General information
The Manual of Diseases of the Autonomic Nervous System defines paroxysms as paroxysmal manifestations of autonomic, emotional, behavioral and cognitive disorders over a relatively short period of time.
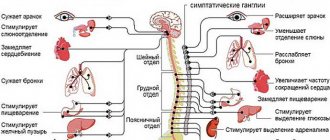
The autonomic nervous system regulates the functioning of internal organs, exocrine and internal secretion glands, lymphatic and blood vessels. The autonomous department of the nervous system is responsible for the activities of all organs and the system as a whole. The human will is unable to influence the work of the autonomic department. Absolutely all autonomic functions are subordinate to the central nervous system and, first of all, to the cerebral cortex.
Main functions of the vegetative department:
- regulation of metabolism , metabolism;
- regulation at the nervous level of all tissues and organs (with the exception of skeletal muscles);
- ensuring adaptive reactions;
- maintaining normal homeostasis in the body.
The structure of the vegetative region
Functionally and anatomically, the autonomic nervous system is divided into several sections:
- sympathetic;
- metasympathetic;
- parasympathetic.
Paroxysmal activity of the brain is the electrical activity of the cerebral cortex, in which an excess of excitation processes over inhibition processes is recorded in one of the brain regions. The paroxysmal state is characterized by a sudden, sharp onset, an extremely rapid course and an equally sudden end.
Paroxysmal disorders are divided into 2 types of paroxysmal activity:
- epileptic (associated with epilepsy);
- non-epileptic (associated with the autonomic department).
Periodic paralysis (paroxysmal myoplegia) is a neuromuscular pathology characterized by periodically triggered attacks (paroxysms) of transient paralysis .
Lifestyle of sick men and women
Thanks to the capabilities of modern medicine, epileptics can lead a normal life. However, he must follow some rules to prevent the development of a seizure:
- Avoid places with large crowds of people, climate changes, time zones.
- Avoid stress.
- Don't drink alcohol.
Do not stay in the sun for a long time, in a bathhouse, or a sauna, so as not to provoke overheating. Maintain a daily routine. Good sleep, alternating work and rest, and proper nutrition are important for the patient. Patients can play sports, but participation in competitions is prohibited.
As for pregnancy and childbirth, there is no clear opinion on this matter. According to statistics, 90% of women suffering from epilepsy normally carry and give birth to healthy children.
Absolute contraindications to pregnancy are:
- Frequent generalized attacks that are not amenable to drug treatment.
- Visible personality disorders of a woman.
- Epistatus.
In other cases, pregnancy is not contraindicated. Six months before conception, a woman should undergo a full examination and discuss pregnancy management tactics and possible risks with her doctor.
The issue of military service with this disease is relevant. Young people with epilepsy can be drafted into the army as Category B4 (fit with minor restrictions) if they are not taking anti-seizure drugs and have not had a seizure in the last five years.
In other cases, the conscript falls under category B and is transferred to the reserve.
Pathogenesis
The main role in the pathogenesis of paroxysms is played by autonomic imbalance , which occurs as a result of a violation of autonomic regulation. According to the widespread concept of Selbach, there is a kind of “swinging balance” between the parasympathetic and sympathetic parts of the nervous system: when the tone of one part increases, the activity of the other increases. Thanks to this balance, it is possible to maintain homeostasis and create certain conditions that ensure the lability of physiological functions.
Using the experimental method, it was possible to prove the lability of all systems: blood pressure, heart rate variation, temperature, etc. The autonomic system becomes vulnerable when these fluctuations go beyond the homeostatic range. Endogenous and exogenous stimuli overstrain regulatory systems, which leads to their breakdown, “disintegration” with special clinical symptoms in the form of vegetative paroxysms.
Classification
According to the flow it is customary to distinguish:
- paroxysmal vegetative-vascular dystonia (symptoms appear episodically, during paroxysms and attacks);
- permanent vegetative-vascular dystonia (symptoms are constantly present).
If there are signs characteristic of both types, then they speak of a permanent-paroxysmal course, in which paroxysms occur against the background of sluggish symptoms.
It is customary to distinguish several types of crises:
- Vagoinsular paroxysms . Characterized by a decrease in blood pressure, slowing or accelerating heart rate ( bradycardia / tachycardia ), dizziness , hyperhidrosis . Fainting is a type of vagoinsular paroxysm.
- Sympathetic-adrenal paroxysms . Characterized by hyperthermia , rapid heartbeat, increased blood pressure, chills-like hyperkinesis , pain in the heart area. Attacks usually end with the release of light-colored urine in a large volume.
- Mixed paroxysms . Combines the features of the two previous options. Symptoms can naturally replace each other. In a certain group of patients, crises occur only during the daytime, in others - at night.
Syndromes with vegetative-vascular dystonia VSD
With vegetative-vascular dystonia of VSD, various clinical syndromes are observed.
Autonomic dysfunction syndrome VSD
Autonomic dysfunction syndrome - combines sympathetic, parasympathetic and mixed symptom complexes of a generalized, systemic or local nature, manifesting permanently or in the form of paroxysms (vegetative-vascular crises), with non-infectious low-grade fever, a tendency to temperature asymmetry.
Sympathicotonia with VSD, sympathoadrenal crisis
Sympathicotonia in vegetative-vascular dystonia is characterized by tachycardia, pallor of the skin, increased blood pressure, weakened intestinal motility, chills, and a feeling of fear and anxiety . During a sympathoadrenal crisis , a headache appears or intensifies, numbness and coldness of the extremities, paleness of the face occur, blood pressure rises to 150/90-180/110 mm Hg. Art., the pulse quickens to 110-140 beats per minute, pain is noted in the heart area, agitation and restlessness appear, sometimes the body temperature rises to 38-39 degrees Celsius.
Vagotonia with VSD, vagoinsular crisis
Vagotonia pressure , and gastrointestinal dyskinesia. Vagoinsular crisis is manifested by a feeling of heat in the head and face, suffocation, heaviness in the head, nausea, weakness, sweating, dizziness, the urge to defecate, increased intestinal motility, miosis is noted, a decrease in heart rate to 45-50 beats per minute, and a decrease in blood pressure. up to 80/50 mm Hg. Art, allergic manifestations in the form of urticaria or Quincke's edema are possible.
Mixed crisis with VSD
Mixed crises in vegetative-vascular dystonia are characterized by a combination of symptoms typical of crises, or their alternate manifestation. There may also be red dermographism, zones of hyperalgesia in the precordial region, “spotted” hyperemia of the upper half of the chest, hyperhidrosis and acrocyanosis of the hands, tremor of the hands, non-infectious low-grade fever, a tendency to vegetative-vascular crises and temperature asymmetries.
Syndrome of mental disorders in VSD
The syndrome of mental disorders in VSD is characterized by behavioral and motivational disorders - emotional lability, tearfulness, sleep disturbances, feelings of fear, and cardiophobia. Patients with VSD have a higher level of anxiety, they are prone to self-blame, and experience fear in making decisions. Personal values prevail: great concern for health (hypochondria), activity decreases during illness.
Syndrome of adaptation disorders, asthenic syndrome with vegetative-vascular dystonia VSD
Syndrome of adaptation disorders , asthenic syndrome is characterized by rapid fatigue, weakness, intolerance to physical and mental stress, and weather dependence.
Hyperventilation (respiratory) syndrome with VSD
Hyperventilation (respiratory) syndrome is manifested by a subjective feeling of lack of air, chest compression, difficulty breathing, and the need for deep breaths. In some patients, it occurs in the form of a crisis, the clinical picture of which is close to suffocation. The most common reasons that provoke the development of respiratory syndrome are physical exertion, mental stress, staying in a stuffy room, sudden changes in cold and heat, and poor transport tolerance. Along with the mental factors of shortness of breath, a decrease in the compensatory and adaptive capabilities of the respiratory function to hypoxic loads is of great importance.
Neurogastric syndrome with VSD
Neurogastric syndrome by neurogastric aerophagia, esophageal spasm, duodenostasis, and various disorders of the motor-evacuation and secretory functions of the stomach and intestines. Patients complain of heartburn, flatulence, constipation.
Cardiovascular syndrome in VSD
Cardiovascular syndrome is manifested by cardialgia in the left half of the chest, which occurs during emotional stress, is accompanied by hypochondriacal disorders, is not relieved by coronary lytics, fluctuations in blood pressure, pulse lability, tachycardia, and functional murmurs are noted. ECG and bicycle ergometry most often reveal sinus and extrasystolic arrhythmias; there are no signs of myocardial ischemia.
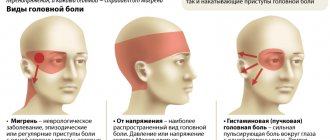
Syndrome of cerebrovascular disorders in VSD
The syndrome of cerebrovascular disorders is characterized by headaches, dizziness, noise in the head and ears, and a tendency to faint. Their development is based on cerebral angiodystonia, the pathogenetic basis of which is dysregulation of cerebral vascular tone of a hypertonic, hypotonic or mixed nature. In some patients with persistent cephalgic syndrome, there is a violation of the tone of not only arterial, but also venous vessels, the so-called functional venous hypertension.
Syndrome of metabolic tissue and peripheral vascular disorders in vegetative-vascular dystonia
The syndrome of metabolic tissue and peripheral vascular disorders is manifested by tissue edema, myalgia, angiotrophoneurosis, and Raynaud's syndrome. The development of this syndrome is based on changes in vascular tone and vascular permeability, disturbances in transcapillary metabolism and microcirculation.
Cardiac syndrome is the most common in vegetative-vascular dystonia (cardiac cardiac type of VSD)
Cardiac syndrome is the most common form. It is this that causes overdiagnosis of organic heart pathology, which in turn is fraught with serious consequences: excommunication from physical education and sports, warnings regarding pregnancy and childbirth, frivolous removal of tonsils, unnecessary prescription of thyreostatic, anti-inflammatory, antianginal and other drugs. Among the leading cardiac syndromes one should highlight: cardialgic, tachycardial, bradycardic, arrhythmic, hyperkinetic.
Cardialgic syndrome with VSD
Cardialgic syndrome occurs in 85% of patients with neurocirculatory dystonia . Cardialgia is associated with increased susceptibility of the central nervous system to interoceptive stimuli; experts regard it as sympathalgia. Once it occurs, cardialgia is fixed using the mechanism of autosuggestion or a conditioned reflex. The pain can be of a different nature: constant aching or pinching in the area of the apex of the heart, intense prolonged burning in the area of the heart, paroxysmal prolonged cardialgia, paroxysmal short-term pain or pain that occurs in connection with physical activity, but does not interfere with the continuation of the exercise. Stress and drug tests are undoubtedly helpful in making a diagnosis. When the terminal part of the ventricular complex changes on the ECG, a stress test in the case of functional cardialgia leads to a temporary reversion of the T wave, and in patients with coronary artery disease it is aggravated. Drug tests in the first case also lead to temporary reversion, but not in the second. Help is provided by invasive methods, lactate dynamics during atrial pacing.
Tachycardia syndrome
Tachycardia syndrome with vegetative-vascular dystonia is characterized by an increase in the automaticity of the sinoatrial node with an increase in the number of heartbeats to 90 or more per minute. The reasons for the development of this syndrome may be an increase in the tone of the sympathetic nervous system or a decrease in the tone of the vagus nerve. Sinus tachycardia significantly limits the physical performance of patients, as evidenced by testing with dosed physical activity. The heart rate reaches submaximal values for a given age even when performing low-power work of 50 - 75 W. With sinus tachycardia, the number of heart contractions at rest rarely exceeds 140-150 beats per minute.
Bradycardic syndrome
Bradycardia syndrome involves a slowing of heartbeats to 60 per minute or less due to a decrease in the automaticity of the sinoatrial node, caused by an increase in the tone of the vagus nerve. The criterion for sinus bradycardia should be considered a decrease in contraction frequency to 45 - 50 beats per minute or less. The bradycardic variant is less common. With more pronounced bradycardia, there may be complaints of headaches and precordial pain, dizziness with rapid extension of the body or transition to orthostasis, and a tendency to fainting and fainting states. A number of other signs of vagoinsular predominance are also identified: poor cold tolerance, excessive sweating, cold hyperhidrosis of the palms and feet, cyanosis of the hands with a marbled skin pattern, spontaneous dermographism. On the ECG, “giant” (“vagal”) T waves may appear in the precordial leads, more often in leads V 2 - V 4.
Arrhythmic syndrome with VSD
In patients with vegetative-vascular dystonia of VSD, as part of the arrhythmic syndrome , extrasystole is more common, supraventricular forms of paroxysmal tachycardia are less common, and paroxysms of atrial fibrillation or flutter are extremely rare. Experts differentiate rhythm disturbances in functional heart diseases from mild myocarditis (rheumatic and non-rheumatic), myocardial dystrophies, reflex effects on the heart (osteochondrosis, gallbladder pathology), hyperfunction of the thyroid gland.
Hyperkinetic cardiac syndrome VSD
Hyperkinetic cardiac syndrome is an independent clinical type of VSD . Like other cardiac syndromes, it is a centrogenically caused autonomic disorder. The final link in its pathogenesis is an increase in the activity of beta-1 adrenergic receptors of the myocardium against the background and due to sympathadrenal predominance. As a result, a hyperkinetic type of blood circulation is formed with a characteristic hemodynamic triad:
1) an increase in stroke and cardiac output, far exceeding the metabolic needs of tissues; 2) increasing the rate of blood expulsion from the heart; 3) compensatory drop in total peripheral vascular resistance.
Vegetative-vascular dystonia: treatment in Russia (treatment of VSD)
Sarklinik successfully uses complex methods for treating various types of vegetative-vascular dystonia (VSD) in adults, children and adolescents. As a result of therapy, the activity of the sympathoadrenal and cholinergic systems is normalized, the sensitivity of alpha and beta adrenergic receptors, the levels of hormones of the hypothalamus, pituitary gland, adrenal glands, acid-base balance, autonomic tone are restored, neurohumoral changes, pathological endocrine and neuroallergic reactions are eliminated, permanent autonomic disorders are stopped, correction of neurotic disorders that occur during the course of the disease occurs.
Treatment of vegetative-vascular dystonia VSD in Saratov, VSD treatment in Russia
The effectiveness of complex treatment of VSD (vegetative vascular dystonia), which can include a variety of reflexology, acupuncture, microacupuncture, moxibustion, alternative methods, acupuncture, reaches 98% and depends on the characteristics of the disease, the severity of dystonia, the duration of the disease, and associated factors. Treatment of VSD, NCD (nephrocirculatory dystonia, vegetative vascular dystonia) is carried out on an outpatient basis and individually. All methods are safe. Sarclinic has been operating for many years, during which time hundreds of patients have been cured of vegetative-vascular dystonia - men and women, adults and children.
Causes
Paroxysms are most often just a manifestation of certain diseases. Paroxysms may be a reflection of dysfunction of the autonomic nervous system.
Paroxysms are triggered against the background of neuroses and some organic brain lesions:
- dysfunction of the vestibular apparatus;
- hypothalamic disorders.
In some cases, attacks accompany migraine and temporal lobe epilepsy. They induce paroxysmal affect and allergic reactions .
Symptoms of diseases of the autonomic nervous system
Sympatho-adrenal paroxysms are characterized by a sudden onset, without warning signs. Most often, an attack occurs after a sleepless night or overstrain (emotional, physical, mental). Main manifestations:
- pale skin;
- mydriasis;
- polyuria;
- trembling, chills in the body;
- dry mouth;
- cold extremities;
- hyperglycemia (rare).
The paroxysm begins and ends with pronounced disturbances in the functioning of the cardiovascular system (instability of blood pressure, tachycardia , shortness of breath ). The patient recovers from paroxysm slowly, over several hours.
Vago-insular paroxysms are characterized by:
- labored breathing;
- drop in blood pressure ;
- feeling of lack of air;
- lethargy;
- hypoglycemia;
- nausea;
- disturbances in the digestive tract;
- hyperhidrosis;
- drowsiness.
Patients quickly recover from paroxysm and recover from the attack. During the first two hours after a crisis, there may be adynamia , drowsiness , sweating and vasomotor disorders.
In the mixed form, symptoms characteristic of the two attacks described above are recorded. The hypothalamic origin of attacks is determined by such manifestations as:
- polyuria;
- bulimia;
- hyperthermia.
In the interictal period, endocrinological diseases and neurotic symptoms can be recorded. Mild neurological symptoms include:
- sluggish abdominal reflexes;
- anisoreflexia;
- asymmetry of nasolabial folds;
- anisocoria.
The behavioral status of the patient during an attack depends on his social appearance, culture and personality structure. Each patient has a different severity of autonomic disorders. Some people experience a deepening of neurotic symptoms during and after a paroxysm. With hypothalamic dysfunction (dynamic and morphological form), sympathetic-adrenal paroxysms are more often recorded and mixed paroxysms are extremely rare.
What is autonomic paroxysm?
Vegetovascular paroxysms are clinical manifestations of dysfunction of the autonomic nervous system (ANS). They are expressed by a sharp deterioration in the patient’s condition with progression of leading symptoms.
Many people ignorant of medicine believe that the types of paroxysms cannot be distinguished without the use of specialized and highly accurate diagnostic methods.
But this is not so, and in most cases an experienced doctor immediately sees what he is dealing with.
Definition of paroxysms
Vegetative-vascular paroxysms are a collective concept that includes all the sudden changes in the functioning of the ANS. They manifest themselves as a complex of symptoms.
The main features of such attacks:
- Suddenness. Pathology occurs without warning and quickly increases after the influence of a provoking factor.
- Emotional dependence. Most paroxysms progress after strong experiences (both positive and negative).
- Functional character. Seizures are manifestations of a disorder in the functioning of the ANS and its structures. When their functions are normalized, the problem goes away.
A synonym for vegetative-vascular paroxysm is crisis. There are several options for the development of the clinical picture against the background of different manifestations of specific pathological reactions. In each case, the characteristics of the symptoms are noted, on the basis of which they are differentiated.
- Paroxysms are characteristic mainly of young patients. In older people, they occur much less frequently due to sclerotic changes in the body and a decrease in the overall ability to quickly mobilize. The vessels lose their elasticity and cannot expand or contract quickly enough to cause a crisis.
- Women get sick more often than men. This is noticeable during menstruation and pregnancy - a hormonal imbalance occurs, which further aggravates the malfunction of the ANS.
Mechanism of occurrence
Functional abnormalities in the functioning of the hypothalamus and peripheral parts are secondary in nature and disappear after the provoking factor is eliminated.
Sometimes the cause of crises is organic damage to the structures of the ANS (tumor, infection, injury), which aggravates the course of the disease. In this case, the diagnosis of VSD is not made, since crises are caused not by an imbalance, but by organic pathology, and are no longer the main condition, but a secondary manifestation.
Depending on which department of the ANS (sympathetic or parasympathetic) predominates, the functioning of specific organs is enhanced or weakened. Traditionally, the following are affected by paroxysms:
- heart;
- vessels;
- nervous system;
- endocrine glands.
During a sharp activation of the ANS, a sudden manifestation of the main manifestations of the disease occurs. For some, this will result in a hypertensive crisis, while others fall into depression.
Types of paroxysms
Depending on the symptoms, they are divided into the following types:
- sympathoadrenal;
- vagoinsular;
- mixed.
The first group includes sudden deterioration of the condition, which is caused by activation of the sympathetic division of the autonomic nervous system.
- People with such paroxysm are anxious, irritable, and sometimes even aggressive.
- Their blood pressure rises, headaches appear, their skin turns pale, and their pupils dilate.
Sedatives have worked well in treatment.
Vagoinsular vegetative-vascular crisis progresses against the background of hyperactivation of the parasympathetic part of the nervous system. Because of this, inhibition of most internal reactions is observed:
- the person is gloomy;
- his blood pressure drops;
- there is sweating, the urge to have a bowel movement, nausea and vomiting;
- pupils constrict;
- heartbeat becomes rare.
The mixed type combines the features of the two options above. It indicates a pronounced imbalance in the functioning of the ANS with constant activation of one or another of its departments.
They are classified according to severity as follows:
- Lungs. They last 10–20 minutes and go away on their own without the use of medications.
- Average. Lasts up to one hour. They manifest themselves as severe symptoms with a noticeable decrease in performance.
- Heavy. The patient is disturbed for more than 60 minutes. Accompanied by pronounced signs of autonomic dysfunction with a strong deterioration in well-being. Elimination requires the use of specialized medications.
Nocturnal paroxysms
Nocturnal paroxysmal dystonia is a separate type of vegetative attacks that does not fit into the traditional classification. Unlike other forms of pathology, the causes of its origin are still unknown.
The problem manifests itself as episodes of chaotic motor activity involving the limbs and the whole body after waking up.
Clinically, nocturnal paroxysm of dystonia resembles an epileptic seizure, but with normal electroencephalography (EEG) readings.
It is believed that the reason for the appearance of such movements is the loss of inhibitory mechanisms in the brain stem. Normally, they interfere with human muscle activity during sleep. The pathology is manifested by characteristic seizures. The average episode length is 10–60 minutes. Treatment has not yet been developed.
Symptoms
The clinical picture of paroxysms caused by dysfunction of the ANS varies depending on the predominance of its specific part.
Typical symptoms of sympathoadrenal crisis:
Patients with sympathoadrenal paroxysm suddenly turn purple, and convulsions may even occur. They tend to express emotions too strongly (screaming, crying).
The vagoinsular variant is characterized by a predominance in the regulation of the peripheral organs of the parasympathetic division of the ANS. Classic symptoms of such paroxysm:
- Deterioration of mood. The person is apathetic, whiny, and does not want to communicate with other people.
- Bradycardia. Functional arrhythmias progress.
- Breathing problems. Shortness of breath, lack of air, and compression of the lungs appear. Some people note the presence of a non-existent obstruction in the bronchi that prevents them from breathing normally.
- Blood pressure drop. In severe forms of paroxysm, a person may even faint. The main danger remains the risk of injury from a fall or progression of symptoms while performing work or driving.
- Discomfort throughout the body. A person is often unable to determine where it hurts. The unpleasant sensation is aching in nature, occurs frequently, and is mildly expressed.
The mixed form of paroxysm is manifested by a combination of the above symptoms with varying degrees of severity.
Features of the flow
Treatment of vegetative paroxysms is complex. It is carried out using both specialized drugs (mainly affecting the functioning of the ANS) and non-drug methods:
- acupuncture;
- aromatherapy;
- physiotherapy;
- meditation.
By fixing the factor that provokes the appearance of the next paroxysm, with its further elimination, it is possible to normalize the person’s condition.
It is possible to completely eliminate the occurrence of attacks by normalizing the balance between the branches of the autonomic system and increasing the threshold of excitability of the nervous system.
Source: https://urokrisunka.ru/info/vegetativnyj-paroksizm-chto-jeto/
Tests and diagnostics
It is extremely important to make a differential diagnosis between paroxysm of the autonomic nervous system and diencephalic (hypothalamic) epilepsy or other hypothalamic . In some cases, this can be extremely difficult; several factors and circumstances must be taken into account.
During hypothalamic epilepsy, convulsions are observed and loss of consciousness occurs (even short-term). Epileptic seizures are characterized by frequent and short repetitions, usually at night. They are not associated with overwork or overstrain.
Electroencephalography is important in differential diagnosis. In individuals with hypothalamic epilepsy, EEG in the interictal period reveals specific changes in the form of epileptic discharges in the oral part of the brain stem. The described electroencephalographic criterion is considered the main one for confirming hypothalamic epilepsy .
To establish the exact nature of a vegetative attack (epileptic or non-epileptic), the doctor also needs to study the patient’s behavior after the attack, understand the patient’s personality, and get to know his family to identify “minor” epileptic signs.
Autonomic paroxysm may occur as a result of involvement of the limbic system in temporal lobe epilepsy and be an aura. In such cases, attacks are stereotypical, short-lived and often manifest as isolated disturbances of any visceral function. Also, the diagnosis of vegetative attacks requires the exclusion of pathology of internal organs (especially in the heart). It is important to exclude hysteria and arterial hypertension .
Diagnosis of symptomatic epilepsy
With symptomatic epilepsy, there is always a complicated history, that is, by asking the person carefully, you can find many clues for yourself. Such individuals always have some kind of trauma, illness, surgery, addiction or something similar in their past. You can find obvious signs of this, such as scars, needle marks. In the children's age category, the presence of nuances during childbirth or in the postpartum period
It is important to distinguish this disease from others with the presence of seizures. Epilepsy has a sudden onset of seizure, but may initially have an aura that serves as something of a warning sign
External causes of the onset of a seizure cannot be detected. But it can be provoked by certain triggers, for example, stopping anticonvulsant treatment, sleep deprivation, and drinking alcohol. Also less massive, but more frequent due to their distribution, can be temperature, allergens, sharp irritants, sound, aromatic, stress, excitement, excessive intake of liquid or sugar substances.
Before the onset of symptomatic epilepsy itself, pathologies of its series may appear: migraines, night terrors, apnea, enuresis. Also, typical signs of an epileptic seizure include an aura, a fall, regardless of the location, if it is a grand mal seizure. During convulsions, the face changes color, first turns pale, then becomes cyanotic. The pupils do not react to light during an attack, and patients often bite their tongues. During the examination, they even ask to show your tongue, because the presence of scars confirms the presence of epilepsy. Very often there may be bowel movements against the person's will. The seizures are photographically similar, that is, one is similar to the previous one. The seizure has a clear sequence: first loss of consciousness, then fall, tonic, then clonic convulsions, coma, stupor, stun. Characterized by acute episodic oligophasia, absolute loss of awareness during an attack. Amnesia after the attack is complete. The duration of the attack is from half a minute to two minutes. Pyramid symptoms may occur.
A complete psycho-emotional and medical examination includes the collection of information, the patient’s life history, medical history
With epilepsy, it is very important to describe seizures, because this gives the person the right to have a disability group. A general somatic and neurological examination and an indicative EEG are required.
Typical EEG patterns will be sharp peak waves and slow waves. Some neurological examinations also include MRI to identify lesions. The purpose of the examination is to identify the causes. You also need to look for mental disorders, which are often associated. To do this, we use conversation, as well as psychiatric questionnaires: Moko, MMSE, scales and determination of intelligence.
Prevention, how to strengthen the autonomic nervous system?
Patients prone to paroxysms should be more attentive to their own health, listening to all symptoms and changes in the functioning of the body. Following simple recommendations will strengthen the autonomic nervous system and avoid paroxysms (or reduce their number as much as possible).
- Start your day with a contrast shower. A light morning manipulation will not only improve your well-being and mood, but also replenish your energy supply. For a beginner, it is enough to splash yourself with cold water after taking a shower. Taking a pine bath before bed has a good effect, which ensures maximum relaxation.
- Complete cessation of smoking and drinking alcoholic beverages. Nicotine promotes vascular spasm, and alcohol negatively affects the functioning of the nervous system.
- Take vitamin complexes in courses. Vitamin A , B vitamins , as well as ascorbic acid ( Vitamin C ) have a positive effect on the functioning of the nervous system.
- Do yoga. Relaxing technique normalizes the functioning of the autonomic nervous system
- Walk outdoors regularly.
Stress protectors help prevent paroxysms. It is for this purpose that daytime tranquilizers are prescribed. Anticonvulsants, some neuroleptics, antidepressants and benzodiazepine tranquilizers are prescribed to correct the patient’s psycho-emotional state. The above drugs have a positive effect on the “stagnant” circulation of nerve impulses and areas of increased excitability.
Antidepressants have sedative, thymoanaleptic and anxiolytic effects, block the reuptake of serotonin and norepinephrine .
Psychotherapy also helps to correct the patient’s psycho-emotional state and change personal attitude towards traumatic factors.
How to live with a disease
Patients with ES can easily live a normal life without feeling inferior. To prevent an attack, you must follow some recommendations:
- Beware of overheating and strong temperature increases.
- Stick to a low-carb diet.
- Eat less spicy and salty foods.
- Do not drink tonic drinks (tea, coffee, energy drinks).
- Quit alcohol and smoking.
- Avoid stressful situations.
With frequent convulsive seizures, patients cannot perform their work duties and receive a disability group.
If attacks occur rarely, the patient can work, but there are a number of activities that are contraindicated for this disease.