmus, dysarthria, ataxia, intention tremor (tremor during voluntary movements), headache, dizziness, sensory disturbances, paresis, dysfunction of the pelvic organs, disturbances in the frequency and rhythm of the pulse, breathing rhythm , lability of blood pressure, symptoms of damage to the caudal group of cranial nerves (IX, X, XI, XII pairs) - impaired facial sensitivity and bulbar disorders (swallowing and speech disorders).
X-ray features
Pathology is detected by measuring the maximum distance by which the tonsils protrude below the plane of the foramen magnum (the conventional line between the ophisthion and basion), the values used for diagnosis differ among different authors [2]:
- above the foramen magnum: normal
- from 3 to 6 mm: uncertain data, must be compared with symptoms, the presence of syringomyelia, etc.
- {amp}gt; 6 mm: Arnold Chiari malformation 1
Some authors use a simpler gradation [1]:
- above the foramen magnum: normal
- {amp}gt; 5 mm: Arnold Chiari malformation 1
The position of the cerebellar tonsils changes with age. In newborns, the tonsils are located just below the foramen magnum and descend lower as the child grows, reaching their lowest point at the age of 5–15 years. Subsequently, they rise to the level of the foramen magnum [3]. Thus, a decrease in tonsils of 5 mm in a child will most likely be normal, and in adulthood these changes should be considered with suspicion [3].