Sympathetic (shown in blue) and parasympathetic (shown in red) divisions of the autonomic nervous system
Autonomic nervous system
(from lat. vegetatio - excitement, from lat. vegetativus - plant),
ANS
,
autonomic nervous system
,
ganglion nervous system
(from lat. ganglion - nerve ganglion), visceral nervous system (from lat. viscera - insides), organ nervous system , celiac nervous system,
systema nervosum autonomicum
(PNA) is part of the body’s nervous system, a complex of central and peripheral cellular structures that regulate the functional level of the body, necessary for the adequate response of all its systems.
The autonomic nervous system is a section of the nervous system that regulates the activity of internal organs, endocrine and exocrine glands, blood and lymphatic vessels[1]. Plays a leading role in maintaining the constancy of the internal environment of the body and in the adaptive reactions of all vertebrates.
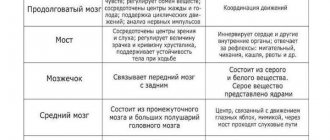
Anatomically and functionally, the autonomic nervous system is divided into sympathetic, parasympathetic and metasympathetic. The sympathetic and parasympathetic centers are under the control of the cerebral cortex and hypothalamic centers [2].
The sympathetic and parasympathetic divisions have central and peripheral parts. The central part is formed by the bodies of neurons lying in the spinal cord and brain. These clusters of nerve cells are called vegetative nuclei. Fibers extending from the nuclei, autonomic ganglia lying outside the central nervous system, and nerve plexuses in the walls of internal organs form the peripheral part of the autonomic nervous system.
The sympathetic nuclei are located in the spinal cord. The nerve fibers extending from it end outside the spinal cord in the sympathetic ganglia, from which the nerve fibers originate. These fibers are suitable for all organs.
The parasympathetic nuclei lie in the midbrain and medulla oblongata and in the sacral part of the spinal cord. Nerve fibers from the nuclei of the medulla oblongata are part of the vagus nerves. From the nuclei of the sacral part, nerve fibers go to the intestines and excretory organs.
The metasympathetic nervous system is represented by nerve plexuses and small ganglia in the walls of the digestive tract, bladder, heart and some other organs.
The activity of the autonomic nervous system does not depend on the will of a person. This means that under normal conditions a person cannot force his heart to beat less often or his stomach muscles not to contract. However, it is possible to achieve conscious influence on many parameters controlled by the ANS using special training methods - for example, using biofeedback methods.
The sympathetic nervous system enhances metabolism, increases the excitability of most tissues, and mobilizes the body's forces for vigorous activity. The parasympathetic system helps restore spent energy reserves and regulates the functioning of the body during sleep.
The organs of circulation, respiration, digestion, excretion, reproduction, as well as metabolism and growth are under the control of the autonomous system. In fact, the efferent section of the ANS carries out nervous regulation of the functions of all organs and tissues, except for skeletal muscles, which are controlled by the somatic nervous system.
Unlike the somatic nervous system, the motor effector neuron in the autonomic nervous system is located in the periphery, and the spinal cord only indirectly controls its impulses.
Terms autonomous system
,
visceral system
,
sympathetic nervous system
are ambiguous. Currently, only part of the visceral efferent fibers is called sympathetic. However, different authors use the term "sympathetic" in different ways:
- in the narrow sense, as described in the sentence above;
- as a synonym for the term "autonomous";
- as the name of the entire visceral (“autonomic”) [3] nervous system - both afferent and efferent.
Terminological confusion also arises when the entire visceral system (both afferent and efferent) is called autonomous.
The classification of parts of the vertebrate visceral nervous system, given in the manual [4] by A. Romer and T. Parsons, is as follows:
Visceral nervous system:
- afferent;
- efferent: special gill;
- autonomic: sympathetic;
- parasympathetic.
Content
- 1 Morphology 1.1 Central and peripheral sections 1.1.1 Central section
- 1.1.2 Peripheral department
- 2.1 General significance of autonomic regulation
SYMPATHETIC AND PARASYMPATHETIC DIVISIONS AND THEIR DIFFERENCES
Based on anatomical and functional differences in the autonomic nervous system, two divisions were identified - sympathetic and parasympathetic.
The sympathetic department is trophic in its main functions. It provides increased oxidative processes, increased respiration, increased heart activity, i.e. adapts the body to conditions of intense activity. In this regard, the tone of the sympathetic nervous system predominates during the day, and at night - the parasympathetic one (“the kingdom of the vagus”). The parasympathetic department plays a protective role (constriction of the pupil, bronchi, decreased heart rate, emptying of the abdominal organs).
The sympathetic and parasympathetic divisions often act as antagonists (Table 1). However, this antagonism is relative. With a sharply changed functional state of the organ, they can act unidirectionally as synergists. In response to increased activity of the body, parasympathetic shifts occur, aimed at restoring energy potential and homeostasis. Thanks to the activity and synergy of both parts of the autonomic nervous system, long-term, adaptive activity of the body is possible.
Thus, between them there is not so much antagonism as interaction, which ensures the most subtle regulation of organ activity.
The sympathetic and parasympathetic divisions also differ in mediators - substances that transmit nerve impulses at synapses. The mediator in sympathetic nerve endings is sympathin (similar to norepinephrine). The mediator of parasympathetic nerve endings is a substance close to acetylcholine.
Along with the functional ones, there are a number of morphological differences in the sympathetic and parasympathetic divisions of the autonomic nervous system, namely:
1. The foci of parasympathetic fibers exiting the brain are separated from each other (mesencephalic, bulbar, sacral sections), sympathetic fibers exit from one, but more extended focus (thoracolumbar section).
2. The sympathetic nodes include nodes of the 1st and 2nd order, and the parasympathetic nodes include the 3rd order (terminal). In this connection, preganglionic sympathetic fibers are shorter, and postganglionic fibers are longer than parasympathetic.
3. The parasympathetic division has a more limited area of innervation, innervating only internal organs. The sympathetic department of the autonomic nervous system, in addition to internal organs, innervates all blood vessels, sweat, sebaceous glands and hair muscles of the skin, as well as skeletal muscles, providing it with trophic innervation.
SYMPATHETIC DIVISION OF THE AUTONOMIC NERVOUS SYSTEM
The sympathetic nervous system consists of central and peripheral divisions.
The central section is represented by the nuclei of the lateral horns of the gray matter of the spinal cord (nuclei intermediolaterales) of the following segments: C8, Th1-12, L1-3 (thoracolumbar region).
The peripheral division of the sympathetic nervous system consists of:
1) nodes of the first order, ganglia trunci sympathici;
2) internodal branches, rami interganglionares;
3) connecting branches are white and gray, rami communicantes albi et grisei;
4) nodes of the second order, ganglia intermediae, involved in the formation of plexuses;
5) visceral nerves, consisting of sympathetic and sensory fibers and heading to the organs, where they end in nerve endings;
6) sympathetic fibers running as part of the somatic nerves.
SYMPATHETIC TRUNK, truncus sympathicus, paired, located on both sides of the spine in the form of a chain of first-order nodes, ganglia trunci sympathici (Fig. 7).
| Rice. 7. Diagram of the structure of the sympathetic trunk (from Foss and Herlinger) 1 - cervical nodes; 2 - thoracic nodes; 3 - lumbar nodes; 4 - sacral nodes; 5 - g. impar. | In the longitudinal direction, the nodes are interconnected by branches, rami interganglionares. In the lumbar and sacral regions there are also transverse commissures that connect the nodes of the right and left sides. The sympathetic trunk extends from the base of the skull to the coccyx, where the right and left trunks are connected by one unpaired coccygeal node, gangllion impar. Topographically, the sympathetic trunk is divided into 4 sections: cervical, thoracic, lumbar and sacral. The sympathetic trunk in the cervical spine is covered with fascia, fascia prevertebralis. In the thoracic, lumbar and sacral regions, it is respectively covered by fasciae endothoracica, subperitonealis et fascia pelvis. The nodes of the sympathetic trunk are connected to the spinal nerves by white and gray communicating branches. |
The white communicating branches, rami communicantes albi, consist of preganglionic sympathetic fibers, which are axons of the cells of the intermediolateral nuclei of the lateral horns of the spinal cord. They are separated from the spinal nerve trunk and enter the nearest nodes of the sympathetic trunk, where part of the preganglionic sympathetic fibers are interrupted. The other part passes through the node in transit and through the internodal branches reaches more distant nodes of the sympathetic trunk or passes to nodes of the second order. Sensitive fibers, the dendrites of the cells of the spinal ganglion, also pass through the white connecting branches.
The white connecting branches go only to the thoracic and upper lumbar nodes. Preganglionic fibers enter the cervical nodes from below from the thoracic nodes of the sympathetic trunk through the rami interganglionares (Fig. 8), and into the lower lumbar and sacral nodes - from the upper lumbar nodes also through the internodal branches.
| Rice. 8. Sympathetic nervous system (according to S.P. Semenov). Sh8 - P3 - segments of the spinal cord with sympathetic nuclei; 1 - superior cervical sympathetic ganglion; 2 - middle cervical; 3 - lower cervical; 4 - stellate ganglion; 5 - solar plexus ganglia; 6 - large and 7 - small splanchnic nerves; 8- inferior mesenteric ganglia. |
From the nodes of the sympathetic trunk, part of the postganglionic fibers joins the spinal nerves - gray connecting branches, rami communicantes grisei, (there is no myelin sheath) and as part of the spinal nerves, sympathetic fibers are sent to the soma, where they end with nerve endings on the sebaceous and sweat glands, smooth muscles, levator hair of the skin, in the wall of peripheral vessels, as well as in skeletal muscles in order to ensure the regulation of its trophism and maintain tone. The gray connecting branches arise from all nodes of the sympathetic trunk and constitute the somatic part of the sympathetic nervous system.
In addition to the gray connecting branches, visceral branches depart from the nodes of the sympathetic trunk to innervate the internal organs - the visceral part of the sympathetic nervous system. It consists of: postganglionic fibers (cell processes of the sympathetic trunk), preganglionic fibers that passed through the first order nodes without interruption, as well as sensory fibers (cell processes of the spinal nodes).
It is important to note that preganglionic fibers in the ganglia of the sympathetic trunk branch repeatedly and form synapses on many cell bodies of effector neurons. The ratio of preganglionic fibers to postganglionic fibers can reach 1: 100. This leads to the phenomenon of animation (multiplication), i.e. to a sharp expansion of the excitation area (generalization of the effect). Due to this, a relatively small number of central sympathetic neurons provide innervation to all organs and tissues. For example, when an animal’s preganglionic sympathetic fibers passing through the anterior roots of the IY thoracic segment are irritated, constriction of the blood vessels of the scalp, neck, forelimb, dilatation of the coronary vessels, and constriction of the vessels of the kidneys and spleen can be observed.
The cervical sympathetic trunk most often consists of three nodes: superior, middle and inferior. The nodes of the cervical spine do not have white connecting branches. Preganglionic fibers come to them from the upper thoracic nodes through the internodal branches.
The upper cervical ganglion, ganglion cervicale superius, is fusiform, about 2 cm long, lies in front of the transverse processes of the II-III cervical vertebrae, on m. longus capitis. The following branches depart from it:
1. Gray connecting branches to the I-IY cervical spinal nerves;
2. The internal carotid nerve, n.caroticus internus, which in the form of two branches approaches the artery of the same name and, entwining it, forms the internal carotid plexus, plexus caroticus internus. The continuation of this plexus in the cranial cavity is the cavernous plexus, plexus cavernosus. Branches extend from the internal carotid plexus: nn. caroticotympanici, which together with the branches of the glossopharyngeal nerve form the plexus tympanicus; n. petrosus profundus, which connects to the parasympathetic nerve - n. petrosus major and forms n. canalis pterygoidei, entering the pterygopalatine ganglion. Without interruption in this node, sympathetic fibers follow to the vessels and glands of the mucous membrane of the nasal cavity and palate. From the cavernous plexus come plexuses for the branches of the internal carotid artery (plexus of the ophthalmic artery, anterior and middle cerebral arteries, plexus of the artery of the choroid plexus), as well as individual branches to the pituitary gland, trigeminal ganglion, oculomotor, trochlear and abducens nerves.
Following the course of the ophthalmic artery, sympathetic fibers are directed to the lacrimal gland, and also as part of the sympathetic root, radix sympathicus, enter the ciliary ganglion. In the node, the fibers are not interrupted, but are sent further as part of the short ciliary nerves, nervi ciliares breves, to the eyeball for innervation of the m.dilatator pupillae and the vessels of the eye. When the upper cervical node is affected, a narrowing of the pupil is observed on the side of the same name.
3. External carotid nerves, nn.carotici externi, which form a plexus around the artery of the same name - plexus caroticus externus. Due to the secondary plexuses along the branches of the external carotid artery, the salivary glands, dura mater and partially the pharynx, thyroid gland and larynx are innervated.
4. Laryngopharyngeal branches, rami laryngopharyngei, which, together with the branches of the vagus and glossopharyngeal nerves, form a nerve plexus in the wall of the pharynx, plexus pharyngeus, and some of the branches, together with n. laryngeus superior (from n. vagus) are directed to the larynx.
5. The superior cardiac nerve, n.cardiacus cervicalis superior, involved in the formation of the superficial (left) and deep (right) cardiac plexuses.
6. Ramus sinus carotici - goes to the bifurcation of the carotid artery, and the sensitive branch from n.glossopharyngeus also comes there.
7. Jugular nerve, n.jugularis, running along the internal jugular vein and disintegrating in the area of the jugular foramen into gray connecting branches to the lower node of the glossopharyngeal, nodes of the vagus and branches of the accessory and hypoglossal nerves.
The middle cervical node, ganglion cervicale medium, is located at the intersection of the inferior thyroid artery with the common carotid artery, at the level of the VI cervical vertebra. Sometimes he is missing. Its internodal branch to the lower cervical node is divided into two bundles, covering the subclavian artery in front and behind like a loop - ansa subclavia. Branches extend from it:
1. Gray connecting branches to the V, VI cervical spinal nerves.
2. Branches to the common carotid artery, forming the plexus caroticus.
3. Branches to the inferior thyroid artery - plexus thyroideus inferior.
4. Middle cardiac nerve, n. cardiacus cervicalis medius, entering the deep cardiac plexus.
The lower cervical ganglion, ganglion cervicale inferius, is located in the region of the initial section of the vertebral artery, at the level of the head of the 1st rib and often merges with the 1st thoracic node, forming the cervicothoracic node, ganglion cervicothoracicum (stellate, ganglion stellatum). Branches extend from it:
1. Gray connecting branches to the VII, VIII cervical and I thoracic spinal nerves.
2. Branches to the subclavian artery, forming the plexus subclavius along its branches.
3. Branches to the vertebral artery, forming the plexus vertebralis, due to which the membranes and vessels of the brain and spinal cord are innervated.
4. Inferior cardiac nerve, n. cardiacus cervicalis inferior, entering the deep cardiac plexus.
5. Branches to the phrenic nerve for innervation of the vessels of the abdominal cavity.
6. Branches to the trachea, bronchi, esophagus, where, together with the branches of the vagus nerve, they form plexuses.
The thoracic section of the sympathetic trunk consists of 10-12 nodes, ganglia thoracica, lying in front of the heads of the ribs. White connecting branches from the thoracic spinal nerves come to the nodes of the thoracic sympathetic trunk. The following branches depart from them:
1. Gray connecting branches to the thoracic spinal nerves.
Visceral branches depart from the upper 5-6 nodes to innervate the organs of the thoracic cavity, namely:
2. Thoracic cardiac nerves, nn. cardiaci thoracici, entering the deep cardiac plexus. All cardiac nerves extending from the nodes of the sympathetic trunk consist of sensory, postganglionic and partially preganglionic sympathetic fibers. The latter are interrupted in the nodes of the cardiac plexuses.
3. Branches to the aorta, forming the thoracic aortic plexus, plexus aorticus thoracicus, which is connected at the top with the cardiac plexus, and at the bottom with the celiac plexus.
4. Branches to the trachea and bronchi, participating together with the branches of the vagus nerve in the formation of plexus pulmonalis.
5. Branches to the esophagus directly from the nodes or from the aortic plexus, forming the plexus esophageus.
6. Branches depart from the V-IX thoracic nodes, forming the large splanchnic nerve, n. splanchnicus major.
7. From X-XI thoracic nodes - small splanchnic nerve, n. splanchnicus minor.
8. N departs from the XII thoracic node (if present). splanchnicus imus.
The splanchnic nerves pass between the crura of the diaphragm and enter the celiac plexus. They consist predominantly of preganglionic sympathetic and sensory fibers.
The lumbar section of the sympathetic trunk consists of 4-5 nodes, ganglia lumbalia, which lie on the anterior surface of the vertebral bodies (along the medial edge of the m. psoas major). A feature of these nodes is the presence of transverse fibers connecting the right and left nodes, which increases the extent of the spread of excitation.
Only the upper lumbar nodes have white connecting branches. Preganglionic fibers to the lower nodes come through the internodal branches from the upper lumbar. Branches extend from them:
1. Gray connecting branches to the lumbar spinal nerves.
2. Visceral nerves - splanchnic lumbar nerves, nn. splanchnici lumbales, consisting predominantly of preganglionic sympathetic and sensory fibers. The upper ones enter the celiac plexus, the lower ones enter the aortic and inferior mesenteric plexuses.
The sacral section of the sympathetic trunk is represented, as a rule, by four nodes, ganglia sacralia, located near the medial edge of the foramina sacralia pelvina, and one unpaired coccygeal node, ganglion impar. All nodes are connected by transverse commissures. They do not have white connecting branches. Preganglionic fibers come to them through the internodal branches from the upper lumbar nodes. Branches extend from them:
1. Gray connecting branches to the sacral and coccygeal spinal nerves.
2. Visceral branches - splanchnic sacral nerves, nn. splanchnici sacrales, consisting predominantly of preganglionic sympathetic and sensory fibers and entering the superior and inferior hypogastric plexuses.
PRESPINAL NODES AND VEGETATIVE
PLEXUS
Prevertebral nodes (ganglia intermedia) are part of the autonomic plexuses and are located in front of the spinal column. On the effector neurons of these nodes, preganglionic fibers end, passing through the nodes of the sympathetic trunk without interruption.
Autonomic plexuses are located mainly around blood vessels, or directly near organs. Topographically, the autonomic plexuses of the head and neck, chest, abdominal and pelvic cavities are distinguished.
In the head and neck area, the sympathetic plexuses are located mainly around vessels from the carotid artery system (many of them were mentioned above). They give fibers to the lacrimal gland, m. dilatator pupillae, to the salivary glands, thyroid, parathyroid glands. Next comes the laryngopharyngeal plexus, formed together with the branches of the vagus and glossopharyngeal nerves. Some fibers from the cervical plexuses innervate the trachea and esophagus.
In the chest cavity, the sympathetic plexuses are located around the descending aorta, in the region of the heart, at the hilum of the lung and along the bronchi, around the esophagus.
The most significant plexus of the thoracic cavity is the cardiac plexus, plexus cardiacus. It is formed by three pairs of cardiac nerves from the cervical nodes of the sympathetic trunk and branches of the vagus nerve. From these sympathetic and parasympathetic sources, two main nerve plexuses are formed: the superficial, plexus cardiacus superficialis, located between the concave side of the aortic arch and the division of the pulmonary trunk, and the deep, plexus cardiacus profundus, located behind the aortic arch - between it and the bifurcation of the trachea. A continuation of these plexuses are the plexuses along the coronary arteries - plexus coronarius dexter et sinister, as well as plexuses located in the wall of the heart. The most significant plexuses are located under the epicardium. There are 6 such plexuses that innervate the myocardium of the atria and ventricles, the septum between them, which are connected to the nodes of the conduction system of the heart and continue into the atrioventricular bundle (His).
The cardiac plexuses contain many vegetative (intramural) nodes, as well as afferent fibers - processes of the sensory nodes of the spinal nerves and the vagus nerve.
In the abdominal cavity, sympathetic plexuses surround the abdominal aorta and its branches (Fig. 9). Among them, the largest plexus is distinguished - the celiac plexus, as N.I. puts it. Pirogov - “brain of the abdominal cavity”.
| Fig.9. Diagram of the abdominal sympathetic plexuses (from Foss and Herlinger). 1- plexus coeliacus et gg. coeliaci; 2-g. aorticorenale et plexus renalis; 3-g. lumbale II; 4- truncus sympathicus; 5- plexus rectalis superior; 6- plexus aorticus abdominalis; 7- plexus mesentericus inferior; 8- plexus rectalis inferior; 9-nn. pelvini; 10- plexus hypogastricus inferior. |
Celiac plexus (solar), plexus coeliacus s. solaris, surrounds the beginning of the celiac trunk and the superior mesenteric artery. The plexus is bounded above by the diaphragm, on the sides by the adrenal glands, and below it extends to the level of the renal arteries. The following nodes take part in the formation of this plexus:
1. Right and left celiac ganglia, ganglia coeliaca, semilunar in shape.
2. Unpaired superior mesenteric ganglion, ganglion mesentericum superius.
3. Right and left aorto-renal nodes, ganglia aorticorenalia, located at the point of origin of the renal arteries from the aorta. These nodes receive preganglionic sympathetic fibers, which switch here, postganglionic sympathetic and parasympathetic, as well as sensory fibers passing in transit through the nodes.
The following nerves take part in the formation of the celiac plexus:
1. Greater and lesser splanchnic nerves, n. splanchnicus major et minor, extending from the thoracic nodes of the sympathetic trunk, which consist mainly of preganglionic sympathetic and sensory fibers. A minority of the fibers are represented by postganglionic fibers. The preganglionic fibers of the greater splanchnic nerve are interrupted in the celiac and superior mesenteric nodes, and the lesser - in the aortorenal nodes.
2. Lumbar splanchnic nerves, nn. splanchnici lumbales, from the upper lumbar nodes of the sympathetic trunk, containing predominantly preganglionic sympathetic fibers, interrupted in the nodes of the celiac plexus and sensory fibers.
3. Branches of the phrenic nerve, rami frenicoabdominales, consisting of sensory and postganglionic sympathetic fibers from the lower cervical ganglion of the sympathetic trunk to innervate the vessels of the abdominal cavity.
4. Branches of the vagus nerve, rami coeliaci, consisting mainly of preganglionic parasympathetic and sensory fibers.
Sensitive fibers of the spinal nodes take part in the formation of the celiac plexus: the upper cervical (phrenic nerve), 7 lower thoracic and 3 upper lumbar.
From the celiac plexus numerous fibers radiate out like rays of the sun in all directions. In this regard, the plexus is called the “solar plexus”.
A continuation of the celiac plexus are secondary paired and unpaired plexuses along the walls of the visceral and parietal branches of the abdominal aorta. Unpaired plexuses: hepatic, splenic, gastric, pancreatic and superior mesenteric. The fibers of the superior mesenteric plexus, spreading along the branches of the superior mesenteric artery, reach the pancreas, duodenum, jejunum, ileum, cecum, transverse colon.
The second most important in the innervation of the abdominal organs is the broadly looped abdominal aortic plexus, plexus aorticus abdominalis, located on the anterior and lateral surfaces of the abdominal aorta below the renal arteries and is a continuation of the celiac plexus. The lumbar splanchnic nerves, which arise from the lower lumbar nodes of the sympathetic trunk, also participate in its formation.
The inferior mesenteric plexus, plexus mesentericus inferior, departs from the aortic plexus, entwining the artery of the same name and its branches. At the root of this artery there is a rather large node, ganglion mesentericum inferius. The formation of the inferior mesenteric plexus involves the splanchnic lumbar nerves (from the lumbar nodes of the sympathetic trunk), branches of the celiac and superior mesenteric plexuses, which enter it from the intermesenteric plexus, plexus intermesentericus. The fibers of the inferior mesenteric plexus reach the sigmoid, descending and part of the transverse colon. The continuation of this plexus into the pelvic cavity is the superior rectal plexus, plexus rectalis superior, which accompanies the artery of the same name.
The fibers of the mesenteric plexuses come into contact with the intermuscular (plexus myentericus) - Auerbach and submucosal (plexus submucosus) - Meissner's plexuses, located in the walls of the gastrointestinal tract. The myenteric and submucosal plexuses consist of groups of parasympathetic cells (intramural ganglia) connected by bundles of nerve fibers. Preganglionic parasympathetic fibers are interrupted here.
Continuation of the abdominal aortic plexus downwards are the plexuses of the iliac arteries and arteries of the lower limb, as well as the unpaired superior hypogastric plexus, plexus hypogastricus superior, which at the level of the promontory is divided into the right and left hypogastric nerves, forming the inferior hypogastric plexus in the pelvic cavity.
Inferior hypogastric plexus , plexus hypogastricus inferior, or pelvic, plexus pelvinus, one of the largest vegetative plexuses (Fig. 10).
It is located on the sides of the rectum, is a plate on each side, extending from the sacrum to the bladder, from which secondary plexuses extend to the pelvic organs along the branches of the internal iliac artery.
In the lower hypogastric plexus, two sections are distinguished in men: anterioinferior and posterior, and in women there is also a middle section.
The upper part of the anterioinferior plexus innervates the bladder, the lower part in men innervates the prostate gland, seminal vesicles, vas deferens and cavernous bodies.
| Rice. 10. Inferior hypogastric plexus (according to G.F. Ivanov). 1- ureter; 2- plexus hypogastricus superior; 3- plexus hypogastricus inferior; 4-nn. pelvini; 5- rectum. |
In women, the middle section of the inferior hypogastric plexus sends nerve fibers to the genitals. Moreover, its lower part is towards the vagina and clitoris, the upper part is towards the uterus and ovaries. The posterior section of the inferior hypogastric plexus innervates the rectum.
The formation of the inferior hypogastric plexus involves vegetative nodes of the second order (sympathetic), nodes of the third order (periorgan, parasympathetic), as well as nerves and plexuses:
1. Internal sacral nerves, nn.splanchnici sacrales, consisting mainly of preganglionic sympathetic fibers that passed without interruption through the nodes of the sympathetic trunk, as well as sensory fibers from the sacral spinal nodes.
2. Branches of the inferior mesenteric plexus (plexus rectalis superior), consisting mainly of postganglionic sympathetic fibers - processes of cells of the inferior mesenteric ganglion and sensory fibers from the lumbar spinal nodes.
3. Internal pelvic nerves, nn. splanchnici pelvini, consisting of preganglionic parasympathetic fibers - processes of the cells of the intermediate-lateral nuclei of the sacral spinal cord (S2 - S4) and sensory fibers from the sacral spinal ganglia.
Sympathetic preganglionic fibers are interrupted in nodes of the second order, parasympathetic - in the third order. Thus, in the formation of the inferior hypogastric plexus, in addition to autonomic fibers, sensory fibers also take part - processes of cells of the lumbar, sacral and coccygeal spinal nodes.
PARASYMPATHETIC DIVISION
Morphology
The distinction of the autonomous (autonomic) nervous system is due to certain features of its structure. These features include the following:
- focal localization of vegetative nuclei in the central nervous system;
- accumulation of bodies of effector neurons in the form of nodes (ganglia) as part of the autonomic plexuses;
- two-neuronality of the nerve pathway from the autonomic nucleus in the central nervous system to the innervated organ.
The fibers of the autonomic nervous system do not emerge segmentally, as in the somatic nervous system, but from three limited areas of the brain spaced apart from each other: cranial, sternolumbar and sacral.
The autonomic nervous system is divided into sympathetic, parasympathetic and metasympathetic parts. In the sympathetic part, the processes of spinal neurons are shorter, while the ganglion ones are longer. In the parasympathetic system, on the contrary, the processes of spinal cells are longer, those of ganglion cells are shorter. Sympathetic fibers innervate all organs without exception, while the area of innervation of parasympathetic fibers is more limited.
Central and peripheral sections
The autonomic (autonomic) nervous system is divided according to topographical characteristics into central and peripheral sections.
Central department
- parasympathetic nuclei of the 3rd, 7th, 9th and 10th pairs of cranial nerves lying in the brain stem (craniobulbar region).
- sympathetic nuclei located in the lateral horns of the thoracolumbar spinal cord; nuclei located in the gray matter of the three sacral segments (sacral section)[5][6];
Peripheral department
- autonomic (autonomic) nerves, branches and nerve fibers emerging from the brain and spinal cord;
- vegetative (autonomous, visceral) plexuses;
- nodes (ganglia) of the autonomic (autonomous, visceral) plexuses;
- sympathetic trunk (right and left) with its nodes (ganglia), internodal and connecting branches and sympathetic nerves;
- terminal nodes (ganglia) of the parasympathetic part of the autonomic nervous system.
Sympathetic, parasympathetic and metasympathetic divisions
Based on the topography of the autonomic nuclei and nodes, differences in the length of the axons of the first and second neurons of the efferent pathway, as well as the characteristics of the function, the autonomic nervous system is divided into sympathetic, parasympathetic and metasympathetic.
Location of ganglia and structure of pathways
Neurons
nuclei of the central part of the autonomic nervous system are the first efferent neurons on the way from the central nervous system (spinal cord and brain) to the innervated organ. The nerve fibers formed by the processes of these neurons are called prenodal (preganglionic) fibers, since they go to the nodes of the peripheral part of the autonomic nervous system and end with synapses on the cells of these nodes. Preganglionic fibers have a myelin sheath, which makes them whitish in color. They leave the brain as part of the roots of the corresponding cranial nerves and the anterior roots of the spinal nerves.
Vegetative nodes
(ganglia): are part of the sympathetic trunks (present in most vertebrates, except cyclostomes and cartilaginous fish), large vegetative plexuses of the abdominal cavity and pelvis, located in the head and in the thickness or near the organs of the digestive and respiratory systems, as well as the genitourinary system, which are innervated by the autonomic nervous system. The nodes of the peripheral part of the autonomic nervous system contain the bodies of second (effector) neurons lying on the way to the innervated organs. The processes of these second neurons of the efferent pathway, carrying nerve impulses from the autonomic ganglia to the working organs (smooth muscles, glands, tissues), are post-nodular (postganglionic) nerve fibers. Due to the absence of the myelin sheath, they are gray in color. Postganglionic fibers of the autonomic nervous system are mostly thin (most often their diameter does not exceed 7 µm) and do not have a myelin sheath. Therefore, excitation spreads slowly through them, and the nerves of the autonomic nervous system are characterized by a longer refractory period and greater chronaxis.
Reflex arc
The structure of the reflex arcs of the autonomic part differs from the structure of the reflex arcs of the somatic part of the nervous system. In the reflex arc of the autonomic part of the nervous system, the efferent link consists not of one neuron, but of two, one of which is located outside the central nervous system. In general, a simple autonomic reflex arc is represented by three neurons.
The first link of the reflex arc is a sensory neuron, the body of which is located in the spinal ganglia and in the sensory ganglia of the cranial nerves. The peripheral process of such a neuron, which has a sensitive ending - a receptor, originates in organs and tissues. The central process, as part of the dorsal roots of the spinal nerves or sensory roots of the cranial nerves, is directed to the corresponding nuclei in the spinal cord or brain.
The second link of the reflex arc is efferent, since it carries impulses from the spinal cord or brain to the working organ. This efferent pathway of the autonomic reflex arc is represented by two neurons. The first of these neurons, the second in a simple autonomic reflex arc, is located in the autonomic nuclei of the central nervous system. It can be called intercalary, since it is located between the sensitive (afferent) link of the reflex arc and the second (efferent) neuron of the efferent pathway.
The effector neuron is the third neuron of the autonomic reflex arc. The bodies of effector (third) neurons lie in the peripheral nodes of the autonomic nervous system (sympathetic trunk, autonomic ganglia of cranial nerves, nodes of extraorgan and intraorgan autonomic plexuses). The processes of these neurons are directed to organs and tissues as part of organ autonomic or mixed nerves. Postganglionic nerve fibers end on smooth muscles, glands and other tissues with the corresponding terminal nerve apparatus.
Lesson summary on the topic: “Somatic and autonomic divisions of the nervous system.”
Biology 8th grade
Lagoda E.I.
Lesson #57
Topic: “ Somatic and vegetative departments
nervous system».
Tasks:
study the structure of the nervous system by functional division, reveal the relationship between the sympathetic and parasympathetic subdivisions of the autonomic nervous system; develop the ability to work with a textbook and answer questions; cultivate interest in the subject.
Type:
combined.
Method:
explanatory and illustrative.
During the classes.
- Organizing time.
Greetings.
The nervous system is the conductor of our body.
Brain training is about constantly solving high-level problems! The brain should be boiling and worrying!!!
- Checking homework.
Conversation on questions:
- Divisions of the forebrain.
- What parts does the diencephalon consist of?
- What is the significance of the thalamus and hypothalamus?
- The structure of the cerebral hemispheres (corpus callosum, gray and white matter).
- What are gyri and sulci?
- What lobes is the cerebral hemisphere divided into? Why did they get their name?
- How are shares divided?
- What zones of the cerebral cortex are distinguished? Where are they located?
- What are the functional differences between the hemispheres?
- Learning new material.
Well done, you completed your homework check. Let's say "hurray!" and clap our hands three times. Now I will ask you to regulate your heart rate to 60 beats per minute. Can you? How about opening the sphincter of the stomach and allowing food to pass into the duodenum?
No.
Indeed, a person can consciously control the activity of only skeletal muscles, his voluntary movements and speech motor function. But you cannot control salivation, sweat, or gastric juice, blood flow and much more.
Problematic question: Why are skeletal muscles subject to our will, but the heart, blood vessels and other internal organs are not?
put forward hypotheses.
During the evolution of vertebrates, the functions of the nervous system were divided. Based on their functional characteristics, the nervous system is divided into:
• somatic
(animal) and
• vegetative
(autonomous) departments, which is divided into two subdivisions -
sympathetic
and
parasympathetic.
The somatic nervous system provides perception of the surrounding world and regulates movements (including those associated with speech). Vegetative – regulates processes common to animals and plants (hence its name): metabolism, respiration, transport of substances, excretion.
Somatic nervous system
This system is formed by sensory nerve fibers going to the central nervous system from various receptors and motor nerve fibers innervating skeletal muscles. The somatic nervous system has central and peripheral parts. There are 12 pairs of cranial nerves leaving the brain. Each segment of the spinal cord produces one pair of nerves containing sensory and motor fibers. All sensory, or centripetal, fibers enter the spinal cord through the dorsal roots, on which there are thickenings - nerve ganglia. These nodes contain the bodies of centripetal neurons.
Fibers of motor, or centrifugal, neurons leave the spinal cord through the anterior roots - 31 pairs of spinal nerves. Each segment of the spinal cord corresponds to a specific part of the body - a metamer.
Supreme center
The somatic nervous system is
cerebral cortex It is here that ways to satisfy needs are sought, and a plan for future actions matures in the frontal lobe of the cortex.
Teacher:
All activity of the nervous system is of a reflex nature, i.e. consists of a huge number of different reflexes of different levels of complexity.
Let's remember what is called a reflex?
Working with textbook text
Student answers:
A reflex is the body’s response to any external or internal influence involving the nervous system.
That's right, here's another definition:
Reflex
is an adaptive reaction of the body that ensures a subtle, precise and perfect balance of the body with the state of the external or internal environment.
“If you turn off all the receptors, then a person should fall asleep and never wake up”
(I.M. Sechenov).
That. The nervous system works on the principle of reflection: stimulus - response. The authors of the reflex theory are outstanding Russian physiologists. Who?
I.P. Pavlov and I.M. Sechenov.
To implement any reflex, a special anatomical formation is required - a reflex arc.
What it is?
A reflex arc is a chain of neurons along which a nerve impulse passes from the receptor (perceiving part) to the working organ that responds to irritation.
The autonomic nervous system innervates internal organs: the heart, blood vessels, stomach, intestines, kidneys, liver, etc. Is the effect of the autonomous system, for example, on the heart and stomach in this case, the same?
That's right, the heart strengthens its work, and the activity of the stomach, on the contrary, is inhibited.
How is the autonomic nervous system structured to
simultaneously carry out such multidirectional actions?
We work with the text of the textbook Discuss.
Autonomic nervous system
Consists of a central and peripheral part. Its highest organ is the hypothalamus
(lower part of the diencephalon), which also regulates the endocrine system through the pituitary gland (hypothalamic-pituitary axis).
It is divided into two subdivisions: sympathetic and parasympathetic.
Let's look at Fig. in the textbook p.127
1. Functional division of the nervous system. Explanation and recording of the diagram in a notebook.
Nervous system
Somatic department Vegetative department
Regulates operation (autonomous)
skeletal regulates the functioning of internal
organ muscles
Sympathetic Parasympathetic subdivision subdivision
Innervation is the connection of organs and tissues with the central nervous system through nerve fibers.
Brain stem - medulla oblongata, pons, midbrain, diencephalon.
2. Independent work with the textbook, answer the questions in notebooks:
1. Which department is subject to volitional control?
2. Where are the higher centers of the somatic and autonomic parts of the nervous system?
3. Using, fig. and use the textbook text to explain the difference between sympathetic and parasympathetic innervation. (Location of nuclei in the central nervous system - higher centers and nerve ganglia).
4. What is the significance of the vagus nerve?
5. Each organ receives nerve impulses from the sympathetic and parasympathetic subdivisions. What is the operating principle of these subdepartments? What is the significance of double innervation of organs? (Thanks to teamwork, the optimal mode of operation of internal organs is established for each specific situation)
4. Consolidation.
Students call the effect and determine which subdivision carried out the innervation:
5.
Summing up the lesson.
Let's return to the objectives of our lesson, have we completed them?
The students answer.
Grading work in class
- Homework.
Study paragraph 52 and answer questions on page 127 in writing
Physiology
General importance of autonomic regulation
The autonomic nervous system adapts the functioning of internal organs to environmental changes. The ANS ensures homeostasis (constancy of the internal environment of the body). The ANS is also involved in many behavioral acts carried out under the control of the brain, influencing not only physical, but also mental activity of a person.
The role of the sympathetic and parasympathetic divisions
The sympathetic nervous system is activated during stress reactions. It is characterized by a generalized effect, with sympathetic fibers innervating the vast majority of organs.
It is known that parasympathetic stimulation of some organs has an inhibitory effect, while others have an excitatory effect. In most cases, the action of the parasympathetic and sympathetic systems is opposite.
The influence of the sympathetic and parasympathetic departments on individual organs
Influence of the sympathetic department:
- On the heart - increases the frequency and strength of heart contractions.
- On the arteries—[7]dilates the arteries.
- On the intestines - inhibits intestinal motility and the production of digestive enzymes.
- On the salivary glands - inhibits salivation.
- On the bladder - relaxes the bladder.
- On the bronchi and breathing - expands the bronchi and bronchioles, enhances ventilation of the lungs.
- On the pupil - dilates the pupils.
Influence of the parasympathetic department:
- On the heart - reduces the frequency and strength of heart contractions.
- On the arteries - does not affect most organs, causes dilation of the arteries of the genital organs and brain, narrowing of the coronary arteries and arteries of the lungs.
- On the intestines - enhances intestinal motility and stimulates the production of digestive enzymes.
- On the salivary glands - stimulates salivation.
- On the bladder - contracts the bladder.
- On the bronchi and breathing - narrows the bronchi and bronchioles, reduces ventilation of the lungs.
- On the pupil - constricts the pupils.
Neurotransmitters and cellular receptors
The sympathetic and parasympathetic departments have different, in some cases opposite, effects on various organs and tissues, and also cross-influence each other. The different effects of these sections on the same cells are associated with the specificity of the neurotransmitters they secrete and with the specificity of the receptors present on the presynaptic and postsynaptic membranes of neurons of the autonomic system and their target cells.
Preganglionic neurons of both parts of the autonomic system secrete acetylcholine as the main neurotransmitter, which acts on nicotinic acetylcholine receptors on the postsynaptic membrane of postganglionic (effector) neurons. Postganglionic neurons of the sympathetic department, as a rule, secrete norepinephrine as a transmitter, which acts on adrenergic receptors of target cells. On the target cells of sympathetic neurons, beta-1 and alpha-1 adrenergic receptors are mainly concentrated on the postsynaptic membranes (this means that in vivo
they are mainly affected by norepinephrine), and al-2 and beta-2 receptors are on extrasynaptic areas of the membrane (they are mainly affected by blood adrenaline). Only some postganglionic neurons of the sympathetic division (for example, those acting on the sweat glands) release acetylcholine.
Postganglionic neurons of the parasympathetic division release acetylcholine, which acts on muscarinic receptors on target cells.
On the presynaptic membrane of postganglionic neurons of the sympathetic division, two types of adrenergic receptors predominate: alpha-2 and beta-2 adrenergic receptors. In addition, the membrane of these neurons contains receptors for purine and pyrimidine nucleotides (P2X ATP receptors, etc.), nicotinic and muscarinic cholinergic receptors, neuropeptide and prostaglandin receptors, and opioid receptors [8].
When norepinephrine or blood adrenaline acts on alpha-2 adrenoreceptors, the intracellular concentration of Ca2+ ions drops, and the release of norepinephrine at the synapses is blocked. A negative feedback loop occurs. Alpha-2 receptors are more sensitive to norepinephrine than to epinephrine.
When norepinephrine and epinephrine act on beta-2 adrenergic receptors, the release of norepinephrine usually increases. This effect is observed during normal interaction with the Gs protein, during which the intracellular concentration of cAMP increases. Beta two receptors are more sensitive to adrenaline. As adrenaline is released from the adrenal medulla under the influence of norepinephrine from the sympathetic nerves, a positive feedback loop occurs.
However, in some cases, activation of beta-2 receptors can block the release of norepinephrine. It has been shown that this may be a consequence of the interaction of beta-2 receptors with Gi/o proteins and their binding (sequestering) of Gs proteins, which, in turn, prevents the interaction of Gs proteins with other receptors [1].
When acetylcholine acts on muscarinic receptors of sympathetic neurons, the release of norepinephrine in their synapses is blocked, and when it acts on nicotinic receptors, it is stimulated. Because muscarinic receptors predominate on the presynaptic membranes of sympathetic neurons, activation of the parasympathetic nerves typically reduces the level of norepinephrine released from the sympathetic nerves.
Alpha-2 adrenergic receptors predominate on the presynaptic membranes of postganglionic neurons of the parasympathetic department. When norepinephrine acts on them, the release of acetylcholine is blocked. Thus, the sympathetic and parasympathetic nerves mutually inhibit each other.
Human autonomic nervous system, neurons and synapse (Diagram, Table)
The autonomic nervous system (or autonomic nervous system) regulates the functioning of internal organs, glands, blood vessels and the heart. Below is a diagram of the structure of the human autonomic nervous system.
Scheme of the structure of the human autonomic nervous system
Divisions of the autonomic nervous system: I - cervical; II - chest; III - lumbar; IV - sacral sections of the spinal cord; V - borderline sympathetic trunk.
Action of the autonomic nervous system
| Organs | Stimulation of the sympathetic nervous system | Stimulation of the parasympathetic nervous system |
| Heart | Increases frequency and strength of contractions | Slows down and weakens contractions |
| Arteries | Taper; blood pressure increases | Expand; blood pressure decreases |
| Intestines | Peristalsis decreases | Peristalsis increases |
| Liver | Bile ducts relax | Bile ducts contract |
| Sweat glands | Increase secretion | Does not affect |
| Salivary and lacrimal glands | Decreased secretion | Increased secretion |
| Pupil of the eye | Expanding | Tapers |
| Bronchi | Expand; breathing becomes easier | Taper |
| Muscles that lift the hair | Shrinks, hair “stands on end” | Relax |
| Amount of sugar in blood | Increases | Decreases |
| Oxygen consumption | Increases | Decreases |
Structure and types of neurons
Nervous tissue is divided into neurons (nerve cells) and neuroglia (supporting, Schwann cells).
Neurons are responsible for perception, conduction, and processing of information. Neuroglia are responsible for supporting, protecting, and feeding neurons.
The figure below shows a diagram of the structure of a motor (multipolar) neuron.
| A neuron consists of a nerve ending, direction of the nerve impulse, interception of Ranvier, myelin sheath, axon, Schwann cell, nerve cell body, nucleus, dendrum. The diameter of the neuron body is 15-150 microns (0.001 mm). Axon length – up to 1 m |
Main types of neurons
| Types of neurons | Functions of neurons |
| Types of neurons by function | |
| Sensitive (sensory, afferent) | Conduct information about sensation (impulse) from the surface of the body and internal organs to the brain |
| Associative (insertion, switching, linking) | Analyze information and develop solutions |
| Motor (efferent, effector) | Conduct impulses (commands) from the brain and spinal cord to all working organs |
| Types of neurons by structure | |
| Unipolar, pseudounipolar, Purkinje cell (in the cerebellum), bipolar | |
Synapse and its structure
A synapse is a place of contact (approachment) of nerve cells with each other and with other cells (muscle, glandular and others).
A synapse consists of an axon (this is a nerve fiber), mitochondria, presynaptic and postsynaptic membranes, synaptic vesicle, reuptake, synaptic cleft, receptors for transmitter and transmitter release.
The figure below shows a diagram of the structure of an interneuron synapse.
When the impulse reaches the end of the axon, a special substance - a transmitter (acetylcholine, norepinephrine, dopamine, histamine, etc.) is transmitted through the synaptic cleft to the axon, dendrite, the body of another neuron or other cells of the body. The transmitter causes excitation or inhibition in the neighboring cell. One nerve cell can form up to 10,000 synapses with neighboring cells.
_______________
Source of information: Rezanova E.A. Human biology. In tables and diagrams./ M.: 2008.
Development in embryogenesis
- Development of the peripheral (somatic) and autonomic nervous system.
The peripheral (somatic) and autonomic nervous system develops from the outer germ layer - the ectoderm. Cranial and spinal nerves in the fetus are formed very early (5-6 weeks). Myelination of nerve fibers occurs later (for the vestibular nerve - 4 months; for most nerves - at 6-7 months).
Spinal and peripheral autonomic ganglia are formed simultaneously with the development of the spinal cord. The starting material for them is the cellular elements of the ganglion plate, its neuroblasts and glioblasts, from which the cellular elements of the spinal ganglia are formed. Some of them are shifted to the periphery to the localization of the autonomic nerve ganglia
Notes
- Brief medical encyclopedia.
- Biologist's Dictionary. (unavailable link)
- For example, in the book “Human Physiology / Ed. V. M. Pokrovsky, G. F. Korotko. - M.: Medicine, 1997. - T. 1 - 448 p.; T. 2 - 368 pp.”
- Romer A., Parsons T. Anatomy of vertebrates. - T. 2. - P. 260.
- I. Espinosa-Medina, O. Saha, F. Boismoreau, Z. Chettouh, F. Rossi.
The sacral autonomic outflow is sympathetic (English) // Science. — 2016-11-18. - Vol. 354, iss. 6314. - P. 893–897. — ISSN 1095-9203 0036-8075, 1095-9203. — DOI:10.1126/science.aah5454. - The sacral division of the autonomic nervous system is sympathetic. Retrieved February 21, 2021.
- Brin V.B. et al. Fundamentals of human physiology in 2 volumes. Textbook for higher educational institutions. Ed. B. I. Tkachenko. St. Petersburg, 1994. T.1 - 567 p. T.2 - 413 p.
- Stefan Boehm, Sigismund Huck. Receptors controlling transmitter release from sympathetic neurons in vitro // Progress in Neurobiology. — Volume 51, Issue 3, February 1997, Pages 225-242.
- G. Ross, C. Ross, D. Ross. Entomology. - M.: Mir, 1985. - P.109.