Doctor Vadim Berezhnoy
Founder of the MediGlobus platform. Medical expert, Head of the department of coordinating doctors.
Astrocytoma is the most common and one of the most aggressive types of brain tumors. The neoplasm turns out to be malignant in 50% of detected cases. For patients whose tumor has been confirmed to be benign, it is important to begin treatment immediately. If you do not undergo therapy in a timely manner, astrocytoma is likely to develop into malignant one.
Features of the tumor
Astrocytoma is characterized by aggressiveness and rapid growth. A tumor at the first stage is considered benign. It has clear boundaries with surrounding tissues (focal astrocytoma), so it is quite easily removed. As the tumor grows, it becomes malignant. The boundaries of its tissues lose clarity (diffuse astrocytoma), which complicates surgical treatment.
Astrocytoma can form in all areas of the brain. Often the tumor cannot be completely removed due to the fact that it is located in an inoperable area or important blood vessels pass close to it. In such cases, other methods of therapy are prescribed.
Diagnostics
To detect neurological disorders, a number of special tests are performed, thanks to which it is possible to see damage to the brain. To clarify the diagnosis, specialists prescribe an examination to obtain images of the organ and the skull as a whole.
On this topic
- central nervous system
What are the dangers of a porencephalic cyst of the brain?
- Olga Vladimirovna Khazova
- May 27, 2021
The pictures will clearly show the condition of the bones. Such a study makes it possible to exclude pathology and head injuries, as well as identify symptoms of intracranial hypertension and the presence of fibrillary astrocytoma. The disadvantage of craniography is its lack of information content.
In order to confirm or refute information about the development of the disease, more modern diagnostic examination methods are used, which make it possible not only to establish the pathology, but also to determine the size, location of the tumor and the degree of progression.
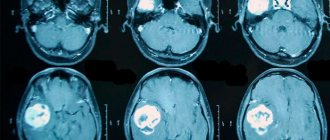
Magnetic resonance imaging
The basis of MRI is magnetic resonance, the essence of which is the action of a powerful magnet on a damaged organ, as a result of which each structure emits different frequency signals that are picked up by the scanner and converted into an image.
MRI allows you to obtain images of all parts of the brain in three-dimensional format. The duration of the procedure is about 30 minutes.
All the time the person is inside the magnet in a motionless state. A gadolinium-based contrast agent may also be used for the study.
CT scan
The patient lies down on the table. The tomograph is positioned so that it is at head level.
On this topic
- central nervous system
Everything you need to know about pituitary adenoma
- Olga Vladimirovna Khazova
- February 28, 2021
The work is based on the same principle as an x-ray, but the result is several images from different angles. The data undergoes computer processing, and the result is displayed in the form of layer-by-layer images of the brain.
To obtain the most accurate result, contrast is used to highlight the necessary areas of the organ being examined. The procedure is inexpensive and allows you to obtain information not only about the condition of bones, but also soft tissues.
Positron emission tomography
The study consists of intravenous administration of a radiopharmaceutical. After 30 minutes, the drug is absorbed by the brain and scanned.
As a result, the specialist receives a three-dimensional model of the organ, which clearly identifies areas with low activity, which indicates the presence of pathological disorders.
Treatment methods for astrocytoma
Since this type of brain tumor is aggressive and grows rapidly, its treatment requires urgency and a comprehensive approach. Treatment methods for astrocytoma are: surgery, radiotherapy, chemotherapy, targeted therapy, and a combination of these.
Chemotherapy
- The drugs are taken orally, administered intravenously or into the brain in the form of implants containing cytostatics (the method is used in later stages).
The purpose of administering chemotherapy is the total destruction of cancer cells. Substances enter the blood and are distributed throughout the body. Healthy cells are also susceptible to the effects of drugs. Due to the intense side effects, chemotherapy is often contraindicated.
Targeted therapy
- Treatment method using special drugs. Once in the body, the active components of such medications can “recognize” healthy and pathological cells. Unlike chemotherapy, targeted drugs affect only the tissues of the pathological neoplasm, therefore the side effects are less dangerous (healthy organs and systems are practically not damaged). Targeted therapy is prescribed for large tumors.
Surgical treatment
Surgery is the main method of treating astrocytoma; depending on the severity of the disease, it is prescribed for different purposes: for complete resection of the tumor and removal of the maximum accessible part - this reduces intracranial pressure and generally alleviates the patient’s condition.
Surgery is necessary for a biopsy. Material is collected for further examination of the tumor using a puncture needle through a small hole in the skull. The tissue sample taken is examined under a microscope to determine whether it is benign or malignant.
Radiation therapy
Can be prescribed before and after surgery. Before surgery, radiotherapy is prescribed to reduce the size of the formation, and after excision, to kill any remaining pathological cells.
In cases where astrocytoma is considered inoperable, radiation therapy is usually the main treatment option. With its help, it is possible to significantly reduce the size of the tumor, which improves the patient’s physical condition and often increases life expectancy. In foreign clinics, innovative radiotherapy techniques are used:
Stereotactic radiosurgery and radiotherapy
– a high dose of radiation is delivered to tumor tissue without affecting healthy cells.
Can be carried out in one session or in a course. Brachytherapy
is internal irradiation in which a radioactive element is injected directly into pathological tissues.
The area of its influence is very limited, so healthy cells are not affected. Craniospinal radiotherapy
is irradiation of the entire spinal cord during the formation of metastases.
Brain astrocytoma: causes of occurrence
Scientists have already identified the main factors that are present in most patients with astrocytoma:
- heredity burdened with cancer;
- unfavorable environmental, economic, social factors;
- traumatic brain injury;
- chronic concomitant diseases that cause intoxication of the body;
- hormonal changes in the body, such as pregnancy or menopause;
- excessive consumption of alcoholic beverages;
- occupational hazards (for example, radiation, oil refining or working with paint materials);
- viral infections with a high degree of oncogenicity.
The exact causes of the development of the disease have not yet been sufficiently studied, but it is easy to notice that modern people encounter most of the provoking factors quite often. It cannot be said for sure that these factors are absolute provocateurs of the development of cancer, but it has been proven that they have a detrimental effect on the body as a whole. Therefore, it is necessary to take care of your health and protect yourself from their excessive exposure, conduct timely preventive examinations, and also not delay diagnosis if complaints from the brain arise.
Surgery for astrocytoma: indications for performance
In addition to removing the tumor, the goals of treatment are also to improve the patient's well-being and prolong the life of the patient. Therefore, when choosing a treatment method, all risks and possible side effects are carefully assessed, and the success of treatment is predicted. Based on such a comprehensive diagnosis, a decision is made on the advisability of the operation.
Indications for surgical treatment of astrocytoma are the following factors: the tumor has already reached a large size and continues to grow, it is in a place accessible to instruments, the physical condition and age of the patient allow the operation to be performed.
Forecast
With fibrillary astrocytoma, the prognosis is quite positive, since the difference between this type of disease is the slow growth of tumors. Deterioration of prognostic data is possible when the tumor degenerates into a malignant form or its diffuse growth is observed.
Timely treatment does not affect the patient's life expectancy in any way.
With rapid progression, the risk of premature death increases as a result of damage to brain structures.
How is the operation performed?
Surgery to remove a tumor in the brain does not require special preparation, with the exception of the patient receiving a fluorescent substance. The components of this drug accumulate in the tumor, which increases its visibility and reduces the risk of affecting nearby vessels.
In most cases, the patient is under general anesthesia during the operation. If the tumor is located near important functional centers (speech, visual), the patient remains conscious. During the operation, a conversation is held with the patient and his perception is checked. There are two main methods used to treat brain astrocytoma:
Endoscopic craniotomy
Minimally invasive surgery method. The tumor is removed with an endoscope inserted through small holes. The duration of the operation is from 2 to 4 hours.
Open surgery with removal of part of the bone tissue of the skull
The patient's head is in a state of fixation with a special clamp. The tumor is removed microsurgically using a navigation system. The operation lasts up to 6 hours.
Causes
To date, it has not been possible to identify the exact provoking factors contributing to the development of fibrillar-protoplasmic astrocytoma. Thanks to some studies, gene abnormalities have been identified in various chromosomes of astrocytes, which can affect the genesis of the pathological process. In addition, natural aging of the brain can provoke the disease.
On this topic
- central nervous system
How does a headache with a brain tumor hurt?
- Natalya Gennadievna Butsyk
- December 3, 2021
In most cases, tumor neoplasms are not associated with heredity, but they are associated with certain congenital conditions, among which are:
- tuberculous sclerosis;
- neurofibromatosis;
- Turcotte's syndrome;
- von Hippel-Lindau disease;
- Li-Fraumeni syndrome.
Such disorders are diagnosed in only 5 percent of cases in people who suffer from astrocytoma.
Rehabilitation after surgery
Upon completion of the operation, the patient is transferred to the intensive care unit, where he is under the care of nurses and physical therapists for 7-10 days. A few days after surgery, a CT or MRI is prescribed.
If no complications arise, the patient is transferred to a rehabilitation center. On an individual basis, it is possible to transfer to a clinic at your place of residence. The period of complete rehabilitation after treatment of astrocytoma is approximately 3 months. During this period, the patient undergoes a recovery program prescribed by the doctor. They are compiled individually and may include exercise therapy, massages, visits to a psychologist, classes with a speech therapist and other rehabilitation techniques.
Treatment
If diagnosed early, diffuse astrocytoma is completely curable. If there is a slow progression of the pathological process, then a wait-and-see approach cannot be ruled out.
In this case, the patient must be regularly examined to assess the rate of progression of the disease. In this case, it is necessary to adhere to a healthy lifestyle, proper nutrition and supportive drug therapy.
Surgery
If diffuse proliferation of tumor cells is observed, they cannot be completely eliminated. It is possible to achieve a positive effect with classical surgery in the presence of dense tumors.
Before operating on a patient, he is given a drug that increases the expression of pathogenic cells. The entire operation process takes place under microscopic control, which allows you to completely remove tumor cells without affecting healthy ones.
Surgical removal requires a long rehabilitation period.
Chemotherapy
It is advisable to use in the early stages of the disease. However, the tumor does not always respond to this treatment method. Only in 30 percent of cases is it possible to achieve positive dynamics.
If there is no result, surgical removal of the tumor is prescribed.
Radiosurgery
Tumor tissues are exposed to ionizing radiation. In this case, unaffected areas are not affected. This type of intervention is controlled by a tomographic device.
Often, several stages are required to eliminate a tumor. After such therapy, in rare cases, complications from the neurological system occur.
Radiation therapy
This type of treatment is used in the presence of astrocytomas no larger than two centimeters in size. A full therapeutic course includes from 5 to 30 sessions, which in some cases makes it possible to achieve complete regression of the disease.
Prognosis after surgery
If the tumor can be completely removed, 5-year recurrence-free survival is achieved in 90% of cases. If it was possible to carry out only partial resection of the formation, there remains a high risk of relapse of the disease.
- The success rate of treatment for piloid astrocytoma of the brain (grade 1 malignancy) is 90%. After treatment of fibrillary astrocytoma (stage 2), the average life expectancy is 6-8 years. 40% of patients who undergo complete tumor removal live more than 10 years. The positive prognosis for treatment of anaplastic astrocytoma (stage 3) is 27%. If a grade 4 tumor (glioblastoma) is detected, the average life expectancy is 12-18 months. 5% of patients manage to prolong life by 3 years. A more favorable prognosis is observed in children: the success rate of treatment of astrocytoma at stages 3-4 is 25%.
Publications in the media
Astrocytomas are a large and most common group of primary tumors of the central nervous system, differing in location, sex and age distribution, growth pattern, grade of malignancy and clinical course. All astrocytomas are of “astroglial” origin. Incidence: 5–7:100,000 population in developed countries.
For all astrocytomas, a universal grading system (WHO) is used according to the histological criterion of “grade of malignancy” • Grade 1 (piloid astrocytoma): there should be no sign of anaplasia • Grade 2 (diffuse astrocytoma): 1 sign of anaplasia, more often nuclear atypia • Grade Grade 3 (anaplastic astrocytoma): 2 signs, most often nuclear atypia and mitoses • Grade 4 (glioblastoma): 3–4 signs: nuclear atypia, mitoses, vascular endothelial proliferation and/or necrosis.
There are a number of clinicopathological groups of astrocytomas.
Diffuse-infiltrative astrocytoma. This concept unites several types of tumors of varying degrees of malignancy.
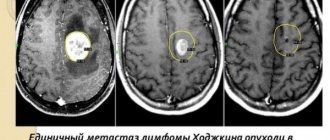
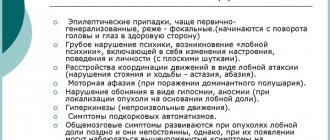
• Diffuse astrocytoma (WHO-2) - 10-15% of all brain astrocytomas, peak incidence 30-40 years, men/women - 1.2:1; are more often located supratentorially in the cerebral hemispheres. Clinical picture. Most often, these tumors manifest as an episyndrome, focal neurological deficit, and signs of increased ICP appear at a late stage of disease development. Diagnostics. Tumors have characteristic CT and MRI semiotics. Treatment. Tactics: tumor removal or observation/symptomatic therapy (the decision can be made only after consultation with a neurosurgeon). The previously popular tactic - biopsy + radiation therapy - has no advantage over “observation”. Prognosis: The average life expectancy after surgery is 6–8 years with marked individual variations. The clinical course of the disease is mainly influenced by the tendency of these tumors to malignant transformation, which is usually observed 4–5 years after diagnosis. Clinically favorable prognostic factors are young age and “total resection” of the tumor. Among diffuse astrocytomas, a number of histological variants are distinguished •• Fibrillar astrocytoma is the most common variant, consisting mainly of fibrillar tumor astrocytes. Nuclear atypia is a diagnostic criterion. Mitoses, necrosis, and endothelial proliferation are absent. The cell density in the specimen is low to moderate •• Protoplasmic astrocytoma is a rare variant, consisting primarily of tumor astrocytes with a small body and thin processes. The cell density in the preparation is low. Characteristic features are mucoid degeneration and microcysts •• Gemistocytic astrocytoma. This variant is characterized by the presence of a significant fraction of gemistocytes in fibrillary astrocytoma (usually more than 20%). A gemistocyte is a variant of an astrocyte with a large, angular, misshapen eosinophilic body.
• Anaplastic astrocytoma (WHO-3) accounts for 20-30% of all brain astrocytomas, peak incidence 40-45 years, men/women -1.8:1; are most often located supratentorially in the cerebral hemispheres. At the moment, the dominant point of view is that anaplastic astrocytoma is the result of malignant transformation of diffuse astrocytoma. Its pathomorphology is characterized by signs of diffuse infiltrative astrocytoma with severe anaplasia and high proliferative potential. The clinical picture is in many ways similar to diffuse astrocytoma, but signs of increased ICP are more common, and there is a more rapid progression of neurological symptoms. Diagnosis: tumors do not have characteristic CT and/or MRI semiotics and can often appear as diffuse astrocytoma or glioblastoma. Treatment: at the moment, the standard treatment algorithm is combination treatment (surgery, radiation therapy, polychemotherapy). Forecast. The average life expectancy after surgery and adjuvant treatment is about 3 years. The clinical course of the disease is mainly influenced by transformation into glioblastoma, which is usually observed 2 years after diagnosis. Clinically favorable prognostic factors are young age, “total resection” of the tumor, and good preoperative clinical status of the patient. The presence of an oligodendroglial component in the tumor may increase survival to >7 years.
Glioblastoma (GBM) and its variants (WHO-4). It is the most malignant of astrocytomas and accounts for about 50% of all astrocytomas of the brain, peak incidence 50–60 years, men/women - 1.5:1; most often located supratentorially in the cerebral hemispheres. There are primary (more often) and secondary GBM (as a result of malignancy of diffuse or anaplastic astrocytoma). Its pathomorphology is characterized by signs of diffuse infiltrative astrocytoma with severe anaplasia, high proliferative potential, signs of endothelial proliferation and/or necrosis. Clinical picture. Primary GBM is characterized by a short medical history, dominated by nonspecific neurological symptoms and rapidly progressive intracranial hypertension. In secondary GBM, the clinical picture is largely similar to anaplastic astrocytoma. Diagnostics. The tumor has characteristic CT and MRI semiotics; differential diagnosis is usually carried out with metastasis and abscess. Characteristic is the invasive growth of the tumor along long conductors (GBM in the form of a “butterfly” when growing through the corpus callosum). Treatment. At the moment, the standard treatment algorithm is combination treatment (surgery and radiation therapy; the role of polychemotherapy in increasing survival in GBM has not yet been reliably proven, and the need for its implementation is considered only in cases where all other treatment methods have been carried out and turned out to be ineffective (“ therapy of despair." Prognosis: The average survival after surgery and adjuvant treatment is about 1 year. Clinical favorable prognostic factors are similar to those for anaplastic astrocytoma.
In addition to the typical glioblastoma multiforme, the following histological variants are distinguished: • Giant cell glioblastoma is characterized by a large number of giant, ugly multinucleated cells • Gliosarcoma is a two-component malignant tumor with foci of both glial and mesenchymal differentiation.
Pilocytic (piloid) astrocytoma is a tumor of childhood, characterized by a relatively “demarcated” growth pattern (in contrast to diffuse astrocytomas) and has characteristic features of localization, morphology, genetic profile and clinical course. It belongs to the lowest (1st degree of malignancy according to the WHO classification for tumors of the central nervous system) and has the most favorable prognosis. More often occurs before the age of 20 years. The most common localization is the cerebellum, visual pathways, and brain stem. The clinical picture is characterized by a very slow increase in both focal (depending on the location of the tumor) and general cerebral symptoms with good adaptation of the body. Particularly characteristic is the slow increase in occlusive hydrocephalus with tumors of the cerebellum and brainstem. Diagnostics. The tumor has characteristic CT and MRI semiotics, which allows, together with the clinical picture, to make a diagnosis before surgery. The standard preoperative examination of such patients is contrast-enhanced MRI. Treatment is surgical; the goal of the operation is “total removal” of the tumor, which is often impossible due to its location (brain stem, hypothalamus). Forecast. Survival of patients is often more than 10–15 years, and therefore exact survival rates do not exist due to difficulties in analyzing such a long follow-up. Note. Among piloid astrocytomas (usually hypothalamic), there is a small subgroup of tumors with locally pronounced “invasive growth” and a tendency to metastasize in the subarachnoid spaces.
Pleomorphic xanthoastrocytoma is a rare tumor (less than 1% of all astrocytomas), occupying an intermediate position in the series of “malignancies” due to its dual behavior (WHO-2). In some cases, the tumor is well demarcated and slowly growing with a favorable prognosis. At the same time, cases of its malignant transformation with an unfavorable prognosis have been described. Clinical picture. Most often, the tumor occurs at a young age and manifests itself as an episyndrome. Characteristic is a superficial subcortical localization and a tendency to involve the adjacent meninges in the pathological process (“meningo-cerebral” volumetric process). Diagnostics: CT/MRI. Treatment is surgical; the goal of the operation is “total removal” of the tumor, which is often achievable. Forecast. 5-year survival rate is 81%, 10 - 70%. An independent prognostic factor is increased (more than 5 mitoses in a high-power field) mitotic activity. Most tumors with an aggressive course are characterized by this indicator.
Abbreviations. GBM - glioblastoma
ICD-10 • D43 Neoplasm of uncertain or unknown nature of the brain and central nervous system • C71 Malignant neoplasm of the brain
Application. Genetic aspects • In astrocytomas, 2 types of damaged genes have been registered: •• dominantly inherited oncogenes, protein products of the gene accelerate cell growth; typical damage is an increase in the gene dose due to amplification or activating mutation •• tumor suppressors, protein products of the gene inhibit cell growth; typical damage is physical loss of a gene or an inactivating mutation • Mutations: •• TP53 gene (*191170, 17p13.1, Â) •• MDM2 (164585, 12q14.3–12q15, Â) •• CDKN1A (*116899, 6p, Â ) •• CDKN2A and CDKN2B (9p21) •• CDK4 and CDK6 (12q13–14) •• EGFR (*131550, 7, Â).
Where to get treatment: the best foreign clinics and doctors
Specialists from clinics in Israel and Spain achieve high success rates in the treatment of astrocytoma. The outcome of the operation largely depends on the accuracy of the manipulations and the experience of the neurosurgeon. Therefore, the main priority when choosing a clinic for treatment should remain the professionalism of the operating doctor.
Teknon Medical Center, Spain
Oliver Bartolome
– expert in the treatment of diseases of the nervous system, work experience – more than 35 years. The doctor specializes in minimally invasive surgery and functional neurosurgery. He is fluent in craniotomy and radiosurgery techniques and performs operations using a Cyber Knife.
Sourasky Medical Center, Israel
Professor Zvi Ram
– Head of the neurosurgery department of the clinic, heads the Society of Neurosurgeons of Israel.
The doctor has been performing brain surgery for more than 30 years, during which time he has developed and implemented many proprietary techniques. He is an expert in minimally invasive neurosurgical operations. Dr. Shlomo Constantini
heads the Department of Pediatric Neurosurgery.
In Israel he is known as one of the best neurosurgeons in the field of treating children and adolescents. Professor Nevo Margalit
is a senior neurosurgeon and heads the unit of skull base surgery at the Sourasky Medical Center. The doctor's narrow specialization is the removal of benign and malignant brain tumors, as well as operations on the base of the skull.
You can find out more information about the treatment of astrocytoma abroad, as well as organize a medical trip, by contacting the coordinating doctors of the international MediGlobus platform.
NeurosurgeryOncologyRehabilitation
Doctor Vadim Berezhnoy
Founder of the MediGlobus platform. Medical expert, Head of the department of coordinating doctors.
Nina Vorobey
Editor
She has been writing medical texts for more than 2 years. Experience in the field of copywriting exceeds 6 years. Has an education in the field of “Social and Legal Protection”. Completed the medical course program. Studies communication techniques for negotiating with patients. In his free time, he attends trainings and seminars on medical psychology.