The essence of the problem
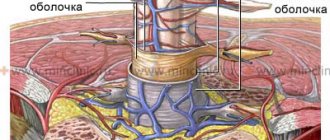
In some diseases, excess fluid appears in the cells and intercellular space of the spinal canal - this is spinal cord edema.
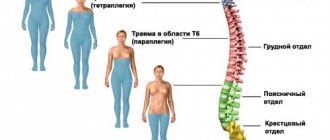
The phenomenon is accompanied by compression of nerve fibers, which leads to the following symptoms:
- Pain below the swollen area of the spine;
- Muscle stiffness or paralysis (the pupil may not respond to light);
- Failure of hematopoietic and immunogenerating functions;
- Dysfunction of the large and small pelvic organs;
- Involuntary defecation and urination or, conversely, their retention;
- Impaired breathing and circulation;
- Increased intracranial pressure (accompanied by headache and nausea).
The closer to the brain the damaged vertebra is located, the more serious the consequences of swelling will be.
The phenomenon is caused by several reasons and, depending on this, several types of spinal cord edema are distinguished.
Manifestations and symptoms of cerebral edema
It should be noted that usually the clinical picture with such a process is almost always the same, regardless of the pathogenesis. It usually consists of three groups of symptoms - stem, focal and intracranial hypertension syndrome.
Stem symptoms can manifest themselves as circulatory and respiratory disorders, and depression of pupillary response is observed. Symptoms of this type are life-threatening.
But first of all, it is the intracranial hypertension syndrome that manifests itself, which develops due to a rapid increase in the amount of fluid in the plane of the skull, which is a closed space, which means that there is an increase in fluid pressure on the brain, which is manifested by a characteristic headache that feels like it is “bursting.” » skull from the inside. Such pain is accompanied by nausea and vomiting, which occurs at moments of greatest intensity of pain, and the level of consciousness decreases. If intracranial hypertension exists for a long enough time, then it becomes clearly visible on radiographs - osteoporosis of the dorsum sella, increased digital indentations, etc. are noted.
Focal symptoms appear in cases where edema is localized in certain areas of the brain, which disrupts their work and eliminates the functions provided to them.
Trabecular edema of the vertebrae
Trabeculae are a bone frame found in various tissues of the body. This element is also present in the spongy bone tissue inside the vertebrae. This fabric is necessary to soften the shock loads on the spine during falls and jumps.
Trabecular edema develops as follows:
- Spongy bone tissue is damaged for one reason or another;
- Damage to spongy tissue leads to damage to the blood vessels that penetrate it. Injury to the capillary wall is accompanied by aseptic (microbial-free) inflammation and bleeding into the cancellous bone tissue;
- The body responds to this by releasing tissue fluid with protective proteins and leukocytes into the vertebra. They eliminate damaged spongy tissue and instead form a scar from connective tissue;
- Scar formation leads to swelling of the spinal cord.
Trabecular edema is caused by the following reasons:
- Osteochondrosis: age-related changes lead to a predominance of destruction processes in cartilage tissue over regeneration processes. The intervertebral disc becomes thinner, scars and then the scar turns into a callus. As a result, the cartilage partially loses its ability to perform a shock-absorbing function, which leads to an increase in the load on the spongy bone tissue of the vertebra. It is destroyed in places and then the mechanism already described above takes place, ending with bone marrow edema. A characteristic feature of edema in osteochondrosis is its superficial location;
- Trauma: Damage to spongy tissue also occurs with a compression fracture of the spine. It consists of crushing a vertebra with subsequent destruction of spongy tissue and hemorrhage into it. Traumatic edema differs from others in its pronounced symptoms: pain, severe inflammation at the site of the injury and adjacent tissues (the body replaces coagulated blood and damaged areas of bone with scar tissue), increased temperature. The fracture may be invisible and then it is detected precisely by bone marrow edema.
With minor injuries (contusions), contusional edema occurs.
Vasogenic edema
This type of edema is caused by blood leaking through the walls of blood vessels when the permeability of the latter is impaired.
A common cause of vasogenic edema of the bone marrow of the spine is an infectious inflammatory process in the body. The following happens:
- Individual microbes in minute quantities are spread by blood to various tissues, including the spongy tissue of the vertebrae;
- The immune system, occupied by the main focus, initially ignores them, which gives the microbes the opportunity to begin reproducing;
- The immune system is already reacting to this: inflammation begins, during which leukocytes destroy hostile cells;
- The foreign substances formed in this case create holes in the walls of blood vessels and the liquid component of the blood with a large amount of proteins enters the spongy tissue. Following this, fluid leaks here in a large volume - swelling of the bone marrow occurs.
Causes
The exact causes of tumor formation in the human body are unknown, but there are a number of factors that can trigger the development of the disease.
These include:
- exposure to large doses of ionizing radiation;
- bad habits (alcohol abuse, smoking);
- hereditary predisposition - if close relatives have had spinal cord tumors, this sharply increases the risk of developing this pathology in their descendants;
- work in hazardous production;
- age - the older a person gets, the higher the risk of developing a tumor.
Perifocal edema
This phenomenon consists of the cells being pushed apart by the accumulating liquid. Its sources are damaged glial cells. But fluid is not the only cause of edema: a large amount of plasma proteins can also enter the white matter of the brain, which can form connections with the glial elements of the brain. This phenomenon leads to a further increase in the volume of liquid.
Tumors develop in the area of lesions up to 10 mm in size.
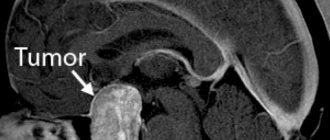
Spinal cord tumors
In the clinic of spinal neoplasms, 3 syndromes are distinguished: radicular, Brownsekar (the transverse of the spinal cord is half affected) and complete transverse lesion. Over time, any tumor of the spinal cord, regardless of its location, leads to damage to its diameter. However, the development of symptoms as the intra- and extramedullary tumor grows is markedly different. The growth of extramedullary formations is accompanied by a gradual change in the stages of radicular syndrome, Brownsecar syndrome and total damage to the diameter. In this case, damage to the spinal cord in the initial stages is caused by the development of compression myelopathy, and only then by tumor germination. Intramedullary tumors begin with the appearance at the level of formation of dissociated sensory disturbances of a segmental type. Then, gradually, complete damage to the spinal diameter occurs. The radicular symptom complex occurs in the later stages, when the tumor spreads beyond the spinal cord.
Radicular syndrome is characterized by intense pain of the radicular type, aggravated by coughing, sneezing, tilting the head, physical work, and straining. Usually the pain increases in a horizontal position and eases when sitting. Therefore, patients often have to sleep half-sitting. Over time, the pain syndrome is accompanied by segmental loss of all types of sensory perception and a disorder of reflexes in the area of innervation of the root. When percussion of the spinous processes at the level of the spinal tumor occurs, pain radiates to the lower parts of the body. The onset of the disease with radicular syndrome is most typical for an extramedullary tumor of the spinal cord, especially for neuroma. Such a manifestation of the disease often leads to errors in the primary diagnosis, since radicular syndrome of tumor genesis cannot always be clinically differentiated from radiculitis caused by inflammatory changes in the root due to infectious diseases and pathology of the spinal column (osteochondrosis, intervertebral hernia, spindyloarthrosis, scoliosis, etc.) .
Brown-Séquard syndrome is a combination of homolateral central paresis below the site of spinal cord lesion and dissociated sensory disorders of the conduction type. The latter include loss of deep types - vibration, muscle-articular - sensitivity on the side of the tumor and a decrease in pain and temperature perception on the opposite side. In this case, in addition to conductive sensory disturbances on the affected side, segmental disorders of surface perception are noted.
Total damage to the spinal diameter is clinically manifested by bilateral conductive loss of both deep and superficial sensitivity and bilateral paresis below the level at which the spinal cord tumor is located. There is a disorder of pelvic functions, threatening the development of urosepsis. Vegetative-trophic disorders lead to the development of bedsores.
Reactive edema
Appears as a result of surgery or any other intervention. After correcting the deformation of the musculoskeletal system (redressing), pain is added to the swelling. In such cases, the patient is prescribed physical procedures for 3-10 days.
If the patient is in severe pain, he is prescribed analgesics.
If there is no pain, he is recommended to perform a number of special exercises involving alternating positions. A controlled load gives a positive result.
Aseptic edema
This type of bone marrow edema first develops in the neck or head of the femur. Its presence is determined visually:
- The sore spot turns red;
- Its temperature rises;
- Swelling is clearly visible;
- There are painful sensations.
Small blood vessels in the affected area release exudate of the serous or fibrinous type, or combinations thereof, into the tissue.
Also, swelling can have different localization. Along with the usual, subchondral edema is distinguished, affecting the subchondral (subchondral) plate. Such edema is detected by urine analysis for C-terminal cross-linked telopeptides of type II collagen.
Diagnostics
Spinal cord edema is detected by the following methods:
- Plain X-ray: demonstrates significant damage to the bones. The information content depends on the correct choice of projection, that is, the patient’s position relative to the emitter. But in any case, small cracks are not detected. It is also impossible to see the swelling itself, since radiography does not visualize the condition of soft tissues well;
- Computed tomography: this method is also based on the use of x-rays, but it is more effective: all damage is detected, down to the smallest. The doctor receives not a snapshot, but a 3D image of the spine obtained as a result of layer-by-layer scanning. But soft tissues are still almost invisible;
- Magnetic resonance imaging (MRI): a fundamentally different diagnostic method that involves exposing the area of the body under study to a powerful magnetic field that causes hydrogen atoms to become excited, and then analyzing the radiation generated by the atoms when they return to a normal state. Due to its high resolution (defects up to 0.5 mm in size are detected) and the ability to visualize soft tissue, MRI is superior to all other methods in terms of information content. The doctor clearly sees the location of the edema and its size.
MRI is especially effective for vasogenic edema, since the contrast agents used in this method leak through the walls of the capillaries along with the blood.
The disadvantage of MRI is that it cannot be used if the patient has metal elements in the body: pacemaker, plates, pins, prostheses, fillings, etc.
Treatment of cerebral edema
Eliminating the problem under discussion is one of the most difficult tasks for anyone, even the most qualified doctor. The situation is complicated by the fact that in this case the patient’s life is at stake and wrong actions can lead to his death.
One of the treatment methods is to reduce pressure in the spinal cord
The main task of the doctor in the acute period of the disease is to restore the normal level of CPP (cerebral perfusion pressure), since the supply of necessary substances to the neurons and the adequacy of the blood supply depend on it. With the problem under discussion, we have increased intracranial pressure, which reduces CPP with all the ensuing consequences. To eliminate high intracranial pressure, the following measures are taken:
- support oxygenation;
- eliminate and prevent the occurrence of nociceptive and pain reactions
- eliminate convulsions and motor agitation;
- maintain normal body temperature;
- diuretics are prescribed;
- carry out moderate hyperventilation;
- eliminate the causes that disrupt the outflow from the cranial cavity.
All the measures described fit into the concept of “conservative” treatment, but in this situation it is not always effective. In this case, surgery is necessary. Typically, craniotomy is performed, the main purpose of which is to reduce intracranial pressure. This decompression surgery involves removing a bone flap. It should be understood that swelling of the spinal cord or brain is a very serious problem, the treatment of which is quite complex, since in this situation the doctor has to make decisions quickly enough, without making mistakes.
Surgery as a last resort treatment for edema