This neuroinfection is transmissible. It primarily affects the brain matter. Differs in seasonal character. Outbreaks are recorded from August to the end of September. The onset has no characteristic symptoms and is general infectious. In the acute period, it is accompanied by meningeal syndrome, disorders of consciousness, hyperkinesis, paresis, myoclonus, and bulbar disorders. To make a diagnosis, it is necessary to perform a lumbar puncture and RIF. ELISA. A PCR study is also indicated. For treatment, serum or specific immunoglobulin is used. Corticosteroid, decongestant, vascular, detoxification, and anticonvulsant drugs are prescribed as symptomatic therapy.
Classification
The disease is more common in certain climatic zones - Southeast Asia, Thailand, India, Primorsky Krai, and the south of the Far East. In warm countries, the activity of the virus is higher, but most local residents have stable immunity to the pathogen. Differences in symptoms among different people are explained by the characteristics of their body.
The following forms of JE are distinguished:
- asymptomatic – up to 3 weeks after infection;
- febrile form - lasts about a week;
- aseptic meningitis - characterized by inflammation of the meninges;
- encephalitis.
Each form is characterized by mild, moderate and severe course.
Seasonality of the disease
Outbreaks of JE incidence are typical for the subtropics and areas with a warm temperate climate. Such areas include some northeastern provinces of China, Japan, and the southern regions of the Far East and Primorye. At an average temperature above +20 degrees, long-term epidemics (40-50 days) occur more often. The maximum number of cases is observed in August and September - during the hottest period. In countries with warm climates, surges in incidence are recorded all year round.
Everyone is susceptible to JE. However, the virus poses varying degrees of danger to residents of different regions. For example, in areas with an increased risk of infection (endemic), in most patients the infection develops latently. The ratio of overt to asymptomatic cases ranges from 1:25 to 1:1000. Most of the population in these areas is immune to the disease. People who have had it develop lifelong immunity.
Among residents of endemic areas, children aged 3-15 years are more susceptible to the effects of the virus. The risk of infection is also higher for visitors from other regions. In most people who have moved, antibodies to the causative agent of Japanese encephalitis can easily be detected during examination after 5-6 years of living in a new place. During disease outbreaks, representatives of all groups of the population become ill, regardless of age. The risk of infection is higher for residents of rural areas, especially for fishermen, hunters and farmers, who are often attacked by blood-sucking insects.
History of discovery and study
The disease has a centuries-old history of origin. It was first identified in Japan in 1924, when an infectious outbreak killed a large number of people. Of the 7,000 infected, only 20% survived.
After research conducted by Japanese scientists, the diagnosis was confirmed - Japanese encephalitis. Later it was called summer encephalitis, mosquito encephalitis B, and autumn mosquito encephalitis.
The final name of the complex neuroinfection was fixed in the form of the term “Japanese encephalitis”.
After identifying the ability of encephalitis to occur in various natural centers, scientists concluded that it is spreading not only in Japan, but also in the Pacific countries.
Residents of Russia were also at risk: in 1938, it was described by Russian researchers in the territory of Southern Primorye.
Symptoms
The incubation period for Japanese encephalitis lasts from 4 to 21 days. The first symptoms include increased fatigue, drowsiness, and sometimes speech and vision disturbances. After 2 days, general infectious symptoms rapidly develop:
- chills;
- headache;
- temperature rise up to 41 degrees;
- muscle pain;
- discomfort in the lumbar region;
- nausea with vomiting;
- increased sweating;
- unsteady gait, frequent loss of balance.
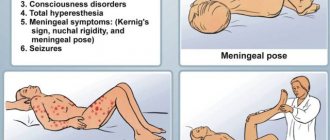
The heartbeat becomes less frequent, and after a few hours it increases. After 3-4 days of development of the disease against the background of infectious-toxic syndrome, the activity of the central nervous system (CNS) is disrupted. This stage is characterized by serious disturbances of consciousness - the person loses control over his behavior, becomes delusional, and becomes absent-minded. The mortality rate of Japanese encephalitis reaches 70% in the first 7 days of the disease.
In 50% of cases, the patient develops signs of psychosis with emotional and motor agitation. Convulsive attacks or meningeal syndrome develop - damage to the membranes of the brain. Sometimes a person falls into a state of coma (complete insensibility).
When moving, the tremor (shaking) of the limbs increases or short contractions of large muscles occur. Among the main symptoms is pathological drowsiness. Increased muscle tone does not allow the patient to relax during sleep, as a result of which he takes forced positions. The occipital and chewing muscle fibers are constantly tense, which can cause paralysis - loss of the ability to function normally.
In severe cases, the patient experiences epileptic seizures and stereotypy of movements occurs - a persistent repetition of the same action. Changes in motor activity occur during the decline of the acute period of encephalitis.
The course of the disease is quite bright - the fever lasts from 7 to 10 days. Symptoms are most pronounced on days 3-5 of encephalitis development. During this period, the disease is complicated by infectious-toxic shock, inflammation and pulmonary edema, or blood poisoning. On days 6-7, the symptoms subside, but the recovery process takes another 1.5-2 months. The state of powerlessness persists for a long time. When pregnant women become infected, the risk of spontaneous miscarriage increases.
During the recovery period, the following complications may appear:
- nephropathy – kidney disease;
- infectious myocarditis – this is the name for inflammation of the heart muscle;
- the formation of bedsores - dead areas of soft tissue as a result of prolonged positioning of the body in one position;
- cystitis.
The consequences of Japanese encephalitis pose a danger to health and life, so if you want to visit an endemic area, you should protect yourself as much as possible by preparing special things and means of protection against insects.
In children
With the development of mosquito encephalitis in children, the nutritional method of transmission of infection is important. That is, a small child becomes infected through certain food products. Most often, children suffer from brain damage.
The brain is responsible for some body functions. Children are characterized by disturbances in consciousness. Up to the development of delusional states and states accompanied by hallucinations.
In children, the disease can be suspected if there is a persistent clinical picture. Most often, the disease is detected in children in the following cases:
- the child shows passivity;
- asthenic conditions of the child;
- the child's movement is impaired;
- body temperature rises;
- fever;
- Strong headache.
All these symptoms reflect a severe picture of the disease. After all, mosquito encephalitis is a persistent disorder in the body’s systems. This disease can cause death in infants.
Mortality is increased in children in the absence of proper treatment. Therefore, in areas of epidemic risk, it is necessary to vaccinate children. This also applies to adults. It is better to prevent a disease than to cure it!
go to top
Transmission routes
Japanese encephalitis is transmitted transmissibly through mosquitoes of the genus Culex and Aedes. The assumption of transmission of the virus through insects of the genus Anopheles is questionable. The route of transmission of the virus to humans is through mosquito saliva during blood sucking. People do not act as sources of infection, since the intensity of spread of the virus throughout the body is low.
A mosquito infected with a pathogenic microorganism retains the pathogen within itself for a long time. The pathogen accumulates in the insect's body, which makes the mosquito a more dangerous carrier. Females can live more than 3 months.
The virus does not persist in the body of overwintered mosquitoes. Typically, episodes of epidemic formation are associated with the introduction of the infectious agent by migratory birds. Despite the focal prevalence of the disease, it affects not only people who find themselves far from populated areas. Even in populated areas and cities there is a risk of becoming infected with JE.
Lifespan
With mosquito encephalitis, life expectancy depends on the course of the disease. With a protracted course of a hidden nature, life expectancy decreases. The treatment process also influences life expectancy.
Only properly selected therapy allows us to talk about the improvement of the patient’s condition. And also about increasing life expectancy. In severe brain disorders, loss of ability to work may occur.
Disability reduces quality of life. As a result, a person may experience great anxiety about their condition. And these neurotic disorders caused by this anxiety reduce life expectancy!
Pathogenesis
With increased virulence of the pathogen (ability to infect) or with a large number of viral agents, some of them are destroyed at the point of entry into the body. The remaining particles end up in the blood and spread to different organs. The virus can spread along nerve trunks.
After spreading throughout the body, the pathogen ends up in the kidneys, lungs, liver and spleen. The disease is asymptomatic when most of the viral agents die in the blood. If surviving microorganisms multiply and accumulate in tissues, a second wave of disease occurs with pronounced clinical manifestations.
Description of the viral agent
The causative agent of Japanese encephalitis is Japanese encephalitis virus. JEV is common in Australia, Southeast Asia, America and Africa. Related viruses are found on most continents.
Japanese Encephalitis Virus (JEV)
The pathogen has a diameter of 40-50 nm. Many rodents, birds and monkeys are very sensitive to the virus. JEV is inactivated (neutralized) when heated to +60 degrees for half an hour and to +70 degrees for 10 minutes. When boiling, inactivation occurs after 2 minutes. The causative agent of the disease dies in acetone or alcohol after 3 days.
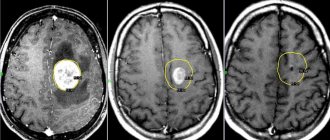
Diagnostics
Japanese encephalitis can be identified through differential diagnosis with tuberculous meningoencephalitis and other encephalitis of viral origin. JE is differentiated from malaria and typhoid fever. The pathogen is easier to find in the blood during a febrile period. It is also found in the cerebrospinal fluid during neurological disorders (in this case the prognosis is unfavorable).
The main method for determining infection is polymerase chain reaction (PCR). This diagnostic method is hypersensitive to the genetic material of many pathogens, which makes it possible to accurately determine the disease. Antibodies produced by the immune system to fight the virus remain in the cerebrospinal fluid for several weeks after the onset of the disease. They remain in the blood for up to several months. When deciphering data from serological studies (search for antibodies in blood serum), it is easy to confuse mosquito viral encephalitis with other flavivirus infections.
Recognition of the causative agent of the disease is based on a combination of laboratory data and clinical manifestations. The doctor takes into account the acute development of encephalitis, the severity of symptoms and the patient’s location several weeks before the onset of symptoms. Diagnosis is carried out as quickly as possible in order to prescribe effective treatment if the disease is confirmed.
Diagnosis methods
The first signal for diagnostics should be the presence of a person during an epidemic in an area that is a risk zone. If at this time a person was bitten by a mosquito, then diagnosis must be carried out immediately.
In Russia, cases of the disease are usually detected at the end of August and before the onset of cold weather in Primorye regions.
A reliable way to determine infection is a blood serum test. It notes the presence of specific antibodies. The most effective is the study of paired sera.
The first sample is taken at the very beginning of the onset of the disease, and the second - after 3-4 weeks. By the end of the first week, you can observe the body's reaction. Titles increase over time. A fourfold increase in titers is considered a positive result.
In addition to this type of diagnosis, hemagglutination suppression and neutralization reactions can be used. The PCR method is also used.
Japanese mosquito encephalitis affected area
Treatment
There is no medicine that can kill the virus. Therapy is aimed at alleviating clinical symptoms. The main measure to combat Japanese encephalitis is timely vaccination.
Therapy of the disease is divided into specific and pathogenetic. In the first case, treatment agents are used at the initial stage - when the first signs of fever appear:
- the patient is administered immunoglobulin three times a day, 3-6 ml;
- 15-20 ml of hyperimmune serum is administered in the first week after the onset of symptoms.
Pathogenetic therapy means include:
- detoxification agents – designed to remove toxic substances from the body;
- diuretics aimed at intensive urine excretion;
- corticosteroids – hormones with anti-inflammatory effects;
- sedative medications – used to calm and reduce emotional arousal;
- anticonvulsants.
If the patient has impaired respiratory or cardiac activity, he is placed in intensive care. Recovering patients require a long period of hospital stay and observation by a psychiatrist.
Prevention
Means of prevention are divided into means of general and individual prevention. The general prevention of Japanese encephalitis includes a number of specific sanitary and hygienic measures aimed at reducing or completely eliminating the possibility of mosquito attacks on people. These include irrigation measures to drain swamps and wetlands, chemical treatments with various chemicals leading to the destruction of mosquitoes. Processing, mechanical and chemical, is carried out on livestock, horses, pigs, goats and cows.
In terms of personal prevention, mechanical protection against mosquitoes is widely used, that is, wearing clothing and masks with appropriate chemical impregnation and repellent chemicals.
An active means of personal prevention of Japanese encephalitis is vaccination.
The information presented in this article is intended for informational purposes only and cannot replace professional advice and qualified medical care. If you have the slightest suspicion that you have this disease, be sure to consult your doctor!
Vaccination
Vaccination against Japanese encephalitis is the main method of protection for people planning to visit Asian countries or areas with warm climates.
There are 4 types of vaccines:
- inactivated – the drug contains parts of inactive pathogens;
- grown in rodent brain tissue;
- artificially recreated in culture of Vero cells - kidney epithelium of the African green monkey;
- live recombinant vaccine (obtained by cloning cells) and attenuated vaccine (the preparation contains a live, but not dangerous pathogen).
The vaccine is given 6-8 weeks before visiting Asian countries. During this time, the body will have time to produce antibodies to the virus. In China, the live attenuated vaccine has become widespread - it is administered to children according to standard methods. It is important to undergo an examination to ensure that the vaccination does not cause an allergic reaction.
Modern vaccines against Japanese encephalitis are inactivated preparations containing particles of killed pathogenic microorganisms. They are usually obtained from primary hamster kidney cells and African green monkey kidney connective tissue. Some drugs are being developed only in certain countries.
Global demand for vaccines is increasing every year. Many Asian countries have introduced an immunization schedule for children over one year of age.
The standard vaccination regimen includes three doses of the drug with an interval of 1 week, and then every 21 days. With an accelerated schedule, the third vaccine is administered to a person a week after the second. Thanks to the action of the first 2 vaccines, the body is protected in 80% of cases. The last time the vaccine is usually administered 10 days before visiting the endemic zone. Revaccination is carried out every 2-3 years. If you plan to live in an endemic zone for less than a month, vaccination is not carried out.