Content:
- 1 Pituitary tumors
- 2 Adiposogenital dystrophy (Pechkarants-Babinsky-Froelich syndrome)
- 3 Gigantism
- 4 Diabetes insipidus
- 5 Hyperhydropexic syndrome (Parhon's syndrome)
- 6 Lawrence-Moon-Bardet-Biedl syndrome
- 7 Hypothalamic-pituitary cachexia (Simmonds syndrome) and postpartum hypopituitarism (Schien syndrome)
- 8 Persistent lactation and amenorrhea syndrome (Chiari-Fromel)
- 9 Itsenko-Cushing disease and syndrome
- 10 Dysregulation of intraocular pressure in hypothalamic-pituitary lesions
Description
The hypothalamus and pituitary gland
are in close anatomical and functional connection, so they are considered as a single system.
It is even recommended to isolate the hypothalamic-adrenergic pituitary system
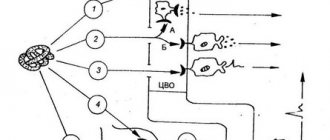
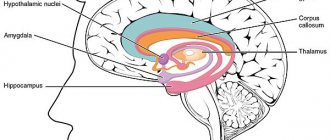
. The hypothalamus produces releasing hormones that stimulate or inhibit the hormones of the adrenergic pituitary gland. The neurohypophysis accumulates and releases vasopressin and oxytocin into the blood, hormones that are synthesized in the supraoptic and paraventricular nuclei of the hypothalamus. These hormones are called neurohormones, and the supraoptic, paraventricular nuclei of the hypothalamus and the neurohypophysis are recommended to be called the hypothalamic-neurohypophyseal endocrine gland [Baranov V. G. et al., 1977].
Since many hypothalamic-pituitary diseases in which ocular symptoms are observed are caused by pituitary tumors, we will consider this issue at the beginning of this chapter.
Functions
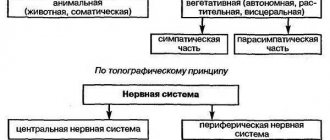
In short, the physiology of the hypothalamic-pituitary system is associated with maintaining homeostasis (self-regulation, ensuring normal functioning of the body, taking into account changing environmental conditions). The hypothalamic-pituitary neurosecretory system coordinates the activity of the peripheral glands, which leads to the formation of adequate behavioral and autonomic reactions corresponding to the current situation.
The hypothalamus is a connecting element between the endocrine system and the autonomic part of the nervous system. In this area of the medulla, nerve fibers are localized, through which impulses are received from sensory receptors - olfactory, gustatory, visceral (located in the area of internal organs). The production of neurohormones occurs predominantly in the anterior lobe and the middle (medial) region of the hypothalamic region.
Neurons of the hypothalamic zone produce peptide-type neurohormones, which are transported to the posterior pituitary gland through synaptic connections between axons. Vasopressin and oxytocin are transported to the posterior compartment. Neurohormones regulate cardiovascular activity (heart rate, blood pressure), respiratory function and the functioning of the gastrointestinal tract (peristalsis, secretion of gastric juice).
The medulla oblongata is involved in the regulation of the autonomic part of the central nervous system. Individual areas of the hypothalamus, as part of their interaction with the limbic system, regulate functions such as behavioral reactions, circadian rhythms (sleep-wake patterns) and physiological needs (hunger, thirst). Other features:
- Maintaining metabolic processes (protein, lipid, carbohydrate, water-salt metabolism) at an optimal level.
- Regulation of the energy production process.
- Coordination of the body's temperature balance.
- Management of the digestive tract.
- Management of excretory functions.
For example, stressful effects provoke increased activity of the medial (located closer to the median plane) portion of the hypothalamic complex, which in turn leads to accelerated production of cortisol in the adrenal cortex. As a result, the concentration of corticoliberin releasing factor increases.
The cascade reaction continues with the accelerated production of adrenocorticotropic hormone by the anterior structures of the pituitary gland, which leads to the development of hypercortisolism. The hypothalamus contains small cell neurons that regulate the activity of the anterior pituitary gland with the help of stimulating and inhibitory (suppressing activity) substances (liberins, statins). Influencing factors enter the adenohypophysis through the hypothalamic-pituitary portal structures.
Feedback with peripheral endocrine sections is organized through receptors located on the membranes of nerve cells that form the hypothalamus. Receptors respond to hormones from the peripheral glands of the endocrine system. As a result, the process of neurosecretion is closely related to the concentration of substances produced by peripheral endocrine glands.
Receiving information about the concentration of hormones produced by the endocrine periphery, the hypothalamus and pituitary gland correct disorders in case of hypofunction or hyperfunction. Correction of hormonal balance is carried out through the release of neurohormones with stimulating or inhibitory effects into the portal pathways of the pituitary gland.
The pituitary system produces tropic hormonal substances that stimulate or suppress the functional activity of the peripheral endocrine glands. The pituitary gland is located in the area of the sella turcica at the base of the skull. The growth of the dura mater from above separates the medullary gland from other structures.
The functions of the anterior segment of the pituitary gland, which occupies 80% of the gland, are associated with the integration of information coming from the peripheral endocrine complex and the hypothalamic region, and with the subsequent coordination of the work of the endocrine periphery.
↑ Pituitary tumors
The main form of pituitary gland pathology is tumors
. These are predominantly adenomas of the anterior or glandular lobe (adenohypophysis). There are three groups of adenomas: eosinophilic, basophilic and chromophobic. Endocrine disorders in adenomas make it possible to distinguish lesions of the chiasma caused by these tumors from lesions of other origin.
Endocrine disorders
in tumors of the pituitary gland they are very diverse, but are not always observed; sometimes they are absent in
chromophobe adenomas
. Pituitary adenoma without endocrine disorders is isolated into a special clinical form and is called the “ophthalmic form.” Its leading manifestation, in addition to the destruction of the sella turcica, is eye symptoms [Tron E. Zh., 1966].
destroy the sella turcica to varying degrees
, which is revealed by x-ray examination of the skull; however, with very small tumors, they are not detected x-ray.
Due to excess production of somatotropic hormone by the anterior pituitary gland, the clinical picture of acromegaly
. The earliest manifestations of acromegaly are sexual dysfunction and headaches.
Due to disproportionate bone growth
the shape of the skull, mainly the facial one, changes greatly, the lower jaw is especially noticeably enlarged. Cartilage and soft tissues and auricles grow; the nose becomes thick, the tongue enlarges, the lips thicken, and swelling of the eyelids appears. The hands, feet, etc. become greatly enlarged.
Due to the disorder of various endocrine functions of the pituitary gland, the functions of other endocrine glands
(diabetes mellitus, thyroid disease, diabetes insipidus).
Very often eye symptoms are observed in combination with endocrine
disorders in tumors such as craniopharyngiomas. Craniopharyngioma is usually located suprasellar (sometimes intersellar) and is a cyst with cholesterol crystals that has a tendency to calcify. The tumor compresses the third ventricle or blocks the foramen of Monroe, resulting in increased intracranial pressure. The growth of craniopharyngioma is accompanied by pressure on the sella turcica, chiasm and hypothalamic region.
Endocrine disorders include decreased function of the pituitary gland and hypothalamus
; This is manifested in children by stunted growth, underdevelopment of the genital organs, secondary sexual characteristics, fat deposition on the chest and abdomen, drowsiness and the development of diabetes insipidus. At a young age, sexual dysfunction is observed.
Timely diagnosis of these tumors and appropriate treatment (radiation therapy, surgical removal) are of paramount importance to prevent blindness
, and often to save the patient’s life, so the role of the ophthalmologist in examining such patients cannot be overestimated.
The hypothalamic-pituitary system and its role in regulating the activity of the endocrine glands
Blood system in children and adolescents
2. The hypothalamic-pituitary system and its role in regulating the activity of the endocrine glands
The pituitary gland is located at the base of the brain under the hypothalamus. The mass of the gland ranges from 0.35–0.65 g. The hypothalamus is connected to the pituitary gland by the general blood supply system. It regulates the work of the pituitary gland, and the latter directly or indirectly affects the work of all endocrine glands. Consequently, the hypothalamic-pituitary ligament ensures coordination of the work of two regulatory systems - nervous and humoral. Thanks to the work of these two systems, the hypothalamus receives information from all parts of the body: signals from extero- and interoreceptors go to the central nervous system through the hypothalamus and are transmitted to the endocrine organs.
The pituitary gland consists of three lobes - anterior, middle and posterior. The anterior lobe of the pituitary gland produces several hormones that regulate and coordinate the work of other endocrine glands. Two hormones have a powerful effect on the reproductive system. One (oxytocin) enhances sexual function, and the other (prolactin) promotes the growth of mammary glands and milk production in women, but suppresses sexual activity. The most well-known hormone of the anterior pituitary gland is somatropin (STH). It has a powerful effect on the metabolism of proteins, fats and carbohydrates, and stimulates body growth. With an excess of growth hormone (GH) in childhood, a person grows to 250–260 cm. If somatropin is produced more than normal (hyperfunction) in an adult, then the cartilaginous and soft tissues of the face and limbs grow (acromegaly). With hypofunction, a sharp slowdown in growth occurs, which leads to the preservation of the proportions of the child's body and underdevelopment of secondary sexual characteristics (pituitary dwarf). Adult dwarfs are no taller than 5–6 year old children. The middle lobe of the pituitary gland produces a hormone that regulates the formation of skin pigments. The posterior lobe does not produce hormones at all. Here, hormones that synthesize the nuclei of the hypothalamus are accumulated, stored and, as needed, released into the blood. The best known of these hormones is vasopressin, which regulates the process of urine formation. With hyperfunction, the process is suppressed and only 200-250 ml of urine is released per day, but edema occurs (Parhan syndrome). With a lack of hormone (hypofunction), diuresis increases sharply to 10–40 liters per day, but since the urine does not contain glucose, the disease is called diabetes insipidus.
Neurosensory cells of the hypothalamus convert afferent stimuli into humoral factors with physiological activity that stimulate the synthesis and release of pituitary hormones. Hormones that inhibit these processes are called inhibitory hormones or statins.
Hypothalamic releasing hormones influence the function of pituitary cells, which produce a number of hormones. The latter, in turn, influence the synthesis and secretion of hormones from the peripheral endocrine glands, and these affect organs or tissues. All levels of this system of interactions are closely interconnected by a feedback system.
Mediators of sympathetic and parasympathetic nerve fibers play an important role in regulating the function of the endocrine glands.
However, there are endocrine glands that are regulated in a different way due to the influence of the level of antagonist hormones, as well as as a result of changes in the concentration of those metabolites (substances), the level of which is regulated by these hormones. There are some hormones produced in the hypothalamus, pituitary hormones, which directly affect organs and tissues.
3. Features of the relationship between the population and the environment in the context of modern scientific and technological revolution. Children's health problem
The scientific and technological revolution has opened up enormous opportunities for humanity to transform the natural environment and use natural resources. However, as human intervention in the natural environment intensifies, the damage to nature becomes increasingly obvious, sometimes reaching levels that can threaten the health and well-being of humans themselves.
The problems of interaction between man and his environment are dealt with by many specialists from various scientific disciplines, from philosophical to technical. Each discipline sees its own aspect of this interaction, determined by its subject of study. However, due to the complex nature of the interaction between man and the environment, there is a need for the emergence of a unified discipline that would use the knowledge accumulated by various sciences on this problem and, on their basis, develop its own approaches and research methods.
In modern conditions of intensive scientific and technological progress, characterized by global changes in the natural environment and the emergence of many new physical and chemical factors that pollute the natural environment, human ecology has become such an integrating discipline. Its goal is to maintain and preserve healthy biogeocenoses.
Currently, human economic activity is increasingly becoming the main source of pollution of the biosphere. Gaseous, liquid and solid industrial wastes are entering the natural environment in increasing quantities. Various chemicals contained in waste, entering the soil, air or water, pass through ecological links from one chain to another, ultimately ending up in the human body.
The body's reactions to pollution depend on individual characteristics: age, gender, health status. As a rule, children, elderly and sick people are more vulnerable. Doctors have established a direct connection between the increase in the number of people suffering from allergies, bronchial asthma, cancer, and the deterioration of the environmental situation in this region. It has been reliably established that industrial wastes such as chromium, nickel, beryllium, asbestos, and many pesticides are carcinogens, that is, they cause cancer. Even in the last century, cancer in children was almost unknown, but now it is becoming more and more common. As a result of pollution, new, previously unknown diseases appear. Their causes can be very difficult to establish.
Highly biologically active chemical compounds can cause long-term effects on human health: chronic inflammatory diseases of various organs, changes in the nervous system, effects on the intrauterine development of the fetus, leading to various abnormalities in newborns.
In addition to chemical pollutants, there are also biological pollutants in the natural environment that cause various diseases in humans. These are pathogenic microorganisms, viruses, helminths, and protozoa. They can be found in the atmosphere, water, soil, and in the body of other living organisms, including the person himself.
Literature
1. Agadzhanyan N.A., Tell L.Z., Tsirkin V.I., Chesnokova S.A. Human physiology. – M.: Medical Book, N. Novgorod: Publishing House of NGMA, 2003. – 528 p.
2. Melnichenko E.V. Age physiology. Reader for theoretical study of the course “Age-related physiology.” Part 1. Simferopol, 2003
3. Nikiforov R.A., Popova G.N. Biology. Human. RIC "Atlas", 1995
4. Scientific and technological revolution, health, healthcare / Ed. A.F. Sergenko, O.A. Alexandrova. – M.: Medicine, 1984. – 248 p.
5. Fedokovich N.I. Human anatomy and physiology: Textbook. Ed. 5th. – Rostov n/d: Publishing house: “Felix”, 2004. – 416 p.
Blood system in children and adolescents
Information about the work “Blood system in children and adolescents”
Section: Medicine, health Number of characters with spaces: 20125 Number of tables: 0 Number of images: 0
Similar works
Features of the body and adaptation to physical activity in children of middle and high school age
88437
5
8
... and high school age, significant changes occur in growth and in the functioning of all organs and systems. 3. Physiological features of adaptation of children of middle and high school age to physical activity The period of middle and high school age has its own specific mechanisms and patterns of adaptation to stress associated with age-related characteristics of development...
Adaptation of children and adolescents to physical activity in the North
84604
12
11
... characteristics are individual developmental characteristics. They vary and depend on the state of health, living conditions, and the degree of development of the nervous system. Chapter II. Research materials 2.1. Research objectives 1. To study the methodological foundations of adaptation of children and adolescents to physical activity. 2. Determine students’ adaptation to physical activity. 3. Assess your health status and...
Study of the influence of tourism on the level of development of general endurance in children of secondary school age
63676
18
4
... combined with smooth operation. This allows you to master large volumes of load with a fairly intense level of exposure [26, p. 115]. Chapter 2. Study of the influence of tourism on the level of development of general endurance of children of secondary school age 2.1 Organization of the study At the first stage of the study, literary sources on this topic were studied. This mainly concerned...
Treatment and rehabilitation of sick children and adolescents with deviant and delinquent forms of behavior in a psychiatric hospital
11890
1
0
... establishments in the absence of persons of the opposite sex. This behavior is observed in adolescents with insufficiently formed selectivity of sexual desire. Dynamics of increase in delinquent and deviant behavior in children and adolescents of the psychiatric hospital of the State Healthcare Institution “OPNB No. 5”. 2005 2006 2007 Number of admissions city rural city rural city rural 98 22 122 …
↑ Adiposogenital dystrophy (Pechkarants-Babinsky-Froelich syndrome)
Adiposogenital dystrophy
occurs in connection with a tumor (usually chromophobe adenoma or craniopharyngioma), hydrocele of the third ventricle, vascular thrombosis, hemorrhage, and birth trauma. This disease can also develop as a result of damage to the hypothalamus during various acute (influenza, typhoid fever, etc.) and chronic (tuberculosis, syphilis) infectious diseases and intrauterine infection (toxoplasmosis).
Patients with this disease complain
for fatigue, drowsiness, decreased performance, weight gain, etc. The disease manifests itself in obesity and hypogenitalism. In boys, there is female-type fat deposition, absence of secondary sexual characteristics, underdevelopment of the genital organs, and cryptorchidism. Girls aged 14-15 years do not have menstruation, and there is underdevelopment of the uterus and its appendages.
Eye symptoms in adiposogenital dystrophy are caused by the above-mentioned pathological processes, depending on the location of which characteristic changes occur. With a tumor of the third ventricle, the most common eye symptom is congestive optic discs
. Congestive discs can be combined with symptoms of damage to the chiasma associated with pressure on it from the bottom of the dilated third ventricle.
From disorders of the oculomotor system
with tumors of the third ventricle, paralysis and paresis of the external eye muscles, paralysis and paresis of gaze, and nystagmus occur.
Hypothalamic-pituitary insufficiency
This pathology is characterized by a decrease in the level of hypothalamic hormones, leading to hypomenstrual and hypermenstrual (less commonly) syndrome - scanty or heavy menstruation.
In women with hypothalamic-pituitary insufficiency, the uterus is reduced, the cervix has a conical shape, the tubes are elongated, thin, tortuous, and the vagina is narrow. This pathological condition is called sexual infantilism. Such anatomical features of the genital organs play a certain role in the occurrence of infertility, but the absence of ovulation is of primary importance.
Treatment of endocrine infertility is carried out depending on the nature and location of the pathological process.
For hypothalamic-pituitary insufficiency and infantilism, hormone therapy is used. Treatment should be carried out strictly as prescribed by a gynecologist under regular monitoring of the amount of sex hormones (estrogen) in the blood and urine.
↑ Gigantism
Pituitary gigantism and acromegaly
are considered as age-related variants of the same pathology. Based on this idea, a disease that begins before puberty manifests itself as gigantism, and in adulthood as acromegaly.
Gigantism
- a rare disease, more common in men;
it usually appears during puberty and is caused by increased secretion of growth hormone
in connection with hyperplasia of eosinophilic cells of the anterior pituitary gland, eosinophilic adenoma or malignant tumor. Pituitary gigantism is characterized by high growth (for men above 200 cm, for women above 190 cm). The length of the limbs prevails over the length of the body, the size of the skull does not correspond to height (relatively small). Violation of the function of the gonads is often observed. An enlargement of the thyroid gland with symptoms of hyperthyroidism, sometimes with exophthalmos, is often observed. Since eosinophilic adenoma is small in childhood, visual disturbances are usually not observed; the changes characteristic of it develop in a later period.
Hypothalamic-pituitary-ovarian regulatory system
Hormonal regulatory systems in the female body
3. Hypothalamic-pituitary-ovarian regulatory system
The menstrual cycle as a whole, with characteristic cyclic changes in the ovaries and endometrium, is under the control of a closely interconnected endocrinological network connecting the hypothalamus, pituitary gland and ovaries. Regulation in this system follows a feedback mechanism.
Luliberin, secreted by the nucleus arcuatus in the region of the mediobasal hypothalamus, is transported along the axons of neurons into the capillary network of the portal vein system in the pituitary stalk and, thus, reaches the gonadotropic cells of the anterior pituitary gland through the bloodstream. Luliberin interacts with specific surface receptors. This stimulates the synthesis and accumulation of FSH and LH in intracellular secretory granules, as well as their release.
The release of luliberin, as well as the subsequent release of LH and FSH, occurs in the form of impulses and is regulated by neurotransmitters. Norepinephrine, for example, stimulates the secretion of luliberin, while dopamine, corticoliberin, oxytocin, vasopressin, serotonin and endogenous opioids have an inhibitory effect.
The individual frequency and amplitude of pulsed releases of luliberin and FSH/LH are one of the functions of the menstrual cycle. During the follicular phase, for example, the pulse rate of LH release is in the range of 60–120 per minute. During the luteal phase, this rate progressively slows down. The greatest intervals between LH secretory impulses are observed shortly before luteal regression. There is a relationship between the concentration of progesterone in the blood serum and a slowdown in the frequency of LH secretory impulses. With the beginning of the fall in progesterone levels, from about the 23rd day of the cycle, i.e. simultaneously with the onset of lysis of the corpus luteum, the frequency of LH secretion pulses progressively increases.
Once again: luliberin controls the synthesis and release of FSH and LH. Cyclic variations in the FSH/LH ratio are a consequence of differences in the sensitivity of the pituitary gland to luliberin, this is determined by sex steroids and follicular inhibin.
Gonadotropins FSH and LH are second-order hormones. In the target organ, the ovaries, their activity is manifested in two ways: stimulation of follicle growth and stimulation of the secretion of sex steroids. Through a “short” feedback mechanism, FSH and LH control their own secretion. Ovarian sex steroids, in turn, have a modulating effect on the hypothalamic-pituitary-ovarian hormonal system through a long-range connection. Thus, they contribute to the synchronization of hormonal profiles throughout the menstrual cycle.
Estrogens and progesterone have a dual function: they can act as both inhibitors and stimulants. For example, at the end of the follicular phase, estradiol stimulates the synthesis, vesicular storage and release of LH, apparently enhancing the release of LH and FSH caused by estradiol. Later, in the second half of the cycle, after the maturation of the corpus luteum, progesterone begins to have an inhibitory effect.
The molecular biology of steroid-mediated feedback is an area fraught with unresolved problems. After sex steroid receptors were discovered in the hypothalamus, a concept emerged according to which this mechanism is based on the regulation of the synthesis of neurotransmitters, which indirectly affect the release of luliberin. Moreover, sex steroids are thought to activate LH-degrading peptidases.
In addition, sex steroids and follicular inhibin act on the pituitary-ovarian system, selectively inhibiting the secretion of FSH.
Further studies are needed to elucidate the modulating effect of SSSH and DSG, which bind sex steroids, on the regulatory connection that exists between the hypothalamus, pituitary gland and ovaries. The same applies to the metabolic capacity of the liver and the storage and metabolic properties of the peripheral target organs of sex steroids.
4. Ovarian cycle and regulation of sex steroid biosynthesis in the ovaries
Of the 7 million oogonia primordially present in the female body, approximately 300–400 develop from the primordial follicle stage to a fully mature egg during a woman's puberty. The primordial follicle consists of an oocyte and a maximum of 10 granulosa cells with a total size of 0.1 mm. The following stages of follicle development are called: primary, secondary and tertiary follicle stages. The tertiary follicle in the preovulatory stage contains approximately 50–60 million granulosa cells, a fluid-filled follicular cavity called the antrum, and a layer of sheath cells enclosing the granulosa cells.
A mature egg that is ready for ovulation has a diameter of approximately 20 mm.
During the ovarian cycle, as a rule, only one primordial follicle develops to the stage of full maturation. According to many researchers, the main reason for this state of affairs is the regulatory role of hormonal levels. Most nonselectively developing primordial follicles undergo atresia. The selective stimulus that determines which follicle should reach maturity appears to originate in the luteal phase of the previous menstrual cycle in the form of a hormonal signal. The rise in FSH concentration, observed at the end of the cycle simultaneously with a fall in progesterone levels, is probably a key tool for selecting the next primordial follicle and sensitizing it to further hormonal impulses.
The secretion of estradiol increases with the onset of follicle maturation. Following this, the following mechanisms are triggered: estradiol, together with FSH, induces receptors located on the surface of granulosa cells. The result of this is an increase in binding capacity, which leads to an increase in the sensitivity of the follicular apparatus to FSH, thereby causing additional growth. Next, FSH activates aromatase present in granulosa cells, thereby starting the process of converting androgens into estradiol. At this stage of evolution, the maturing follicle containing follicular fluid is rich in FSH and estradiol. The concentration of hormones in the follicular fluid is necessary and sufficient for the full growth of the follicle and its maturation, despite the fact that the level of estradiol, increasing until the end of the follicular phase, causes a progressive blockade of pituitary FSH secretion. The remaining follicles, which have reached only the early stage of evolution, are deprived of FSH stimulation and die.
From the beginning to the middle of the follicular phase, granulosa cells are practically devoid of specific receptors for LH. Thus, the effect of LH at this stage of the menstrual cycle is limited to its effect only on the cells of the inner lining of the follicle wall. Under the influence of LH, androgens are formed from cholesterol esters, which are transported to granulosa cells as estradiol precursors.
Under the influence of FSH, towards the end of the first half of the cycle, there is an enhanced induction of LH receptors located on the surface of granulosa cells.
The proportion of LH-stimulated androgens and FSH-stimulated estradiol is crucial for the process of normal follicle maturation. Excessive androgens lead to atresia, and only a balanced dominance of estrogen stimulation allows the follicle to fully mature.
A massive LH surge based on the preovulatory peak causes luteinization of granulosa cells and switches steroid biosynthesis to progesterone production. Simultaneously, approximately 28–36 hours after the massive LH surge, ovulation is initiated. In addition to the synthesis of progesterone, the corpus luteum also secretes estradiol and androgens.
The duration of progesterone synthesis, as well as its release during the luteal phase, is directly dependent on the number of LH receptors, the maximum number of which is observed on days 22 and 24 of the cycle. After the onset of menstrual bleeding, LH receptors are not detected in the corpus luteum. The regulatory mechanism also involves an inhibitor of LH binding; present in the cells of the corpus luteum and follicular fluid.
There is no doubt that the full functioning of the corpus luteum can only occur in the case of optimal hormonal stimulation of the preovulatory dominant follicle. The concentration of LH receptors is the most important indicator of normal development of the corpus luteum, however, since the induction of LH receptors is mediated by FSH, transient suppression of FSH during the follicular phase of the cycle can automatically lead to a decrease in estradiol and progesterone levels, as well as a reduction in cellular mass of the corpus luteum. In relation to clinical practice, the main conclusion from the above may be that treatment of corpus luteum deficiency should be carried out during the follicular phase of the cycle, rather than replacement during the luteal phase.
Ovulation, which is the release of the cumulus oophorus, is provoked by a combination of increased intrafollicular pressure, prostaglandin-mediated activation of collagenases with subsequent partial destruction of the fibrous structures of the follicle wall, as well as contractile stimuli.
Hormonal regulatory systems in the female body
Information about the work “Hormonal regulatory systems in the female body”
Section: Medicine, health Number of characters with spaces: 14118 Number of tables: 0 Number of images: 14
Similar works
Physiology of the endocrine system
68349
0
0
..., called the general adaptation syndrome (G. Selye). The pituitary-adrenal system plays a major role in the development of adaptation syndrome. Pancreas The pancreas is a mixed-function gland. Endocrine function is carried out through the production of hormones by the pancreatic islets (islets of Langerhans). The islands are located mainly in the tail...
The state of the immune system in adolescents
68852
0
0
... adaptive reactions in adolescents are very important both in terms of studying intersystem connections in the body and for purely applied purposes. This is determined by the need to predict the state of a teenager’s immune reactivity, select optimal conditions for vaccination, and adequate treatment of diseases. In recent years, much attention has been paid to circadian, infradian and annual biorhythms. ...
Features of the body and adaptation to physical activity in children of middle and high school age
88437
5
8
... and high school age, significant changes occur in growth and in the functioning of all organs and systems. 3. Physiological features of adaptation of children of middle and high school age to physical activity The period of middle and high school age has its own specific mechanisms and patterns of adaptation to stress associated with age-related characteristics of development...
Endocrine system of animals and humans
27269
1
0
... in livestock farming in order to increase the number of livestock and increase its productivity, as well as veterinary medicine and medicine for the treatment of various diseases of the endocrine system. Consider in detail the problem of iodine deficiency diseases in humans and animals in Russia, in particular in the Orenburg region, the causes and ways to solve the problem, the main approaches to prognosis, diagnosis and treatment of iodine deficiency...
↑ Diabetes insipidus
There are hypothalamic and renal forms
diabetes insipidus. Hypothalamic diabetes insipidus is caused by a lack of antidiuretic hormone production. It can be an independent disease or one of the manifestations of some endocrine and non-endocrine diseases; most often occurs between the ages of 18 and 25 years.
Renal diabetes insipidus
observed only in males. The disease is genetically determined and is inherited in a recessive, sex-related manner.
Diabetes insipidus is most often caused by neurotropic viral infections
(influenza, etc.)" may be associated with other acute and chronic diseases (whooping cough, scarlet fever, typhoid fever, relapsing fever, sepsis, tuberculosis, syphilis), as well as with traumatic brain injury, tumors of the pituitary gland and hypothalamus. This disease can be combined with other endocrine pathologies (adiposogenital dystrophy, acromegaly and gigantism, pituitary dwarfism, Simmonds syndrome, Itsenko-Cushing disease).
Antidiuretic hormone deficiency
can be absolute, in case of damage to the supraoptic and paraventricular nuclei of the hypothalamus, as well as the hypothalamic-pituitary tract, through the fibers of which neurosecretion enters the posterior lobe of the pituitary gland, and relative, due to the excess of its destruction in the periphery.
Diabetes insipidus can also develop due to congenital pathology of kidney tubule receptors
.
Lack of antidiuretic hormone causes a decrease in water reabsorption
renal tubules and increased diuresis. Dehydration occurs, which is accompanied by irritation of the corresponding center of the hypothalamus, resulting in severe thirst.
Diabetes insipidus most often occurs suddenly, less often develops gradually. Patients complain
for constant thirst and frequent copious urine output, loss of appetite, headache, weakness, etc.
The stomach may expand due to the intake of large amounts of liquid, as well as its prolapse; sometimes gastritis and colitis develop.
In some cases, women experience menstrual irregularities up to amenorrhea and a tendency to spontaneous abortion. Men experience decreased libido and impotence. Children experience delayed growth and sexual development, and bedwetting.
Changes in the organ of vision
in diabetes insipidus, they are mainly observed in cases where this disease develops as a result of damage to the hypothalamic-pituitary region by a tumor or an inflammatory process.
If there is compression of the area of the optic chiasm by a tumor or other formation, then chiasmatic syndrome
congestive optic disc
occurs . Possible increase in intraocular pressure.
Other changes in the visual organ have been described in diabetes insipidus.
. Sometimes there are complaints of “dry” eyes and fatigue when reading. A significant decrease in the sensitivity of the cornea and sluggish pupillary reactions were noted.
↑ Hyperhydropexic syndrome (Parhon's syndrome)
This disease, which occurs predominantly in men, is caused by excess production of antidiuretic hormone.
, while fluid is periodically retained in the body, water intoxication occurs, and oliguria with a high relative density of urine (1.020-1.030).
Patients with hyperhydropectic syndrome complain
for headache, decreased amount of urine excreted. Patients have dry and pale body skin, uniform obesity, and swelling often occurs in various parts of the body. Women may develop amenorrhea, men may experience decreased sexual function and impotence.
It is believed that in the occurrence of Parhon's syndrome
psychic trauma, toxic-infectious effects and allergic factors are of known importance.
Of the eye symptoms noted
narrowing of the retinal arteries, which is associated with the vasopressor effect of anhydriuretic hormone. However, total blood pressure in patients with this syndrome is not increased, which has a certain diagnostic value.
↑ Lawrence-Moon-Bardet-Biedl syndrome
This disease, like adiposogenital dystrophy, is associated with damage to the hypothalamic-pituitary system
.
Clinical manifestations
Lawrence-Moon-Bardet-Biedl syndrome are very similar to those with adiposis-genital dystrophy: obesity, hypoplasia of the genital organs, decreased sexual function, poor development of secondary sexual characteristics.
In addition to these symptoms, there is a violation
growth process, skull deformation, polydactyly, mental retardation. Characterized by muscle weakness, drowsiness, increased appetite and thirst.
Eye symptoms occupy a significant place in the clinical picture of the disease.
: strabismus, nystagmus, myopia, pigmentary degeneration of the retina.
Patients with retinal pigmentary dystrophy
complain of decreased vision and difficulty in orientation at dusk. An ophthalmoscopic examination of the fundus reveals characteristic pigment foci in its periphery, shaped like bone bodies (Fig. 42).
Rice. 42.
Retinal pigmentary dystrophy.
Gradually their number increases, they spread to the center, the vessels of the retina narrow. Other areas of the fundus become discolored, sometimes so much so that the choroid itself is visible. The optic disc becomes yellowish-white and atrophic.
Central vision
remains high for a long time.
The field of view narrows concentrically, and at the extreme periphery (within 10°) it is preserved. As the process progresses, a further narrowing of the field of vision is observed, up to a tubular one. In an advanced stage, complications are sometimes observed: cataracts, glaucoma
. Changes in the macula area may also occur.
Hypothalamic-pituitary dysfunction
The causes of dysfunction of the hypothalamic-pituitary system can be physical or mental stress, infectious diseases (meningitis, encephalitis), diseases of the nasopharynx (tonsillitis, sinusitis), injuries, lack of sleep, insufficient vitamin content in a woman’s body, and fasting. As a result, the production of hormones is disrupted.
Hypothalamic-pituitary dysfunction affects patients with menstrual cycle disorders: luteal phase deficiency, anovulatory cycles (lack of ovulation) or amenorrhea. There is increased secretion of estrogen and high levels of prolactin and gonadotropin in the blood (hormones synthesized in the hypothalamus). An insufficient amount of FSH leads to a lack of follicular growth, anovulation, and, as a result, to infertility.
This group also includes women with increased levels of ovarian production of androgens (hormones responsible for male sexual characteristics). Constantly high levels of androgens lead to suppression of ovulation and can cause hirsutism (increased hair growth), acne, anovulation, and lack of menstruation.
In women with hypothalamic-pituitary dysfunction, treatment depends on the level of hormones in the blood. If there is a high level of prolactin in the blood, before prescribing hormonal therapy, a course of treatment is carried out aimed at reducing the production of prolactin. While undergoing hormonal therapy, a woman is also given stimulation of ovulation with certain drugs, which often makes it possible to conceive a child.
↑ Hypothalamic-pituitary cachexia (Simmonds syndrome) and postpartum hypopituitarism (Schien syndrome)
Hypothalamic-pituitary cachexia
(Simmonds syndrome) develops as a result of destructive changes in the anterior lobe of the pituitary gland and the hypothalamus. This leads to insufficiency of the adenohypophysis and progressive exhaustion. The disease most often affects women aged 30-40 years and is caused by damage to the hypothalamic-pituitary region by tumors, as well as acute or chronic infectious diseases (influenza, typhus, tuberculosis, syphilis, etc.), as well as skull trauma, accompanied by hemorrhage in the anterior lobe pituitary gland Simmonds syndrome can also occur after surgery - hyophysectomy.
In connection with these lesions, the function of triple hormones of the adenohypophysis is lost and, as a result, the function of the peripheral endocrine glands, mainly the thyroid gland, gonads and the adrenal cortex, is reduced.
Patients complain
for weakness, loss of appetite, headache, drowsiness, chilliness, constipation alternating with diarrhea, decreased libido, menstrual irregularities.
Characteristic signs
premature aging, severe exhaustion, weak expression of the subcutaneous fat layer, pallor and atrophy of the skin, hair loss, atrophy of the lower jaw, dental caries and tooth loss. Bradycardia, hypotension, atony and intestinal ptosis, and liver dysfunction are noted. Pronounced changes occur in the neuropsychic sphere: lethargy, depression, memory loss, etc. As the process progresses, symptoms observed in schizophrenia develop.
With Simmonds syndrome, various symptoms also occur in the visual organ.
. Patients sometimes complain of decreased vision and fatigue when reading. In some cases, there is hair loss in the eyebrow area, eyelash swelling of the eyelids, narrowing of the palpebral fissures, atrophy of the subcutaneous and orbital tissue, muscles, and retraction of the eyeballs. Sometimes swelling of the conjunctiva of the eyelids and eyeball, decreased sensitivity of the cornea, sluggish pupillary reactions, and the development of cataracts are observed.
Changes in the organ of vision are caused by
mainly by damage to the adenohypophysis by a tumor or other pathological processes. The most common is chiasmatic syndrome (bitemporal hemianopsia or bitemporal narrowing of the visual field), and later primary optic disc atrophy develops. If tumor growth is accompanied by increased intracranial pressure, optic disc congestion may develop. Naturally, all of these changes are accompanied by decreased vision.
Postpartum hypopituitarism
(Schien's syndrome) in its clinical picture is similar to Simmonds' syndrome, but is less pronounced. The disease develops slowly and has a chronic course; no severe depletion is observed. Symptoms of thyroid insufficiency are often observed, accompanied by thyroid swelling, sometimes swelling of the face and lower extremities.
Mental changes in Sheehan's syndrome are mild and associated with hypothyroidism
.
It is believed that postpartum hypopituitarism
caused by spasm of the vessels of the adenohypophysis, which occurs during labor hemorrhage.
Changes in the organ of vision
with Sheehan's syndrome are similar to those with Simmonds' syndrome, but are less pronounced.
Diagnosis of hypothalamic-pituitary dysfunction
To diagnose disorders in the hypothalamic-pituitary-ovarian system, a full range of clinical, laboratory, biochemical blood tests, hormone studies, and an X-ray of the skull (the area of the sella turcica where the pituitary gland is located) is necessary. Measuring basal temperature is informative. During the period of ovulation, there is an increase in rectal temperature by an average of 1 °C. If the luteal phase is insufficient, there is a shortening of the second phase of the cycle; the temperature difference in both phases of the cycle is less than 0.6 °C.
Ultrasound scanning of follicle growth and endometrial thickness is performed throughout the menstrual cycle.
An endometrial biopsy is performed 2–3 days before the onset of menstruation, which makes it possible to determine the functionality of the endometrium, and laparoscopy.
An informative method for studying the pituitary gland is computed tomography (CT). X-ray CT examination of the head allows us to identify changes in the density of the pituitary gland, differentiate micro- and macroadenomas, “empty” sella and cysts from normal pituitary tissue.
To diagnose neoplasms of the hypothalamic-pituitary region, MRI is used. A normal pituitary gland on MRI has the outline of an ellipse. MRI makes it possible to distinguish the pituitary stalk, the slightest changes in the structure of the pituitary gland, individual cysts, cystic tumors, hemorrhages, and cystic degeneration of the pituitary gland. The advantage of MRI is that it does not involve x-ray radiation, which makes it possible to repeatedly examine the patient over time.
↑ Syndrome of persistent lactation and amenorrhea (Chiari-Fromel)
Chiari-Fromel syndrome
occurs in women and girls as a result of damage to the hypothalamus with the subsequent development of endocrine disorders. Often the cause of the disease is chromophobe pituitary adenoma, a tumor of the hypothalamus. In this regard, prolactin-releasing inhibitory factor ceases to have an inhibitory effect on prolactin production, which leads to continuous lactation.
Patients with this syndrome complain
for headaches, menstrual irregularities, secretion of milk from the mammary glands, and this is not associated with pregnancy and breastfeeding. In some cases, there is exhaustion, in others, on the contrary, excess fat deposition. Hypertrichosis is observed.
Eye symptoms are mainly caused by pituitary tumors
a, which puts pressure on the optic chiasm. This causes a bitemporal narrowing of the visual field, bitemporal hemianopia. Subsequently, descending atrophy of the optic nerves develops.
Changes in the organ of vision
are not observed in all cases; in some patients the process does not progress for a long time and Chiari-Fromel syndrome manifests itself only as persistent lactation and menstrual irregularities, amenorrhea.
Diseases of the hypothalamic-pituitary system
As has already become clear, the pathology of this system is associated with disturbances in the normal activity of one of its departments - the hypothalamus, the anterior and posterior parts of the pituitary gland.
Any change in the hormonal balance in the body leads to serious consequences in the body. Especially when the “composer” or “conductor” makes mistakes.
In addition to hormonal imbalances, pathologies in the hypothalamic-pituitary system can be caused by cancer and injuries that affect these areas. It is impossible to list all the diseases that are in one way or another connected with this regulatory system. We will focus on the most significant pathologies and give a brief description of them.
↑ Itsenko-Cushing's disease and syndrome
In 1932, N. Cushing described in detail the clinical picture of the disease associated with the presence of basophilic pituitary adenoma
. But back in 1924, N.M. Itsenko reported a similar picture of the disease, in which changes in the interstitial brain were identified. In this regard, it was proposed to call the pathological condition described by these authors Itsenko-Cushing's disease.
Based on modern ideas about the unified system hypothalamus-pituitary-adrenal cortex, many authors call Itsenko-Cushing disease a pathological process in which the hypothalamus is primarily affected
and other parts of the central nervous system that regulate the function of the hypothalamus, the pituitary gland (pituitary adenoma), and Itsenko-Cushing syndrome is a pathological process in which the adrenal glands are primarily affected [Gpncherman E. 3., 1971; Vaskzhova E. A. et al., 1975, etc.].
Itsenko-Cushing syndrome may also be caused by ectopic tumors
, producing ACTH-like substances, and hypercortisolism associated with the treatment of various diseases with corticosteroids.
Hypercortisolism
is the main manifestation of both Itsenko-Cushing's disease and Itsenko-Cushing syndrome. The clinical manifestations of Itsenko-Cushing disease and Itsenko-Cushing syndrome have many common symptoms.
Itsenko-Cushing's disease and syndrome are observed 5 times more often in women than in men. The disease affects people aged 20 to 40 years. Already in the early period, patients complain
weakness, which is likely due to increased catabolism due to increased production of cortisol, as well as hypokalemia. Complaints of headaches, pain in the heart area, rapid heartbeat are quite common, and pain in the spine and ribs is not uncommon. Women are concerned about menstrual irregularities and infertility, while men are concerned about weakened libido and sexual function.
Complaints about changes in appearance
(obesity, skin coloring) are presented when the process has already developed. It is generally accepted that hypercortisolism causes such manifestations of the disease as osteoporosis, steroid diabetes, hypokalemia, muscle atrophy, characteristic obesity, matronism, and trophic changes in the skin. Headache, dizziness, visual and hearing disorders, drowsiness, insomnia, vestibular dysfunction, night hunger, mental depression are considered hypothalamic and cerebral symptoms.
Naturally, this division is conditional, for example, arterial hypertension may have a central origin and may be associated with hypercortisolism, as well as with secondary renal dysfunction.
With the disease and Itsenko-Cushing syndrome, patients have a characteristic appearance
: the face becomes round, moon-shaped. Obesity is observed in the neck, supraclavicular areas, mammary glands, abdomen, and back (in the area of the upper thoracic vertebrae). There are no signs of limb obesity. The skin of the face becomes purple-cyanotic, a marble pattern appears on the skin of the shoulders, legs, thighs, and stretch marks are very characteristic. Acne and boils often occur. Women experience excess hair growth.
Muscle atrophy is common
, caused by a disorder of protein metabolism (due to the catabolic effect of glucocorticoids, inhibition of protein synthesis). Osteoporosis is very common, often leading to bone fractures. Osteoporosis, which usually occurs in the late period of the disease, is caused by the catabolic effect of glucocorticoids on bone tissue.
The earliest and most common sign of the disease and Itsenko-Cushing syndrome is arterial hypertension
(Fig. 43).
Rice. 43.
Hypertensive changes in the fundus of the eye in a patient with Itsenko-Cushing syndrome.
Arterial pressure
can reach a high level (systolic 250 mm Hg, diastolic 150 mm Hg). The more severe the form of the disease, the more pronounced the arterial hypertension. In this case, symptoms of cardiovascular failure may develop.
Changes in renal function characteristic of arterial hypertension are also noted
. In the pathogenesis of hypertensive syndrome, along with a violation of the central mechanisms of regulation of vascular tone, hypersecretion of mineralocorticoid hormones - aldosterone, corticosterone - is important. Electrolyte imbalances leading to hypokalemia and hypernatremia may contribute to the development of edema.
One of the early signs of the disease and Itsenko-Cushing syndrome is a disorder of the function of the gonads
. In women, this manifests itself in menstrual irregularities, including amenorrhea, impaired fertility, hypertrichosis, and hirsutism.
In case of Itsenko-Cushing's disease and syndrome, glucose tolerance is often impaired
e and latent or overt diabetes develops. Features of the course of mild or moderate diabetes mellitus in these diseases are rare ketoacidosis, frequent glucosuria with low glycemia (discrepancy between the level of glycemia and glucosuria)
With Itsenko-Cushing's disease, approximately 10% of patients experience skin hyperpigmentation
on the neck, elbows, abdomen, caused by increased secretion of adrenocorticotropic and melanocyte-stimulating hormones. In Itsenko-Cushing syndrome, there is no hyperpigmentation of the skin.
Thus, Itsenko-Cushing's disease can be attributed to neuroendocrine forms
hypothalamic syndrome, which also includes the so-called juvenile hypercortisolism. The latter differs from typical Itsenko-Cushing's disease in that adolescents with this lesion have higher growth than their peers, which is due to excess production of somatotropic hormone along with adrenocorticotropic hormone.
In addition to the typical form of Itsenko-Cushing's disease, the so-called erased form of the disease
when, against the background of Cushingoid changes in the patient’s appearance, there are no symptoms characteristic of Itsenko-Cushing’s disease: osteoporosis, arterial hypertension, obvious disturbance of carbohydrate metabolism [Vasyukova E. A. et al., 1975].
Itsenko-Cushing syndrome
, caused by tumors of extra-adrenal localization (bronchi, pancreas, mediastinum, etc.) is marked by rapid progression and significant severity of all symptoms of the disease.
Currently, diagnostic methods have been significantly improved
Itsenko-Cushing's disease and Itsenko-Cushing syndrome, which provides the possibility of differential diagnosis between them. These methods include determining the rate of secretion and studying the content of corticosteroids in the blood and urine. In Itsenko-Cushing's disease, the secretion of cortisol increases significantly with a relatively slight increase in the secretion of other corticosteroids; with benign tumors of the adrenal cortex, the production of corticosteroids and their content in the blood and urine differ little from the corresponding indicators for Itsenko-Cushing's disease, and with malignant tumors of the adrenal cortex, a significant increase in the secretion of 11-deoxycortisol and corticosterone is noted.
Functional tests are of known importance for the differential diagnosis of Itsenko-Cushing disease and Itsenko-Cushing syndrome. Tests with metapyrine and dexamethaeon have become widespread
.
In the diagnosis of Itsenko-Cushing's disease and syndrome, X-ray examination
plays a minor role. Basophilic pituitary adenomas, which can cause Cushing's disease, are small in size and are not detected x-ray (due to this, there are no ocular symptoms characteristic of pituitary tumors). Tumors of the adrenal cortex, causing Itsenko-Cushing syndrome, are detected radiographically only when they reach large sizes, and in most cases they are not detected.
With the disease and Itsenko-Cushing syndrome, various eye symptoms
. In connection with arterial hypertension, retinal angiopathy is most often detected, which disappears when blood pressure normalizes; Hypertensive angiosclerosis of the retina and even less often hypertensive retinopathy develops less often. The predominant occurrence of small changes in the retina (angiopathy) is apparently due to the fact that both the disease and Itsenko-Cushing syndrome develop at a young age, when the intraocular vascular system is highly resistant to damaging factors [Margolis M. G., 1973] .
In case of Itsenko-Cushing's disease and syndrome, disturbances in the regulation of intraocular pressure
, usually of the transient symptomatic hypertension type. An increase in ophthalmotonus can also be persistent, with the development of symptoms of glaucoma. There are studies indicating that primary glaucoma may be a consequence of hypercortexism.
exophthalmos can sometimes develop
, which is associated with increased hormonal function of the anterior pituitary gland, from which a special exophthalmic factor is isolated.
With Itsenko-Cushing's disease, there may be symptoms caused by damage to the basal-diencephalic parts of the brain
: feeling of protruding eyeballs, pain in the area of the superciliary arches and behind the eyeballs. In inflammatory processes at the base of the brain, changes in the optic nerves may develop; sometimes ptosis of the upper eyelid, anisocorpus, and upward gaze paralysis occur, which is apparently caused by damage to the quadrigeminal tract and the nuclei of the oculomotor nerves [Gincherman E. 3., et al., 1969].