Hemifacial spasm
is a condition characterized by painless, involuntary clonic or tonic contractions of the facial muscles innervated by the ipsilateral facial nerve on one side of the face, usually the left. People have no control over these spasms, which can continue even during sleep. Hemifacial spasm is usually painless and considered harmless. Hemifacial spasm is more common in middle-aged women and Asian people. This rare condition affects approximately 11 in 100,000 people.
Hemifacial spasm is different from other nerve and muscle conditions affecting the face because it tends to affect only one side of the face. However, there are differences between those typical of hemifacial spasm and other forms of the disease.
Research shows that:
- 62% of cases are caused by a vessel putting pressure on the facial nerve;
- 18% had a tic that mimicked a hemifacial spasm;
- 11% were caused by Bell's palsy;
- 6% were the result of facial nerve injury;
- 2% were due to hereditary causes;
- less than 1% of cases were caused by damage to the nerves or circulatory system of the brain.
Photo : Laskawi R. The use of botulinum toxin in head and face medicine: an interdisciplinary field //Head & face medicine. – 2008. – T. 4. – No. 1. – P. 5.
Facial hyperkinesis
Facial hemispasm and paraspasm, blepharospasm are diseases associated with uncontrolled contraction of facial muscles. They are very similar to neuropathy, neuritis, and facial nerve paresis.
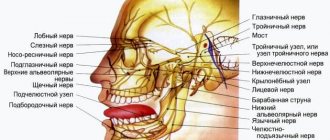
Facial muscle control is structured as follows:
- Nerve cells of the cortex and subcortical nuclei of the brain send nerve impulses to the brain stem, to the control centers of the facial nerve;
- These centers distribute impulses along the nerve fibers and send them along the nerve, like an electrical cable, directly to the facial muscles;
- Each tiny nerve fiber causes its own microscopic section of muscle to contract.
Causes of facial hyperkinesis:
- An error in the functioning of the subcortical nuclei of the brain, as a result of which excess uncontrolled nerve impulses are sent to the facial muscles, which lead to spasm;
- Excessive stimulation of the facial nerve centers in the brain stem;
- Irritation of the facial nerve itself after it leaves the brain.
In the first and second cases, this is the result of damage to the nucleus or center due to neuroinfection, multiple sclerosis, blood supply deficiency or tumor. In the third case, the disease occurs even with slight compression of the root of the facial nerve in the area of its exit to the base of the brain by an altered vessel (entanglement of the nerve by an artery), a tumor, or compression in the thickness of the parotid salivary gland in some of its diseases.
Even doctors often confuse facial hyperkinesis with neuropathy, neuritis of the facial nerve. We will definitely understand the causes of the disease and provide the necessary treatment.
Hemifacial spasm (HFS) is a disorder characterized by painless, involuntary unilateral tonic or clonic contractions of the facial muscles innervated by the ipsilateral facial nerve [106, 108].
In 1875, F. Schultze [83] described the clinical picture of HFS, the cause of which was an aneurysm of the left vertebral artery. A detailed description of the clinical picture of HFS was made in 1894 by the French neurologist E. Brissaud [19]. Already in the 19th century, HFS was considered as a separate nosological unit and stood out from the group of other facial hyperkinesis. Over the past 100 years since the publication of classical descriptions of HFS, the etiology of this disease has been identified and effective treatment methods have been developed.
In 2004, N. Tan et al. [99] showed 203 family doctors a video recording of a patient suffering from HFS: only 9.4% of them were able to correctly diagnose and 46.3% of doctors were able to correctly choose the management tactics for such a patient. Primary care doctors are poorly informed about this disease and cannot prescribe adequate treatment and refer the patient to the appropriate specialist. In the modern Russian-language scientific literature there is a limited number of publications devoted to the diagnosis and treatment of HPS [4, 9]. In modern manuals on neurology and neurosurgery, ideas about etiology and pathogenesis are not fully reflected.
In classic cases, an attack of HFS begins with rare contractions of the orbicularis oculi muscle, then, gradually progressing, the spasm affects the entire half of the face, the frequency of muscle contractions increases and reaches such an extent that the patient cannot see with the eye of the affected side (typical HFS). With atypical HFS, the attack begins with contraction of the cheek muscles, then the spasm spreads up the face [50, 80]. Attacks of spasms occur spontaneously and can persist even during sleep; they are provoked by overwork, stress, and anxiety [31].
In 1905, the neurologist J. Babinski described the paradoxical synkinesis of the facial muscles during HFS: “On the side of the spasm of the m. orbicularis oculi
contracts, the eye closes, at this time the inner part
of m.
frontalis on the affected side also contracts, which leads to the raising of the eyebrow during the closure of the palpebral fissure” [15]. J. Devoize [28] called this symptom “the other Babinski’s sign” (“another Babinski’s symptom” to distinguish it from Babinski’s symptom when the pyramidal tract is affected); some authors consider it pathognomonic for HPS. The described synkinesis is characteristic of HFS and does not occur in other facial hyperkinesis [90].
The disease usually first appears between 40 and 50 years of age [14, 31]. HFS is a chronic disease, the rate of spontaneous remission is less than 10% [31]. Months or years after the onset of the disease, patients may develop moderate paresis of the facial muscles on the affected side [51]. Muscle weakness is detected in 47% of cases in the muscles of the eyelids and in 77% when assessing the strength of other facial muscles [34]. Bilateral HPS is extremely rare (0.6-5%) [94, 108].
Other cranial nerves may be involved in the pathological process. HPS is often combined with dysfunction of the auditory nerve - an anomaly of the acoustic reflex of the middle ear is observed in 50% of patients with hemispasm [71], hearing loss to varying degrees is detected in 15% [31]. Sometimes HFS is accompanied by low-pitched noise in the ipsilateral ear, this is due to the involvement of the m.stapedius
, which contracts synchronously with the facial muscles [84]. In 5% of cases, HPS can be combined with trigeminal neuralgia [63, 79, 108]. Cushing called this syndrome "painful tic convulsif" - "painful facial tic." A combination of HPS with blepharospasm has been described [91].
According to the Minnesota Epidemiological Study [14], conducted in 1960-1984, the prevalence rate of HFS was 7.4 per 100,000 male population and 14.5 per 100,000 female population; The mean annual incidence rate, age-standardized for the white population in the United States in 1970, is 0.74 per 100,000 for men and 0.81 for women. The incidence rate and prevalence rate of the disease are highest in the age group from 40 to 79 years. Note that this study included patients with both primary and secondary HPS. According to N. Nilsen et al. [76], in Norway the prevalence of HFS is 9.8 per 100,000 population. A higher incidence of HFS has been noted [12] among people of the Mongoloid race compared to Caucasians. Such differences may be associated with features in the structure of the skull, in particular the size of the posterior cranial fossa [54]. However, epidemiological studies have not been conducted to identify the prevalence of HPS in people of the Mongoloid race.
Despite the fact that the clinical picture of HPS was described at the end of the 19th century, the cause of this disease remained a mystery to researchers for many years. In the 50-60s of the 20th century, there was an active discussion about the “peripheral” or “central” origin of GFS.
R. Siekert [86] and E.P. Fleiss [7] described symptomatic HFS in tumors of the tympanojugular glomus. In the above observations, richly vascularized glomus tumors affected the facial nerve, which resulted in the development of HFS. S.N. Davidenkov [3] and E.P. Fleiss [7] believed that facial hemispasm is of a peripheral nature, and there are no symptoms of central nervous system damage. R. Wartenberg [107] studied the “central” genesis of HPS. According to his hypothesis, HFS is based on changes in the functional state of the nucleus of the facial nerve and supranuclear structures. However, all these concepts did not make it possible to explain the features of the clinical picture of HFS and to develop effective treatment methods on their basis.
In 1947, E. Camblell and C. Keedy [20], and then E. Lain and P. Nyrac [58] suggested that the cause of hemifacial spasm is compression of the facial nerve by ectatic vessels of the base of the brain. In 1962, this guess was confirmed during surgical exploration of the posterior cranial fossa in patients with HFS [35, 36].
The priority in the development and popularization of the theory of microvascular compression as a cause of neurovascular compression syndromes of cranial nerves (trigeminal neuralgia, HPS, glossopharyngeal neuralgia, spastic torticollis) belongs to the American neurosurgeon P. Jannetta [47-49, 51]. The theory of microvascular compression, in his opinion, is based on a neurovascular conflict - a “conflict” between the root of the cranial nerve at the site of its entry and exit from the brain stem with the adjacent vessel.
The main pathogenetic factor in the development of microvascular compression syndromes of the cranial nerves is the mechanical effect of a pulsating vessel on the nerve trunk with the subsequent spread of pathological impulses and the development of its paroxysmal functional activity (paroxysmal facial pain - when affecting the trigeminal nerve, paroxysmal contraction of the facial muscles - when affecting the facial nerve) [49]. Compression factors are usually atherosclerotic aberrant or ectatic arteries. A conflict of a nerve with an arterial vessel (anterior or posterior inferior cerebellar arteries, vertebral or basilar arteries) is more often observed; a conflict of a nerve with a venous vessel is rarely observed [64].
With the development of neuroimaging methods, the introduction of surgical microscopy into widespread practice and, as a consequence, the improvement of surgical techniques, compression of the facial nerve by ectatic vessels began to be considered the main cause of HFS, and the concept of neurovascular conflict in the genesis of microvascular compression syndromes began to gain more and more supporters [1, 2 , 5, 6, 8, 29]. According to P. Jannetta, compression of the nerve occurs in the zone of entry and exit of the nerve root (REZ - root exit/entry zone). It is important that in the zone of root exit, thinner central glial myelin transforms into thick, peripheral “Schwann myelin” (this anatomical feature was first described by H. Obersteiner and E. Redlich in 1894 - the Obersteiner-Redlich zone) [77]) .
In typical HPS, the vessels compress the anterocaudal region of the VII/VIII nerve complex, and in atypical HPS, compression is localized in the posterostral region. The features of the neurovascular conflict zone explain the differences in the clinical picture of typical and atypical HPS [50]. The contact of vessels with the exit zone of the vestibular nerve root leads to the appearance of complaints of dizziness in the clinical picture, and when the vessels come into contact with the exit zone of the cochlear nerve root, complaints of hearing loss and tinnitus appear [50]. Combined compression of the roots of the V and VII nerves is possible; in this case, HPS will be accompanied by facial pain (a combination of trigeminal neuralgia and HPS) [79].
Although the generally accepted cause of neurovascular conflict is vascular compression, a number of studies have been published that provide data that do not fit into the classical theory of P. Jannetta. It should be noted that the subject of discussion is the possible localization of areas of neurovascular conflict, and not the concept of neurovascular compression at its core, which is recognized by most researchers.
H. Ryu et al. [81]. distal portion. There are several descriptions [33, 72, 109] of cases of identifying a zone of neurovascular conflict outside the zone of root exit.
D. De Ridder et al. [27] suggested that the frequency of microvascular compression syndromes of cranial nerves in the population depends on the length of the central segment of each of them. Since the central segment of the trigeminal nerve has the greatest length [59] and is then followed in descending order by the facial, glossopharyngeal and vestibulocochlear nerves, accordingly, trigeminal neuralgia will most often occur, and compression of the vestibular nerve will occur less frequently. Clinically significant is compression of the nerve throughout the “central” segment (the segment of the nerve covered with “central” myelin), and not just compression in the REZ zone [27]. A similar point of view was previously expressed by T. Leclerq [61] and A. Moller [66].
This hypothesis can be confirmed by the data of M. Sindou et al. [87]. These investigators analyzed the results of 579 microvascular decompressions for trigeminal neuralgia. It turned out that compression in the area of the root exit occurred only in 52.3% of cases, in its middle portion - in 54.3%, in the area of the Meckel cavity - in 9.8%.
Currently, the theory of microvascular compression makes it possible to explain the clinical and neurophysiological features of HFS. Based on this concept, an effective method for treating HFS has been developed—microvascular decompression surgery. This fact, like no other, testifies in favor of the theory developed by P. Jannetta. Undoubtedly, it requires further development and addition.
Some authors believe that neurovascular conflict is one of the factors in the genesis of HFS and other microvascular compression syndromes. Thus, A. Kuroki and A. Moller [57] consider primary nerve injury, accompanied by local demyelination, in combination with vascular compression in this area as a combination of trigger factors in the development of hemifacial spasm. These judgments also complement the theory of microvascular compression and do not contradict it.
Some studies highlight the association between hypertension and HPS. Arterial hypertension is considered a risk factor for the occurrence of HPS, since hypertension contributes to the progression of atherosclerotic changes in blood vessels, which leads to their ectasia and pathological tortuosity, predisposing to the development of vascular compression. In turn, it is assumed that compression of the ventrolateral parts of the medulla oblongata by ectatic vessels can lead to arterial hypertension [25, 52, 76, 93].
The development of MRI and MR angiography has provided additional evidence in favor of the theory of neurovascular conflict, since direct visualization of the nerve root and the vessel compressing it has become possible. High-resolution MRI and MR angiography are quite sensitive methods for detecting neurovascular conflict [10, 38, 92].
Sometimes HPS is caused by space-occupying formations of the cerebellopontine angle (tumors, vascular malformations, aneurysms) [24, 100, 104]. Space-occupying formations alter neurovascular relationships, leading to displacement of blood vessels and their contact with nerve roots, or have a direct compressive effect on the facial nerve. Hemispasm can also be caused by multiple sclerosis [101], lacunar infarction in the pontine region [105], inflammatory diseases of the middle ear [60], and deformations of the skull bones (for example, in Pagett's disease) [45].
Thus, depending on the etiology, HFS can be divided into primary
, the causes of which are neurovascular conflict in the area where the nerve exits the trunk, and secondary - caused by other pathological processes. The division of HPS into primary and secondary is currently generally accepted in the literature [22, 25, 108]. The use of the term “idiopathic HFS” is incorrect, since the cause of the spasm has been established.
Currently, there are two main hypotheses for the pathogenesis of HPS. The central hypothesis explains the symptoms of HFS by changes (hyperexcitability) of the nucleus of the facial nerve [67, 68], the peripheral one - by damage to the myelin sheath and ephaptic transmission of nerve impulses between different nerve fibers [74, 75].
V. Nielsen in 1984 [74, 75] put forward the hypothesis of ephaptic or ectopic transmission: as a result of nerve compression and subsequent demyelination, “false” synapses are formed, through which ectopic activity can be triggered due to mechanical irritation in adjacent nerve fibers. He showed that this mechanism underlies the electrophysiological phenomenon, the so-called abnormal muscle response in HPS. This phenomenon disappears after decompression of the facial nerve using microvascular decompression [51, 74, 75].
A. Moller and P. Jannetta [67-69] believe that the main pathological processes in HFS occur in the nucleus of the facial nerve in response to peripheral stimuli (vascular compression). K. Digre and J. Corbett [29] put forward an alternative hypothesis, according to which, as a result of compression, aberrant regeneration occurs in the facial nerve, which leads to the restructuring of axonal fibers.
In the 70-80s, CT and MRI were considered as auxiliary diagnostic methods and served mainly to exclude organic pathology (tumors, vascular malformations, aneurysms), which could cause secondary HPS, or to identify compressing vessels of large diameter (for example, ectatic vertebral arteries) [30, 89, 100]. With the advent of high-field MR tomographs with high resolution and the subsequent development of special software (3D reconstruction programs), the capabilities of the method have expanded significantly. The possibility of non-invasive visualization of neurovascular conflict has become possible [10, 38, 92].
Numerous studies have shown that MRI and high-resolution MR angiography are quite sensitive methods for detecting neurovascular conflict [39, 92]. Y. Nagaseki et al. [73] demonstrated that detection of small-diameter vessels (anterior and posterior inferior cerebellar arteries) was possible in 75.9%, and large-diameter vessels (vertebral artery) in 100%; there were no false-negative results. The authors emphasize that the diagnostic capabilities of MRI depend on the correct projection (oblique sagittal MRI projection) and the correctly selected pulse sequence.
At the present stage of development, MRI in most cases makes it possible to identify the cause of HFS (tumor, aneurysm, vascular malformation in the area of the cerebellopontine angle, focus of demyelination, focus of lacunar infarction) and visualize the neurovascular conflict, i.e. distinguish between secondary and primary GFS.
Although the key to diagnosing HPS is primarily a neurological examination, electromyography (EMG) also provides a lot of useful information. There is evidence that HPS has pathognomonic electromyographic patterns [32, 69]. R. Hjorth and R. Willison [43] described two main EMG patterns in HPS. The first is short, quick tics (twitching), which are simultaneously observed in various muscle groups of half the face and are often accompanied by blinking movements. The EMG records isolated bursts of repeated high-frequency discharges. Each series includes from 2 to 40 discharges from one motor unit. The intervals between series of discharges vary greatly, their frequency is 200-250 Hz, but can reach 350-400 Hz. Attenuation of the motor unit action potential during a volley of discharges is often observed. The second characteristic, but less common type of movement abnormality is prolonged, irregular, fluctuating muscle contractions, which lead to forced closure of the eye for several seconds. Despite the fact that in this situation it is not possible to record the signal from individual motor units in isolation, the researchers were able to establish that the excitation of the motor units occurred irregularly and with a lower amplitude than in the first pattern [43].
With HFS, another electroneurophysiological phenomenon can be observed: with electrical stimulation of one of the branches of the facial nerve, contraction of the facial muscles innervated by other branches of the facial nerve occurs, for example, with stimulation of the temporal branch, contractions of m. mentalis
. This phenomenon is called the abnormal muscle response phenomenon or the lateral spread phenomenon [67, 68]. It is believed that this effect is due to the cross-transmission of antidromic activity that occurs as a result of microtrauma to the nerve during a neurovascular conflict [74, 75]. This phenomenon is used not only for diagnosing HPS, but also for intraoperative monitoring when performing MIA [39, 51, 78, 88].
HFS should be distinguished from a number of other facial hyperkinesis [29, 108]. R. Blair and H. Berry [18] cite the following diseases and syndromes with which a differential diagnosis must be made: essential blepharospasm; facial myokymia (pseudofasciculations), including tic (psychogenic facial spasm), focal cortical seizures affecting the facial muscles, aberrant regeneration of nerve fibers after facial nerve injury or Bell's palsy, delayed (tardive) dyskinesia (as a complication of taking antipsychotics).
Some authors [98, 102] consider it possible to include Meij’s syndrome (a combination of blepharospasm and oromandibular dystonia) in this list.
To treat HFS, drugs from different pharmacological groups are used: carbamazepine [11], clonazepam [41], gabapentin [23], levetirace [26], baclofen [82]. However, their effect was studied in small samples of patients, without placebo control. Therefore, the long-term effect of such treatment seems rather doubtful [98]. Due to the fact that the pathology in question requires constant use of medications in fairly high doses, it is necessary to take into account their side sedative effect, which cannot but affect the quality of life of patients.
Botulinum toxin type A has proven itself well in the treatment of HFS [17, 95]. The effectiveness of this drug was established by W. Jost and A. Kohe [53] in a study conducted taking into account the principles of evidence-based medicine: the effect of botulinum toxin was studied in large samples (up to 2000 patients) in a double-blind, placebo-controlled study. The drug is administered subcutaneously or intramuscularly into the affected muscles. The use of botulinum toxin in the early stages of the disease is especially promising.
However, injections must be performed on average every 3-4 months [106], the cost of the drug is quite high, and it requires strict adherence to storage rules. The effectiveness of treatment (significant regression of symptoms) is observed in 70-75% [98, 110]. In 2-14%, complications such as ptosis, keratitis, diplopia, epiphora (retention lacrimation), drooling, strabismus (strabismus) are observed [53, 55]. A. Wang, J. Jancovic [106], observing 110 patients, described transient paresis of the facial muscles (23%), ptosis (15%). Assessing the results of treatment with botulinum toxin, one can still note their lack of durability, and the high cost limits its use [78, 98].
Attempts at surgical treatment of HFS were made at the beginning of the 20th century. Before the advent of microvascular decompression methods, treatment of HFS was limited to applying severe or moderate therapeutic destructive effects to the peripheral part of the facial nerve or parts of the nerve in the region of the cerebellopontine angle. Complete or partial destruction of the peripheral part of the facial nerve or its branches was performed surgically or by injection of glycerol or ethanol [40], but instead of nerve spasm, its paresis sometimes developed [65]. Moreover, after 3-6 months, a recurrence of spasm usually occurred due to nerve regeneration. Myectomy was also performed - unilateral resection of m. orbicularis oculi
and
m.
corrugator supericiliaris [37]. Currently, extracranial destructive procedures are practically not used due to their low effectiveness [46].
In 1960, W. Gardner [36] published a case of recovery from HFS after neurolysis of the facial nerve in the area of the internal auditory canal. By 1962, he had experience in the surgical treatment of 19 patients, all of whom had undergone neurolysis of the VII nerve in the region of the cerebellopontine angle. In 7 cases, compression of the facial nerve by the loop of the anterior inferior cerebellar artery or the internal auditory artery was detected [36]. Later, W. Scoville [85] successfully treated HFS in one patient by displacing the peripheral artery from the facial nerve in the area of the cerebellopontine angle, but the patient lost hearing after the operation.
P. Jannetta developed and popularized microvascular decompression for neurovascular syndromes. He performed his first decompression during HFS in February 1966, and in 1970 his first article on this topic was published [47]. The operation consists of installing a protector (Teflon is usually used) between the conflicting vessel and the nerve, which eliminates the chain of pathological impulses. In 1999
M. McLaughlin, P. Jannetta et al. in a corresponding publication [64], they summarized more than 30 years of experience in performing microvascular decompression for neurovascular syndromes, citing the results of 4400 operations.
Other scientific centers have also accumulated sufficient material on the use of microvascular decompression in HFS, allowing us to assert that this method is more effective in the treatment of primary facial spasm, the cause of which is a neurovascular conflict, reaching 86-93% [1, 13, 16, 21, 56 , 64]. F. Barker et al. [16] reported complete regression of HFS symptoms in 86% of 612 patients, partial effect was achieved in 5% of cases with an average follow-up period after therapy of 8 years; according to long-term results obtained by R. Illingworth et al. [44] (average follow-up period 8 years), the effectiveness of the procedure was 92.2% (in 83 out of 86 patients).
The recurrence rate of HFS after microvascular decompression, according to various authors [103, 108, 109], is up to 20%. In a work devoted to the study of relapses of HFS after microvascular decompression, J. Tew and P. Troy [103] showed that if a patient does not have a relapse after surgery for 2 years, then the probability of developing a recurrent spasm is less than 1%, the relapse rate in their work is approaching 7%. The most common complications after such an intervention are permanent or transient dysfunction of the vestibulocochlear and facial nerves. Complete loss of function of the vestibulocochlear nerve occurs in 1.6-2.6%, moderate hearing loss in 0.6-0.7% of cases [16, 64]. Paresis of the facial nerve in various series occurs in 3.4-4.8%; As a rule, facial nerve dysfunction is transient, and when assessing the long-term results of microvascular decompression, in most cases, complete regression of prosoparesis is noted [78]. To avoid dysfunction of the VIII nerve, intraoperative monitoring of acoustic brainstem evoked potentials is used [70, 88]. Less common are dysfunction of the caudal group of cranial nerves, infectious complications, wound liquorrhea, hemorrhages in the trunk and cerebellum. Works have been published to evaluate complications in large samples of patients. When analyzing the results of 4400 microvascular decompressions for neurovascular compression syndromes of the cranial nerves, M. McLaughlin, P. Jannetta et al. [64] noted the following frequency of complications: in the group of patients operated on before 1990, cerebellar damage 0.87%, hearing loss 1.98%, liquorrhea 2.44%. In the group of patients operated on after 1990, the number of complications decreased: 0.45% of patients had cerebellar damage, 0.8% had hearing loss, and 1.85% had wound liquorrhea [21, 64]. It should be noted that for surgeons who perform a large number of operations, the incidence of complications is minimized [21, 64, 98].
The basis for assessing the results of treatment for HFS is primarily a clinical assessment of the regression of hemispasm symptoms. In this regard, a gradation of relevant changes was proposed. For example, V. Marneffe et al. [62] suggest that the result be considered “excellent” if the spasm completely disappears, “good” if the regression is more than 80%, “satisfactory” if the regression is from 20 to 80%, and the result is considered “unsatisfactory” if the symptoms are relieved by less than 20%. . T. Iwakuma et al. [46], P. Jannetta [49, 51], R. Auger et al. [13] used a 6-level scale to evaluate the results, highlighting “excellent”, “good”, “satisfactory”, “unsatisfactory”, “poor” and “recurrent”. In all rating systems, “excellent” is the result of complete disappearance of symptoms, “good” is the disappearance of 75-80%. The goal of treatment is, of course, to achieve “excellent” or “good” results.
Despite the fact that HFS does not pose an immediate threat to the lives of patients, it significantly worsens its quality, limiting their professional and social activity, causing psychological discomfort [51, 96]. More than 75% of patients experience discomfort due to their disease, 15-65% suffer from depression. HFS impairs vision in 60% of patients and interferes with work activity in 36% of patients [12].
To assess the quality of life of patients with HFS, both “general” (SF-36) and special Hemifacial spasm scales (HFS-7 and HFS-8) are used. The validity and reliability of the latter was shown in the works of E. Tan et al. [97]. The HFS-7 and HFS-8 have 7 or 8 questions and are very quick to complete. K. Heuser et al. [42] demonstrated the use of this tool to evaluate the effectiveness of microvascular decompression for HFS and found that this procedure significantly improved the quality of life of patients.
Thus, the cause of primary HPS is compression of the facial nerve in the area where it leaves the trunk by vessels, secondary HPS is most often caused by pathological processes in the area of the cerebellopontine angle. The diagnosis of HFS is established clinically and using these additional methods (EMG, MRI). Differential diagnosis must be made with a number of other facial hyperkinesis. The basis of modern ideas about the pathogenesis of primary HFS is the theory of microvascular compression, the cornerstone of which is the concept of neurovascular conflict. The most effective treatment for primary HFS is microvascular decompression of the facial nerve. Methodologically, this procedure is well developed. The second most effective treatment method is botulinum toxin injections. This method has a number of disadvantages, but it may be preferred by patients who categorically do not accept surgical treatment methods. The determining criteria in assessing the results of treatment for HFS are the degree of clinical regression of hemispasm and improvement in the quality of life of patients.
Examination for facial hyperkinesis
The success of treatment directly depends on an accurate diagnosis of the location and cause of damage to the pathways and brain centers of the facial nerve. Therefore, we carefully examine each patient. Your doctor will determine the cause of excessive stimulation of the facial muscles, and based on the data obtained, select the most effective treatment.
MRI and X-ray computed tomography of the brain and facial skull. On tomograms, especially if they are performed with preliminary contrast, the brain centers of the facial nerve and its area of exit (root) to the base of the brain, blood vessels, and skull bones are visible. They help to see the cause of compression of the facial nerve root and evaluate the structure of the salivary glands. Circulatory disorders, cysts and tumors are easily recognized.
Blood tests to check for infections and biochemical changes that damage the brain and facial nerve. The suspicion of the presence of a neuroinfection and its activity can be easily verified using a blood test.
Electromyography, Blink reflex - electrophysiological techniques based on measuring the electrical potentials of the facial muscles. They help assess the function of impulse transmission along the facial nerve, the degree of its impairment, judge the effectiveness of treatment, the presence of complications, and help in choosing the correct treatment tactics.
Treatment
At the moment, there are several methods of treating hemifacial spasm. Competent and timely therapy can partially or completely block the manifestations of this pathology.
Medication method
Gabapentin capsules are taken orally whole before, after or during meals, with plenty of water.
It is based on taking drugs belonging to various pharmacological groups. Most often, patients with clonic hemifacial spasm are prescribed medications such as Clonazepam, Gabapentin, Baclofen, etc.
This technique has quite significant drawbacks, and therefore it is usually not considered as a serious treatment for involuntary spasms of the facial muscles. Among the disadvantages of this treatment it should be noted:
- No long-term effect.
- A large number of side effects.
- Insufficient statistical indicators.
Botulinum toxin
Botulinum toxin is injected directly into the affected area. According to research results, the technique has shown high efficiency in the treatment of both initial and advanced stages of the disease. The disadvantages of the technique are as follows:
- Therapy is expensive and requires systematic repetition.
- If the patient has ophthalmological problems, then the use of the drug is contraindicated for them.
- This procedure is also not performed for allergy sufferers.
To date, treatment with botulinum toxin has yielded positive results in ¾ of patients with facial hemispasm.
How to stop facial hyperkinesis. Administration of Botulinum toxin A
Botulinum toxin A (Botox, Dysport) is a means of reducing the excitability of the muscles involved in hyperkinesis. The drug is one of the most convenient options for the symptomatic treatment of spasms of the muscles of the face and eyes, and other hyperkinesis. We inject Botulinum Toxin A using a syringe with a very thin needle directly into the affected muscle, after which the muscle stops engaging in tics or other hyperkinesis. The effect develops within 3-5 days and lasts up to 4-8 months. During this time, a course of treatment of the causes of the disease and rehabilitation procedures (massage, gymnastics, physiotherapy, psychotherapy, cosmetic procedures) are carried out.
Symptoms of hemifacial spasm
The first sign of spasm is usually twitching of the left eyelid muscles. These spasms can be severe enough to cause the eyes to close and watery eyes. If the condition is left untreated, hemifacial spasm symptoms may become more severe and affect more and more facial muscles. The spasm can affect the muscles of the mouth and pull them to one side. Some people may develop spasms on both sides of the face. Pain and “clicking” in the ear and hearing loss may be symptoms of this condition. Sometimes hearing loss also occurs.
Treatment of facial muscle spasms
Depending on the detected causes of the disease, your doctor will choose the appropriate combination from a wide range of treatment methods:
- Prescription of drug therapy aimed at reducing irritation of the facial nerve root, restoring blood supply, eliminating infection if it is detected;
- Injection of Botulinum toxin A into muscles subject to involuntary contractions;
- Acupuncture, massage, gymnastics;
- Special neuropsychological gymnastics, which allows you to normalize the relationships between different parts of the brain;
- Carrying out neurosurgical intervention to eliminate contact between the modified vessel and the root of the facial nerve (microvascular decompression) or remove the tumor.
Diagnostics
Early cases of hemifacial spasm are sometimes difficult to distinguish from facial myokymia, tics or myoclonus, which may be caused by pathological processes in the cerebral cortex or brainstem. In such cases, neurophysiological testing is the most valuable diagnostic method.
Wide and variable synkinesis on eyeblink tests and high-frequency discharges on electromyography (EMG) with associated clinical manifestations are diagnostic criteria for hemifacial spasm. Stimulation of one branch of the facial nerve can spread and cause a response in the muscle innervated by another branch. Synkinesia is absent in essential blepharospasm, dystonia or epilepsy. Needle myography shows irregular, short, high-frequency burst potentials (150-400 Hz) of motor units that correlate with clinically observed facial movements.
Visualization methods
Magnetic resonance imaging is the diagnostic method of choice when there is a need to exclude compression effects. Angiography of the cerebral vessels is generally of little value in the diagnosis of hemifacial spasm. Ecstatic blood vessels are rarely identified, and these vessel findings may be difficult to correlate with nerve effects. Performing angiography and/or magnetic resonance angiography is typically used to perform surgical vascular decompression.
Diagnostic methods
To determine an accurate diagnosis, doctors do not need much time; it is enough to check the patient by writing a few sentences on plain paper. During the course of action, typical symptoms of the anomaly can be identified:
- Incorrect placement of the hand and fingers.
- Tonic tension, tremors, constant loss of the pen and inhibition of the writing process due to painful sensations.
- Compensatory acts (to relieve discomfort, the patient often shakes his arm, pushes another limb, or massages the sore area).
The most popular diagnostic methods include:
- A detailed survey and obtaining a detailed medical history allows us to clarify the stages of development of the disorder, the likelihood of recurrence, and the presence of neurological abnormalities.
- Neurological examination - during a seizure, the tonic state of the muscle region is determined. Long-term damage to the hand is accompanied by a decrease in the level of muscle tone to 4 out of 5 points.
- Visiting a consultation with a psychiatrist.
- Electroneuromyography is prescribed, which will help detect tension/laxity regulation disorders in individual muscle groups of the dominant forearm.
- Writing test - helps to evaluate the duration and quality of the written text.
- Magnetic resonance imaging of the brain is prescribed to rule out cancer, encephalitis and other serious diseases.
How does writer's cramp manifest itself?
The main nuance of the disease is the step-by-step spread of disorders. The process begins with subclinical handwriting deformations, which are usually ignored by the patient. Later, difficulties appear in writing text, which arise when there is a need to quickly complete work, stress overload, or physical strain. As the anomaly progresses, persistent changes in some details in the handwriting are noticed, the patient writes noticeably more slowly, and the first problems begin to appear. A forced stop of business occurs with a sharp spasm, tremor, pain or weakness.
To prevent a negative situation, individuals adopt a certain position of their hands or fingers, shake or push with a healthy hand, and choose a comfortable writing object (a thick pen, brush). At the first stage of development of the disease, dyskinetic disorders manifest themselves in an isolated manner, that is, other types of motor activity (for example, playing a musical instrument, knitting, using a keyboard on a computer) remain normal.
At a late stage of the disease, the patient’s clinical symptoms become more pronounced, which causes a loss of the ability to control graphospasm through volitional efforts, and the compensatory techniques used do not work. Violations progress to motor everyday acts. Difficulties arise in spearing food with cutlery, typing text from a mobile phone, or even simply fastening buttons. Doctors say that the severity of the disease depends on posture (it is much easier for patients to write in an upright position) and external conditions. Constant overwork and stress provoke the rapid development of dysgraphia, while rest and calmness reduce its manifestation.
Treatment options
Therapeutic measures for a patient diagnosed with writer's cramp are quite difficult, as they require regular implementation, a long time and perseverance. Drug treatment does not have a quick effect and can cause various adverse reactions. Doctors prescribe pharmacological drugs only in a comprehensive course. The implementation of procedures is monitored by a neurologist, rehabilitation specialist and kinesiotherapist. Treatment plan:
- Medicines - combination formulations of medications, which are selected for each patient separately, have shown maximum effectiveness.
- Kinesiotherapy is a set of exercises for preserved movements. In some cases, the patient is recommended to learn to write with the other hand or use a computer.
- The use of an orthosis is a device for fixing the fingers and hand, which helps to increase the time of continuous writing.
- Written exercises are different techniques for improving activity.
- Botulinum toxin injections are a fairly promising treatment option. Difficult to perform, since it is problematic to find specific foci for administering the drug.