© Author: Olga Khrabrova, edited by first category doctor Z. Nelli Vladimirovna, especially for SosudInfo.ru (about the authors)
Modern medicine contains a huge list of diseases. Many of them have such similar symptoms that it is difficult for a layman to figure out what the true cause of his illness is. And this is correct: everyone should know well only what he was taught. But there are several factors that push a person to independently search for the cause of his health problems. Firstly, most people today are well educated and know how to work with information, and secondly, many have doubts that the doctor’s diagnosis was correct.
In the frantic rhythm of modern life, man, with the development of the benefits of civilization, has become able to move in space faster, but to move much less. Physical inactivity is a provoking factor against which obesity, problems with the musculoskeletal system, heart and blood vessels, respiratory and digestive disorders develop. An inactive lifestyle is the main cause of such a disease as venous stagnation. Let us consider in detail its symptoms and forms of manifestation.
Etiology
The primary cause of venous hyperemia is difficulty in the outflow of blood into tissues or organs, which leads to increased pressure. There will be slower blood flow in the capillaries, causing them to expand to the size of venules.
In the area where hyperemia is localized, due to slow blood flow, there is an intense release of oxygen to the tissues and a large intake of carbon dioxide into the blood, which leads to hypoxemia and hypercapnia. The organ or tissue takes on a blue tint - cyanosis. In this place, the body temperature decreases, swelling occurs due to the large accumulation of water. The permeability of the walls of blood vessels increases.
Causes of venous stasis in the pelvic organs or lower extremities:
- sedentary lifestyle;
- use of hormonal medications;
- increase in circulating blood volumes;
- excess body weight;
- chronic inflammatory processes;
- tumors of the uterus or ovaries;
- pregnancy or difficult childbirth with complications;
- excessive physical activity.
Venous congestion in the head refers to passive hyperemia and can appear due to intracranial or extracranial disorders:
- injuries;
- tumors in the cervical region;
- lung pathologies;
- congenital abnormalities in blood vessels;
- vein blockage
Obstructed blood flow can provoke venous congestion in the lungs, causing tissue compaction and a change in the color of the organ; over time, the resistance of the capillaries decreases and sclerosis forms.
The causes of stenosis in the heart are previous infectious diseases, inflammatory processes in the heart muscle, impaired blood circulation and vascular patency. In childhood, the disease is diagnosed due to heart disease or autoimmune processes.
Causes of venous stagnation
Fursenko I.A. cardiologist
Research Institute of Experimental and Clinical Medicine, Novosibirsk
If you ask a random person what he associates the following picture with:
Most likely, you will get the correct answer: “Blood stagnates in the vessels.”
The veins that return blood from the organs back to the heart resemble a river in the spring flood. Any obstacle—an increase in pressure, stagnation “upstream”—can cause a wide flood of such a “river.” The walls of the veins are thin, pliable, easily stretched, forming “in which blood cells and various protein “garbage” accumulate, forming blockages and congestion, which can further aggravate the situation. Metabolism and oxygen transport are disrupted, and trophic ulcers occur. And really bad things can happen if a blood clot breaks off and travels to the heart and lungs.
How can we help?
Option 1 - strengthen the banks
Option 2 - Clear congestion
Actually, until recently, there were means only for option 1 - venotonics (medicines) and compression garments.
Now in the arsenal of doctors there is TROMBOVAZIM®, a complex-action drug prescribed specifically for chronic venous insufficiency (CVI)[2]. The main thing it does is influence the fibrin framework of the thrombus, providing a thrombolytic effect [1, 2], and clears the congestion. Normal, calm blood flow is restored, swelling is reduced, and trophic ulcers are healed [3]. The drug TROMBOVAZIM® acts on blood clots in such a way that they slowly dissolve in the blood stream, gradually melting like ice.
TROMBOVAZIM® is an enzyme preparation created using the unique AXIS technology, in collaboration with doctors and physicists. The uniqueness of the technology allows you to work exactly in the right place without affecting the blood coagulation system as a whole. And most importantly, TROMBOVAZIM® has an oral dosage form - capsules for oral administration.
The very idea of creating and the first work on the synthesis of the thrombolytic drug TROMBOVAZIM® appeared in the Novosibirsk Akademgorodok. In the period 2002-2006, preclinical and clinical studies were conducted that confirmed the effectiveness and safety of the drug TROMBOVAZIM®, and in 2007 the first oral thrombolytic TROMBOVAZIM® in tablets was registered. In 2013, the team of authors was awarded the State Prize for its development and implementation.
Currently, TROMBOVAZIM® is available in all major cities of Russia.
Dear readers! Please write in the comments under the article what other topics related to edema and the treatment of thrombosis interest you.
There are contraindications. It is necessary to consult a specialist.
Products by topic:[product](Thrombovasim)
1. “ANGIOLOGY AND VASCULAR SURGERY” 2015 • VOLUME 21 • No. 1
EXPERIENCE OF CLINICAL USE OF THE NEW DRUG TROMBOVAZIM® IN VASCULAR SURGERY (Madonov P.G., Kinsht D.N., Ershov K.I., Shilova M.A., Solovyov O.N.)
2. Instructions for use of the medicinal product for medical use TROMBOVAZIM® capsules 400 IU, 600 IU, 800 IU.
3. Clinical study “Rokit-VN” according to protocol No. 03-04, 2005
as an advertisement
Classification
Hyperemia has several varieties:
- arterial (active);
- venous (passive);
- mixed.
The disease can be classified according to the location of hyperemia:
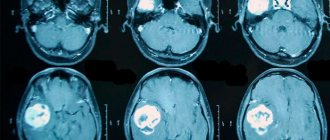
- Congestion of cerebral vessels occurs due to pathology inside or outside the skull; this is a secondary symptom. The chronic form provokes oxygen starvation of the brain with swelling and increased intracranial pressure. Without treatment, the functional features of the brain suffer.
- Pulmonary venous hyperemia provokes pulmonary edema. The tissue of the organ thickens and becomes brown in color (due to the accumulation of a special pigment). The disease is complicated by the development of sclerosis in the tissues.
- Stagnation in the pelvis. Occurs frequently and is passive in nature. The pathological process is observed in both women and men, which leads to painful sensations in the lower abdomen, provokes infertility and problems with the genital organs. In women, problems with blood flow cause premature labor, which causes the birth of an underdeveloped or stillborn baby.
- Hyperemia in the lower extremities. The pathological process develops slowly, forming vascular deformation and causing problems with blood flow.
- Venous congestion in the kidneys causes an increase in their size and hardening. The flow of blood into the organ is disrupted, resulting in renal spasm.
Venous congestion in the legs
The disease can be detected in the liver and upper extremities, in the intestines and ovary.
According to the degree of the disease, experts distinguish:
- Acute venous congestion provokes blockage of the veins, the patient’s condition is serious. Severe pain and swelling appear, the temperature of the skin at the site of the pathology drops sharply and becomes bluish in color, and spots with blisters may form on the skin due to hemorrhage. Sensitivity is greatly reduced, the patient is feverish, and the blood pressure is low. If you do not help a person in the near future, disorders in the body become irreversible.
- Chronic venous congestion is sluggish and is not detected at first. The patient's condition worsens gradually: heaviness, severe fatigue, soreness, and swelling appear. Other signs depend on the location of the process.
Any deviation from the norm requires an immediate response in order to prevent complications in time.
Treatment of cerebral venous outflow disorders
In a situation where a patient is diagnosed with a violation of venous outflow, he is prescribed venotonics and other vascular drugs. But this measure is temporary, as mentioned above. As soon as the medication is stopped, the complaints return. The answer to the question: “How can this be?” is very simple: “Because the cause of the disease has not been eliminated.”
In this situation, osteopathic treatment is, literally, salvation, because the doctor works with the root cause of the disease. First of all, the osteopath eliminates the disorders visible to him:
- normalizes muscle tone, because Hypertonicity can cause compression of the veins and disrupt the outflow.
- eliminates the slightest displacement of skull structures;
- restores the correct position of the vertebrae.
Most patients, after starting treatment, note increased strength, improved sleep and memory, and a feeling of lightness in the body. But there are situations when after the first session the condition may worsen. But, we hasten to reassure you, this is temporary. Let's explain why this happens. When any problem arises, our body tries to independently adapt to new circumstances, i.e. compensation processes are launched. If a person turns to an osteopath at the beginning of a problem, then most likely he will not experience any discomfort after the session, because The body has not yet had time to rebuild. If the problem has been developing for years, then there is a high probability that after the first visit to an osteopath the condition may worsen somewhat, because the body must get used to the “rearrangement”. Malaise, as a rule, lasts a couple of days, then the condition improves and the body heals itself.
Dear patients, remember that you do not have to endure and wait for the body to cope with the disease on its own. Take action and help your body. And there will be health and harmony in your life. It’s not for nothing that they say that in a healthy body there is a healthy mind
Symptoms
Hyperemia manifests itself symptomatically in different ways, it all depends on the form, degree and location of formation:
- In the pelvis in men and women, when the outflow of blood is disrupted, discomfort occurs in the lower abdomen, and pain intensifies during sexual intercourse. Bleeding may occur in the intestines with prolapse of hemorrhoids.
- Brain stasis leads to severe pain, dizziness, fainting, noise and buzzing in the ears. The patient's face swells and the mucous membrane of the throat turns pale.
- Hyperemia of the lungs causes shortness of breath, coughing, and bloody sputum production.
- Symptoms of stagnation in the legs: tissue temperature decreases, heaviness in the legs is felt, limbs swell, the skin turns blue. The sensitivity of the skin drops sharply, subcutaneous hemorrhages are observed, trophic ulcers appear, which become infected and suppurate.
- Venous congestion in the heart leads to swelling of the legs, pale skin, and brittle nail plates. Over time, the veins clearly protrude, and there is puffiness and pain in the chest area.
How does congestion manifest in the veins of the legs?
Varicose veins, known to everyone, are a clinical manifestation of blood stagnation in dilated veins that have lost their tone.
Symptoms of pathology:
- dull pain and heaviness in the muscles that develop in the evening;
- swelling on the feet and legs against the background of bluish skin of the fingers;
- chilly feet even in summer;
- manifestations on the skin in the form of a light mesh on the hips, under the knees, on the legs;
- disruption of tissue trophism in later stages (non-healing cracks in the skin of the feet, ulcers).
You can read about the treatment of varicose veins on our website in this article.
Inactive deep vein valves take part in the mechanism of venous stagnation of the legs
Diagnostics
Venous congestion in the head or other organs is diagnosed by studying the medical history, listening to complaints and conducting an external examination of the patient.
Depending on the symptoms and suspicions of the doctor, the patient is referred for additional procedures:
- ultrasonography;
- X-ray;
- Magnetic resonance imaging;
- CT scan;
- laparoscopy.
Diagnostic laparoscopy
After establishing the cause of venous stagnation and the severity of the condition, individual therapy is prescribed.
Pathogenesis and mechanism of development of pathology
The pathogenesis of venous hyperemia is due to the following factors:
- low arteriovenous pressure;
- venous blockage (thrombosis or embolism);
- decreased elasticity of venous walls;
- difficult movement of venous blood due to its thickening and increased viscosity;
- compression of veins by edema, tumor, etc.;
- impaired cardiac performance;
- decreased suction function of the chest due to accumulated blood or air in the pleural plane.
So, let us repeat that the mechanism of development of venous hyperemia is:
- compression of veins by external factors - tumor, scars, uterus during pregnancy, surgical ligation of blood vessels;
- compression of veins by edematous fluids;
- venous blockage by a thrombus.
Prolonged venous hyperemia can cause complete atrophy of the organ.
Treatment
Treatment of venous stagnation depends on the cause of the pathology. For mild cases of the disease, a set of therapeutic exercises, massages, and special diets are prescribed. The patient should get rid of bad habits to prevent vasospasm.
Drug treatment includes:
- taking venotonics, which reduce the permeability of vascular walls, remove inflammation, restore elasticity, improve blood circulation, and eliminate swelling;
- use of angioprotectors and antiplatelet agents.
For hyperemia in the kidneys, antibacterial drugs and painkillers are prescribed.
In addition to the basic treatment, the patient is provided with medical advice on proper nutrition, wearing comfortable underwear and shoes. Use a contrast shower and cream for varicose veins. In severe cases, surgical procedures are prescribed.
How to treat
If any symptoms appear, you need to go to the hospital. Which doctor should I see? Phlebologists, urologists and surgeons are involved in the diagnosis and treatment of such ailments.
After the examination, tests are prescribed, as well as instrumental examination - ultrasound, MRI, phlebography with a contrast agent.
Often, it may be necessary to undergo several studies to obtain a more reliable picture of the disease.
Sometimes it happens that the cause of the pathology is not related to neoplasms or other diseases, in which case preventive measures and treatment with medications that help improve blood supply are sufficient.
Options for other reasons:
- Hormone therapy, surgery - if the cause is tumors.
- Physical activity, antibacterial or antiviral therapy - if the cause is a sedentary lifestyle.
- Exercise therapy – due to physical inactivity or wearing clothes that cause discomfort.
- Treatment methods for venous stagnation in different organs depend on the location of the anomaly. Therapy includes several methods.
- Pelvic plethora. Mostly medications (drugs, suppositories) are used, but sometimes surgical intervention is still necessary.
- Congestion of the brain is eliminated by lowering pressure and reducing swelling. They use pills, injections, neck massage, and electrical stimulation.
- Pulmonary stasis is mostly treated with medication; in case of serious complications, surgery is performed. Disability may be assigned.
- Kidney hyperemia requires the prevention of infectious complications and pain relief. In this regard, it is imperative to take antibacterial drugs that have the ability to relieve pain. Blood flow is restored by surgery.
- Stasis of the lower extremities is treated with diuretics, venotonics, and ointments. When treating leg stasis, it is important to use compression stockings, or tights. A contrast shower and daily walking come to the rescue. To alleviate the condition, you can raise your legs.
The best prevention of venous blood stagnation is a healthy lifestyle. Namely: moderate, regular exercise, healthy eating, giving up bad habits.