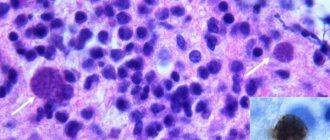
Demyelinating disease is a pathological process of destruction of the myelin sheath that affects neurons in the brain and spinal cord. At the same time, the conductivity of impulses in the nervous system deteriorates. The disease is characterized by the destruction of brain myelin. This dangerous condition affects the functioning of the entire body. The disease occurs with equal frequency in both adults and children. Modern medicine does not have the means to completely cure this disease. It can only be weakened and the flow slowed down.
Demyelination
Demyelinating brain disease according to ICD-10 has codes G35, G36 and G77. The process caused by damage to the nervous tissue negatively affects the functioning of the entire organism as a whole. Certain nerve endings are covered with a myelin sheath, which performs important functions in the body. For example, myelin ensures the rapid transmission of electrical impulses and, accordingly, if this process is disrupted, the entire system suffers. Myelin consists of lipids and protein compounds in a 70/30 ratio.
Expert opinion
Author: Daria Olegovna Gromova
Neurologist
The most common demyelinating brain disease is multiple sclerosis. Its symptoms are very diverse, so the patient rarely immediately comes to a neurologist. Decreased vision, numbness of the limbs, problems with motor skills - different doctors give different recommendations, although it is enough to simply send the patient for an MRI and laboratory tests that will confirm fears or rule out brain diseases.
Demyelinating disease is not only multiple sclerosis, it is also neuromyelitis optica and acute disseminated encephalomyelitis. These diseases have no cure, but their progression can be slowed down. In general, doctors give a favorable prognosis when treating these pathologies. The diagnosis of “multiple sclerosis” is now made more often, but the disease itself is milder than 30-40 years ago.
Thanks to modern methods of therapy and research, a benign course is observed in approximately half of the cases - patients fully retain their ability to work, start families, and give birth to children. There are some restrictions, for example, visiting baths and saunas, prolonged exposure to the sun is prohibited, but otherwise the lifestyle remains the same, no special diets are needed.
Development mechanisms
The nervous system consists of central and peripheral sections. The regulation mechanism between them works as follows: impulses from the receptors of the peripheral system are transmitted to the nerve centers of the spinal cord, and from there to the brain. The disruption of this complex mechanism causes demyelination.
Nerve fibers are covered with a myelin sheath. As a result of the pathological process under consideration, this membrane is destroyed and fibrous tissue is formed in its place. She, in turn, cannot conduct nerve impulses. In the absence of nerve impulses, the functioning of all organs is disrupted, since the brain cannot issue commands.
ICD 10 code
Demyelinating diseases of the brain ICD 10 have codes:
- G35-G37 – demyelinating diseases of the central nervous system;
- G35 – multiple sclerosis;
- G37 – other demyelinating diseases of the central nervous system. Diseases are different;
- G37.9 – demyelinating disease of the central nervous system, unspecified.
Diseases of the nervous system are classified in ICD 10 under the code G00-G99. Experts consider the classification according to ICD 10 to be insufficiently perfect. Another disability scale has been created that is used for multiple sclerosis - EDSS. This scale evaluates all conditions in multiple sclerosis - gait, balance, paralysis, self-care and other factors. To use the scale, the doctor takes a special exam to assess the patient’s condition.
Causes
Demyelinating diseases of the brain are characterized by damage to the peripheral and central nervous systems. They most often occur against the background of a genetic predisposition. It also happens that a combination of certain genes provokes disturbances in the functioning of the immune system. There are other causes of demyelinating diseases:
- state of chronic or acute intoxication;
- solar radiation;
- ionizing radiation;
- autoimmune processes in the body and genetic pathologies;
- complication of bacterial and viral infection;
- poor nutrition.
The Caucasian race is considered to be the most susceptible to this pathology, especially those representatives who live in northern latitudes. This type of disease can be provoked by a head or spinal injury, depression, or bad habits. Some types of vaccines can also trigger the development of such pathologies. This applies to vaccinations against measles, smallpox, diphtheria, influenza, whooping cough, and hepatitis B.
Causes
Demyelinating diseases affecting the central and peripheral nervous systems often develop against the background of a genetic predisposition. Patients often have a combination of certain genes that causes malfunctions of the immune system. Other reasons:
- Autoimmune and genetic pathologies.
- Taking antipsychotic drugs (neuroleptics).
- Chronic and acute intoxications.
- Ionizing radiation, solar radiation.
- Past viral and bacterial infections.
- Nutritional features.
It is believed that representatives of the Caucasian race living in northern latitudes are most susceptible to the development of pathology. Provoking factors are injuries to the head and spine, frequent stressful situations, and bad habits. The risk of getting sick increases due to vaccination against smallpox, influenza, measles, whooping cough, diphtheria, hepatitis type B and other infectious diseases.
Classification
Demyelinating disease of the nervous system is classified into different types, which are based on the destruction of the myelin sheath. In this regard, the pathology under consideration is divided accordingly into multiple sclerosis, Marburg disease, Devic disease, progressive multifocal leukoencephalopathy and Guillain-Barré syndrome.
Multiple sclerosis
Multiple sclerosis is characterized as a severe chronic and immunodegenerative disease of the central nervous system, prone to progression. In most cases, the disease occurs at a young age and almost always leads to disability. This demyelinating disease of the central nervous system is assigned code G35 according to ICD-10.
Currently, the causes of the development of multiple sclerosis are not fully understood. Most scientists are inclined to the multifactorial theory of the development of this disease, when genetic predisposition and external factors are combined. The latter include:
- infectious diseases;
- state of chronic intoxication;
- taking certain medications;
- change of place of residence with a sharp change in climate;
- lack of fiber and high-calorie diet.
The relationship between the symptoms of multiple sclerosis and the stage of the disease is not always clear. The pathology can have a wave-like course. Exacerbations and remissions can be repeated at varying intervals. A feature of multiple sclerosis is that each new exacerbation has a more severe course compared to the previous one.
The progression of multiple sclerosis is characterized by the development of the following symptoms:
- sensory disturbances (goosebumps, numbness, tingling, burning, itching);
- visual impairment (impaired color rendering, decreased visual acuity, blurred picture);
- trembling of the limbs or torso;
- headache;
- speech disorders and difficulty swallowing;
- muscle spasms;
- gait changes;
- cognitive impairment;
- heat intolerance;
- dizziness;
- chronic fatigue;
- libido disturbance;
- anxiety and depression;
- stool instability;
- insomnia;
- autonomic disorders.
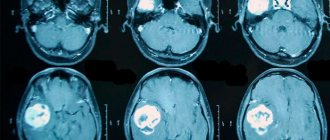
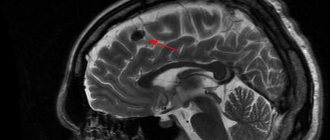
There are also secondary symptoms of multiple sclerosis. They imply complications of the disease. Foci of demyelination in the brain are determined using magnetic resonance imaging, including the introduction of a contrast agent.
Treatment of multiple sclerosis is carried out using methods such as:
- plasmapheresis;
- taking cytostatics;
- prescription of immunosuppressants;
- use of immunomodulators;
- taking beta interferons;
- hormonal therapy.
- symptomatic therapy with the prescription of antioxidants, nootropic drugs and vitamins.
During the period of remission, patients are prescribed sanatorium treatment, massage, and physical therapy. In this case, all thermal procedures should be excluded. To alleviate the symptoms of the disease, medications are prescribed: those that reduce muscle tone, eliminate tremors, normalize urination, stabilize the emotional background, and anticonvulsants.
Multiple sclerosis is classified as an incurable disease. Therefore, these treatment methods are aimed at reducing symptoms and improving the patient’s quality of life. The life expectancy of patients with this disease depends on the nature of the pathology.
What it is?
Demyelinating brain disease occurs secondary to infections - inflammatory, viral diseases or vaccinations, and is sometimes a consequence of a metabolic or genetically determined disorder of myelin metabolism. Other causes are hypoxic-ischemic damage, poisoning.
A risk factor for cerebral demyelination is febrile illness, and symptoms of the disease can be quite severe. In these diseases, there is a gradual destruction of myelin (= a lipoprotein formed with the help of proteins and fatty substances, the task of which is to accelerate the conduction of oxygen). Demyelinating disease lasts a relatively long time and gradually improves. Demyelinating diseases result from the destruction of myelin in both the CNS and PNS.
The most common demyelinating diseases are:
- multiple sclerosis;
- diffuse sclerosis, also known as Schilder's disease;
- polyneuropathy affecting the PNS;
- amyotrophic lateral sclerosis;
- ADEM = acute disseminated encephalomyelitis.
In accordance with ICD-10, demyelinating diseases are defined by the following code: G00-G99 – diseases of the nervous system → G35-G37 – demyelinating diseases of the central nervous system.
Marburg disease
Hemorrhagic fever or Marburg disease is an acute infectious pathology caused by the Marburg virus. It enters the body through damaged skin and mucous membranes of the eyes and mouth.
Infection occurs through airborne droplets and sexual contact. In addition, you can become infected through the blood and other secretions of the patient. After a person recovers from this disease, he develops a stable and long-lasting immunity. Re-infection was not encountered in practice. A person who has recovered from Marburg hemorrhagic fever experiences the formation of necrosis and foci of hemorrhage in the liver, myocardium, lungs, adrenal glands, kidneys, spleen and other organs.
The symptoms of the disease depend on the stage of the pathological process. The incubation period lasts from 2 to 16 days. The disease has an acute onset and is characterized by an increase in body temperature to high levels. Along with fever, chills may appear. Signs of intoxication increase, such as weakness, headache, pain in muscles and joints, intoxication and dehydration. 2-3 days after this, gastrointestinal dysfunction and hemorrhagic syndrome appear. A stabbing pain appears in the chest area, which intensifies during breathing. In addition, the patient may develop a dry cough and substernal stabbing pain. The pain may spread to the throat area. The mucous membrane of the pharynx becomes very red. Almost all patients experienced diarrhea, which lasted almost 7 days. A characteristic sign of this disease is the appearance of a measles-like rash on the body.
All symptoms intensify by the end of the first week. Bleeding from the nose, gastrointestinal tract, and genital tract may also be observed. By the beginning of week 2, all signs of intoxication reach their maximum. In this case, convulsions and loss of consciousness are possible. According to the blood test, specific changes occur: thrombocytopenia, poikilocytosis, anisocytosis, granularity of erythrocytes.
If a person is suspected of having Marburg disease, he is urgently hospitalized in the infectious diseases department and must be kept in an isolated box. The recovery period may take up to 21-28 days.
Main causes of demyelinating disease
Among the main reasons as a result of which demyelination of the brain begins to develop in the body are:
- The reaction of the human immune system to the protein that makes up myelin. As a result of irreversible processes that occur in the body, such a protein begins to be perceived by the immune system as foreign. The cells begin to attack it and gradually destroy it. This reason is the most dangerous. This mechanism can be triggered by the entry into the body of an infection or features of the human immune system that are hereditary in nature. These include multiple sclerosis, multiple encephalomyelitis, etc.
- The demyelinating process can begin in response to the presence of a neuroinfection that specifically affects myelin.
- Disturbance of metabolic processes in the body. As a result, myelin begins to suffer from a deficiency of the substances it needs and gradually collapses. This is possible in patients who have a history of diabetes and problems associated with the thyroid gland.
- The effect on the body of toxins and chemicals, including: alcohol, psychotropic drugs, acetone, waste products of the body.
- Paraneoplastic processes that occur as a complication of cancer.
As a result of scientific research, it was possible to establish that heredity and unfavorable environmental conditions play a special role in the damage to myelin (the sheath of nerve fibers). There is also information about the connection between the likelihood of the occurrence of this disease and the geographic location of a person, where foci of demyelination are noted.
An important role in the development of demyelinating brain disease is played by stress, poor nutrition, viruses (among which the most common are herpes, measles, rubella, etc.), bacteria and poor ecology.
There are two types of brain demyelination:
- Myelinoclasty - characterized by a hereditary predisposition to the rapid destruction of the myelin sheath.
- Myelinopathy is a process of destruction of the myelin sheath that has other causes.
Devic's disease
Neuromyelitis optica or Devic's disease has a chronic pattern similar to multiple sclerosis. This is an autoimmune disease, the causes of which are still unclear. One of the reasons for its development is an increase in the permeability of the barrier between the meninges and the vessel.
Some autoimmune diseases can trigger the progression of Devic's disease:
- rheumatoid arthritis;
- systemic lupus erythematosus;
- Sjögren's syndrome;
- dermatomyositis;
- thrombocytopenic purpura.
The disease has specific symptoms. Clinical manifestations are caused by disruption of conductive impulses. In addition, the optic nerve and spinal cord tissue are affected. In most cases, the disease manifests itself as visual impairment:
- a veil before the eyes;
- pain in the eye sockets;
- blurred vision.
As the disease progresses and there is no adequate treatment, the patient runs the risk of completely losing his vision. In some cases, regression of symptoms with partial restoration of eye function is possible. Sometimes it happens that myelitis precedes neuritis.
Neuromyelitis optica has two course options: a progressive increase in symptoms with simultaneous damage to the central nervous system. In rare cases, a monophasic course of the disease occurs. It is characterized by steady progress and worsening symptoms. In this case, the risk of death is increased. With the right treatment, the pathological process slows down, but complete recovery is not guaranteed.
The second option, the most common, is characterized by an alternating change of remission and exacerbation and is designated by the concept of “recurrent course.” It is also accompanied by visual disturbances and spinal cord dysfunction. During the period of remission, a person feels healthy.
To identify Devic's disease, a set of measures is carried out. In addition to standard diagnostic procedures, lumbar puncture with cerebrospinal fluid analysis, ophthalmoscopy and MRI of the spine and brain are performed.
Treatment of Devic's disease is long and difficult. The main goal is to slow the progression of the disease and improve the patient’s quality of life. As part of drug therapy, glucocorticosteroids, muscle relaxants, antidepressants, and centrally acting painkillers are used. In severe cases of the disease, the patient may face complications such as paralysis of the legs, blindness, or persistent dysfunction of the pelvic organs. With timely and correct treatment, a complete recovery is guaranteed.
How is the diagnosis made?
The diagnosis of “focal changes in the brain substance of a dystrophic nature” is quite difficult to establish. This requires identifying the signs of the pathologies listed above and excluding other somatic diseases and possible neuroses. By the way, people with diabetes and rheumatism are also at risk.
The doctor must assess the patient’s condition, his neurological status, and also conduct the necessary examinations. The most accurate indications are provided by an MRI study, where lesions can be identified, as well as their size and location. Tomography makes it possible to determine changes in the density of brain tissue even in the initial stage of the disease. Correctly reading the MRI results is an important step in starting treatment for the problem described.
Progressive multifocal leukoencephalopathy
People with immune deficiency may experience progressive multifocal multifocal leukoencephalopathy. This is an infectious disease caused by the penetration of the JC virus, which belongs to the Polyomavirus family, into the body. A feature of the pathology is that asymmetric and multifocal brain damage occurs. The virus affects the membranes of nerve endings, which are made of myelin. Therefore, this disease belongs to the group of demyelinating pathologies.
Almost 85% of patients with this diagnosis are AIDS or HIV infected. The risk group includes patients with malignant tumors.
Main symptoms of the disease:
- mood swings;
- visual disturbances;
- paresthesia and paralysis;
- memory impairment.
Multiple sclerosis
This is the most common of the demyelinating diseases. Its peculiarity is that foci of demyelination are located in several parts of the central nervous system, so the symptoms are varied. The first signs of the disease appear at the age of about 25 years, more often in women. In men, multiple sclerosis is less common, but progresses more rapidly.
Guillain-Barre syndrome
An acute inflammatory disease characterized by “demyelinating polyradiculoneuropathy.” It is based on autoimmune processes. The disease manifests itself as sensory disturbances, muscle weakness and pain. It is characterized by hypotension and disorder of tendon reflexes. Respiratory failure may also occur.
All patients with this diagnosis should be admitted to the intensive care unit. Since there is a risk of developing respiratory failure and a ventilator may be required, the department must have intensive care. Patients also need proper care with the prevention of bedsores and thromboembolism. It is also necessary to stop the autoimmune process. For this purpose, plasmapheresis and pulse therapy with immunoglobulins are used. Full recovery of patients with this diagnosis should be expected within 6-12 months. Deaths occur due to pneumonia, respiratory failure and pulmonary embolism.
What is the demyelinating process?
Some nerve endings (in particular, axons of the peripheral and central nervous systems) are covered with a specific myelin sheath. This structure performs a number of important functions. In particular, myelin is responsible for the speed of transmission of electrical impulses along nerve fibers. In addition, the membrane performs barrier and support functions, and is also responsible for nourishing nerve endings.
Demyelinating brain disease is accompanied by some damage to the myelin sheath, which naturally affects the functioning of nerve cells. By the way, demyelinating diseases are a whole group of certain lesions of the nervous system, each of which has its own characteristics and is accompanied by a unique set of symptoms.
Symptoms
Demyelination always manifests itself as a neurological deficit. This sign indicates the beginning of the process of myelin destruction. The immune system is also involved. Brain tissue - spinal and brain - atrophies, and expansion of the ventricles is observed.
Manifestations of demyelination depend on the type of disease, causative factors and location of the lesion. Symptoms may be absent when the damage to the brain substance is minor, up to 20%. This is due to a compensatory function: healthy brain tissue performs the tasks of the affected areas. Neurological symptoms rarely appear - only when more than 50% of the nervous tissue is damaged.
The following are common signs of demyelinating brain diseases:
- paralysis;
- limited muscle mobility;
- tonic spasms of the limbs;
- dysfunction of the intestines and bladder;
- pseudobulbar syndrome (impaired pronunciation of sounds, difficulty swallowing, change in voice);
- impaired fine motor skills of the hands;
- skin numbness and tingling;
- visual dysfunction (decreased visual acuity, blurred images, fluctuations in the eyeballs, color distortions).
Neuropsychological disorders characteristic of the pathology in question are caused by memory deterioration and a decrease in mental activity, as well as changes in behavior and personal qualities. This is manifested by the development of neuroses, depression, dementia of organic origin, emotional swings, severe weakness and decreased performance.
Main symptoms
Demyelination is a pathology that always manifests itself as a neurological deficit, which makes it possible to suspect the beginning of the process of myelin destruction if neurological symptoms appear without obvious reasons. The demyelinating process always occurs with the participation of the immune system, leading to atrophy of brain tissue - brain and spinal cord, and dilation of the ventricles.
Symptoms of demyelination depend on the type of disease, the causes and localization of the lesion in the brain, spinal cord or in the structures of the PNS. With minor damage to the brain substance (up to 20%), symptoms may be absent, which is associated with complete compensation of functions. The tasks assigned to damaged nerve fibers are performed by healthy tissues. Neurological symptoms usually appear in cases where the amount of nerve tissue damaged exceeds 50%. General signs:
- Ataxia (disorder of coordination when working a muscle group).
- Paresis, paralysis.
- Muscular hypotonia (muscle weakness).
- Pseudobulbar syndrome (dysarthria - impaired pronunciation due to a disorder of the innervation of the elements of the speech apparatus, dysphagia - difficulty swallowing, dysphonia - changes in pitch, timbre, strength of the voice).
- Visual dysfunction (nystagmus - involuntary oscillations of the eyeballs, deterioration of visual acuity, loss of visual fields, blurred, unclear images, color distortion).
- Changes in skin sensitivity, paresthesia (numbness, tingling, itching, burning).
- Tonic spasms, mainly in the extremities.
- Bladder and bowel dysfunction.
Neuropsychological disorders are associated with deterioration of memory and mental activity, changes in personality and behavior. Patients often develop neuroses, dementia of organic origin, asthenic syndrome, depression, and less often euphoria. Patients are subject to sudden changes in mood, they lack a critical analysis of their own behavior, which, against the background of dementia, leads to numerous problems in everyday life.
Diagnostics
An early stage of the pathology with the absence of characteristic symptoms is accidentally discovered during a diagnostic examination for another reason. To confirm the diagnosis, neuroimaging is performed, and the neurologist determines the degree of impairment of the conductive function of the brain. The main diagnostic method is magnetic resonance imaging. In the photographs you can clearly see areas of the affected tissue. If you do angiography, you can determine the extent of vascular damage.
Demyelinating brain disease: symptoms
Of course, many people are interested in what changes they need to pay attention to. Unfortunately, the symptoms in this case depend on the location of the lesions, the stage and characteristics of the course of the disease.
Naturally, there are some signs that may indicate that a person is developing one or another demyelinating brain disease. As a rule, first of all, the patient develops increased fatigue and decreased performance. The main symptoms also include varying degrees of incoordination, as well as changes in gait and tremor.
In addition, some patients note changes in sensitivity - it can either increase or decrease or even disappear completely. Signs include periodic burning and tingling sensations in the extremities.
In addition, demyelinating disease of the brain can also cause disturbances in the functioning of the pelvic organs. For example, some patients experience fecal or urinary retention or, conversely, incontinence.
Naturally, such diseases also affect a person’s mental state. Depressive states and certain behavioral disorders may develop. Often, progressive demyelination causes a decrease in the level of intelligence.