Lesions in the white matter of the brain are areas of damage to brain tissue, accompanied by a violation of the mental and neurological functions of higher nervous activity. Focal areas are caused by infection, atrophy, loss of blood supply and trauma. Most often, affected areas are caused by inflammatory diseases. However, areas of change may also be of a dystrophic nature. This is observed mainly as a person ages.
Focal changes in the white matter of the brain can be local, single-focal, or diffuse, that is, the entire white matter is moderately affected. The clinical picture is determined by the localization of organic changes and their degree. A single lesion in the white matter may not affect the dysfunction, but massive damage to neurons causes a disruption in the functioning of nerve centers.
Symptoms
The set of symptoms depends on the location of the lesions and the depth of damage to the brain tissue. Symptoms:
- Pain syndrome. Characterized by chronic headaches. Unpleasant sensations intensify as the pathological process deepens.
- Rapid fatigue and exhaustion of mental processes. Concentration deteriorates, the volume of operative and long-term memory decreases. It is difficult to master new material.
- Flattening of emotions. Feelings lose their sharpness. Patients are indifferent to the world and lose interest in it. Previous sources of pleasure no longer bring joy and desire to engage in them.
- Sleep disturbance.
- In the frontal lobes, foci of gliosis disrupt the control of the patient’s own behavior. With deep violations, the concept of social norms may be lost. Behavior becomes provocative, unusual and strange.
- Epileptic manifestations. More often these are small convulsive seizures. Individual muscle groups contract involuntarily without threat to life.
White matter gliosis can manifest itself in children as a congenital pathology. The lesions cause dysfunction of the central nervous system: reflex activity is disrupted, vision and hearing deteriorate. Children develop slowly: they get on their feet late and begin to speak.
EPIDEMIC FOCUS
Epidemic focus
(Greek epidemos common among the people; synonymous
with focus of infectious disease
) - the location of the source of infection and the surrounding area, within which the spread of the pathogen is possible, which is due to the corresponding transmission mechanism.
The epidemic focus is the main element of the epidemic process (see). The dimensions (boundaries) of the outbreak, with a certain degree of convention, are determined by the specific features of the transmission mechanism, as well as the degree of activity of the pathways and factors of transmission of the causative agent of a given infectious disease in specific social, everyday and natural conditions. As a rule, in diseases with natural focality (see), the boundaries of the epidemic focus are much wider than in anthroponoses (see).
An epidemic focus is usually discovered in connection with the identification of a patient with a manifest infectious disease, less often - as a result of a laboratory examination of clinically healthy people. At the same time, the most dangerous in epidemic terms are patients with atypically occurring forms of infectious diseases, as well as people who communicated with them, who are in the incubation period of the disease, or healthy carriers of the infectious agent.
The main measures taken in an epidemic outbreak with the aim of eliminating it (see Anti-epidemic measures) consist of identifying, isolating and sanitizing all patients, regardless of the clinical form of the disease. However, an epidemic focus can remain active even after the source(s) of infection have been neutralized, if the pathogen remains viable in the environment (for example, an epidemic focus of acute intestinal infections) or in the body of arthropod carriers (for example, an epidemic focus of blood infections). Therefore, the second most important measure to eliminate an epidemic outbreak is disinfection (see), disinsection (see) and deratization (see).
The concept of “epidemic focus” cannot be identified with the concepts of “focus of infection” and “focus of infection”. A “focus of infection” means a territory exposed to bacteriological weapons (see Focal point of mass casualties); with a “focus of infection”, which is associated with local pathological changes in the body of a particular patient, caused by the local influence of microorganisms or the action of toxic products of their vital activity.
Bibliography:
See bibliography. to Art. Epidemiology.
P. N. Burgasov, A. A. Sumarokov.
Causes
Damaged areas in the white matter are caused by the following diseases and conditions:
- Group of vascular diseases: atherosclerosis, amyloid angiopathy, diabetic microangiopathy, hyperhomocysteinemia.
- Inflammatory diseases: meningitis, encephalitis, multiple sclerosis, systemic lupus erythematosus, Sjogren's disease.
- Infections: Lyme disease, AIDS and HIV, multifocal leukoencephalopathy.
- Poisoning by substances and heavy metals: carbon monoxide, lead, mercury.
- Vitamin deficiency, especially B vitamins.
- Traumatic brain injuries: bruise, concussion.
- Acute and chronic radiation sickness.
- Congenital pathologies of the central nervous system.
- Acute cerebrovascular accident: ischemic and hemorrhagic stroke, cerebral infarction.
Symptoms of dystrophy of the brain substance
It is better to prevent any disease than to treat it later, and for this you need to know its external manifestations (signs) and symptoms.
- First stage. In the first couple of days, a person feels a little tired, lethargic, dizzy and sleeps poorly. This occurs due to decreased blood circulation in the brain. The degree of significance increases with the development of vascular diseases: cholesterol deposition, hypotension, etc.
- Second stage. At the second stage, a so-called “disease focus” appears in the brain; damage to the brain substance deepens due to poor blood circulation. The cells do not receive enough nutrition and gradually die. The beginning of this stage is indicated by memory impairment, loss of coordination, noise or “shooting” in the ears and severe headaches.
- Third stage. Due to the discircular nature of the last stage, the focus of the disease moves even deeper, the affected vessels bring too little blood to the brain. The patient exhibits signs of dementia, lack of coordination of movements (not always), dysfunction of the sensory organs is possible: loss of vision, hearing, shaking hands, etc.
The exact changes in the brain substance can be determined using MRI.
Without treatment, diseases such as:
- Alzheimer's disease. The most common form of nervous system degeneration.
- Pick's disease. A rare progressive disease of the nervous system, manifesting itself from 50-60 years of age.
- Huntington's disease. Genetic disease of the nervous system. developing from 30-50 years.
- Arterial hypertension.
- Cardiocerebral syndrome (impairment of basic brain functions due to cardiac pathology).
At-risk groups
Risk groups include people exposed to the following factors:
- Arterial hypertension. They are at increased risk of developing vascular lesions in the white matter.
- Poor nutrition. People who overeat, excessively consume extra carbohydrates. Their metabolism is disrupted, as a result of which fatty plaques are deposited on the inner walls of blood vessels.
- Foci of demyelination in the white matter appear in older people.
- Smoking and alcohol.
- Diabetes.
- Sedentary lifestyle.
- Genetic predisposition to vascular diseases and tumors.
- Constant hard physical labor.
- Lack of intellectual work.
- Living in conditions of air pollution.
Treatment
Individual changes in the white matter, which are clearly visible on MRI, may mean that the patient has abnormalities in the blood circulation of the brain of vascular origin. Based on these data, the doctor will prescribe an examination that will more clearly show the causes of this situation and allow you to prescribe the correct treatment.
To select treatment for focal changes in the brain substance of a dyscirculatory nature, the doctor first prescribes therapy for the disease that led to this situation. Drugs are prescribed that improve blood circulation between brain structures, oxygen exchange, reduce blood viscosity, have a sedative and analgesic effect, as well as complexes of vitamins and essential elements.
Diagnostics
Focal changes in the brain are difficult to diagnose in the initial stage. Detection of pathology is made difficult by the rather sparse symptoms.
Ultrasound diagnostics with Doppler sonography reveals abnormalities in the vessels of the brain (asymmetry, increased venous blood flow, stenosis, atherosclerosis). CT scan (computed tomography) determines previous heart attacks, accumulation of fluid in cavities and thinning of tissues (atrophy of brain structures).
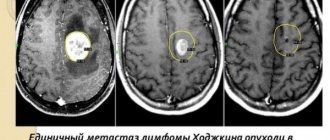
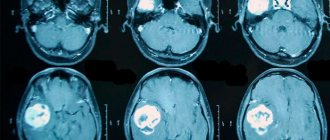
The most reliable and accurate results can only be obtained by examining magnetic resonance imaging (MRI) of the skull. The image is obtained by interacting an electromagnetic field with hydrogen atoms.
This diagnosis allows you to evaluate the functioning of neurons and detect changes in the density of brain tissue. Having identified asymptomatic stages of focal lesions, it is possible to begin timely therapy.
MRI allows you to obtain images in three planes (transverse, longitudinal and frontal) and identify the cause of malnutrition of brain structures:
- Necrotic single lesion in the cerebral cortex, resulting from narrowing or closure of a spinal artery by a thrombus (congenital pathologies, the result of atherosclerosis or spinal hernia);
- Multiple focal lesions – pre-stroke condition (diagnosis allows timely treatment to begin and the development of irreversible processes to be prevented);
- Changes in the frontal or parietal lobe - small lesions that occur with hypertension and crises;
- Microfocal lesions - diagnosed by injection of a contrast agent, typical for older patients, or the presence of congenital anomalies.
Mechanism of development of central nervous system lesions
Residual damage to the central nervous system is always caused by unfavorable factors that preceded it.
In most cases, the basis for the pathogenesis of such symptoms is cerebral ischemia. In children, it develops during the period of intrauterine development. Due to insufficient blood supply to the placenta, the fetus receives little oxygen. As a result, the full development of nervous tissue is disrupted, and fetopathy occurs. Significant ischemia leads to intrauterine growth retardation and the birth of a child before the gestational age. Symptoms of cerebral hypoxia can appear already in the first days and months of life. Residual organic damage to the central nervous system in adults often develops due to traumatic and infectious causes. Sometimes the pathogenesis of nervous disorders is associated with metabolic (hormonal) disorders.
Pathologies
Focal changes in the substance of the brain of a dystrophic nature most often take the form of pathologies such as:
- A cyst is a small cavity that is filled with fluid. It often interferes with the normal functioning of neighboring areas of the brain, as it compresses blood vessels. Cysts are divided into intracerebral (cerebral) and arachnoid. The latter appears in the meninges. Its occurrence is promoted by the accumulation of cerebrospinal fluid and inflammatory processes. Cerebral occurs in place of dead brain tissue.
- Necrotic state of tissue - appears when the supply of important nutrients to areas of the brain for any reason deteriorates. Dead cells form so-called dead zones and are not regenerated.
- Hematomas and brain scars occur after severe trauma or concussion. Foci of this type lead to structural damage.