Causes
The disease is hereditary, linked to the X chromosome, so boys are almost always affected. Girls are carriers of a pathological gene (boys rarely survive to adulthood, and, moreover, are usually sterile). A change in the structure of the gene responsible for the synthesis of the dystrophin protein occurs on the chromosome.
Although the content of dystrophin in skeletal muscles is extremely small (thousandths of a percent), without it necrosis of muscle tissue quickly develops and progressive muscle dystrophy develops. If the gene is damaged in a site that completely destroys the synthesis of the dystrophin protein, Duchenne dystrophy develops. When insignificant parts of the protein are involved in the process, the disease takes the form of Becker's dystrophy.
Prevention and prognosis
Spouses with a history of hereditary diseases in their family should visit a geneticist before planning a pregnancy. Prevention of pathology also involves prenatal diagnosis. By identifying myopathy in the early stages, you can terminate the pregnancy.
Duchenne myopathy is a hereditary pathology characterized by severe course and rapid progression. This is a modern medical problem characterized by the destruction of muscle tissue and the rapid development of muscle weakness. All patients, without exception, die at an early age due to the development of complications incompatible with life. Only adequate and comprehensive therapy, strict adherence to doctor’s recommendations, careful care and parental care can slow down the progression of the disease.
Patients quickly become disabled and die at a very young age. The worst thing is that even qualified doctors, modern medical technologies and therapeutic techniques of the 21st century cannot help children with myopathy. The disease still remains incurable, taking young lives. Modern medical scientists around the world are working to create a radical way to combat Duchenne myopathy.
Symptoms
The onset of symptoms begins in early childhood, usually between 1 and 3 years. Initially, there is a delay in motor development, the child begins to walk late, often stumbles when walking, and gets tired quickly. Later, constant pathological muscle fatigue develops. The child practically cannot climb stairs. The gait begins to resemble a “duck” gait.
A characteristic symptom is the “ladder” symptom: an attempt to get up from a sitting position occurs using the hands, gradually, slowly, in several stages.
Gradually, muscle atrophy begins to be noted, first in the proximal parts of the lower, then upper extremities. Later, the muscles of the pelvic girdle, hips, back, and shoulder girdle atrophy. A “wasp” waist, curvature of the spine, and protruding shoulder blades (pterygoid blades) almost always develop.
Almost always there is a characteristic symptom of progressive Duchenne muscular dystrophy - pseudohypertrophy of the leg muscles. The muscles, although increased in volume, do not have sufficient strength and are very painful to the touch.
Three stages of the disease can be distinguished: - Stage I - weakness manifests itself only with significant physical activity (usually the first year of the disease). — Stage II – difficulty climbing stairs, weakness when walking quickly develops. — Stage III – represents paralysis, muscle contractures with the inability to move independently.
According to the type of course, it is divided into: Rapid progression. The ability to move is lost quickly, within the first 4-5 years from the onset of the disease. Average rate of progression: the patient cannot move after 10 years. Slow progression: there are no pronounced motor disorders 10 years after the onset of the disease. Typically, this option is characteristic of other types of muscular dystrophies than Duchenne dystrophy.
FACTS ABOUT DUCHENNE/BECKER MUSCULAR DYSTROPHY
WHAT IS DUCHENNE/BECKER MUSCULAR DYSTROPHY? Muscular dystrophies are genetic diseases characterized by progressive wasting and weakness of muscles, starting with microscopic changes in them. As muscles break down, their strength decreases.
In the early stages of DMD and BMD, the muscles of the chest (shoulder muscles), trunk, and upper and lower leg muscles are affected. Weakness in these muscles causes difficulty standing up, climbing stairs, and maintaining balance.
Duchenne muscular dystrophy (DMD) was first described in 1860 by French neurologist Guillaume Benjamin Amand Duchenne. Becker muscular dystrophy (BMD) is named after the German doctor Peter Emil Becker, who described this variant of DMD in 1950.
In DMD, signs of muscle weakness usually appear in boys around 3 years of age. The disease gradually weakens the skeletal or voluntary muscles of the arms, legs and torso. Around early adolescence or even earlier, the heart and respiratory muscles may also be affected.
BMD is a milder form of DMD. Its onset usually occurs in adolescence or early adulthood, and its progression is slower and much less predictable than DMD.
(Although DMD and BMD affect boys almost exclusively, in rare cases girls can also get these diseases. See “Does It Run in the Family?” )
WHAT CAUSES DUCHENNE AND BECKER MUSCULAR DYSTROPHY?
Before 1980, very little was known about the causes of any type of muscular dystrophy. In 1986, researchers identified a gene in which defects, called mutations, caused DMD. In 1987, the protein associated with this gene was identified and named dystrophin.
Genes contain codes, or recipes, for proteins (proteins), which are very important biological components of all life forms. DMD develops when a certain gene located on the X chromosome loses its ability to produce the protein dystrophin. DMD is caused by slightly different mutations in the same gene. People with BMD have some dystrophin, but it is either not enough or its quality is impaired. The presence of some dystrophin in BMD protects the muscles from degeneration as severe and rapid as in DMD.
Muscles are made up of bundles of fibers (cells). A group of independent proteins located along the membrane surrounding each fiber help muscle cells function normally.
When one of these proteins, dystrophin, is missing, it causes Duchenne muscular dystrophy, but if it is insufficient or defective, Becker muscular dystrophy develops.
By the way, eating or not eating protein-rich foods cannot replace lost dystrophin. For more information about how a gene mutation leads to the development of Duchenne and Becker dystrophies, see “Does It Run in the Family?”
WHAT HAPPENS TO THE MUSCLES OF PEOPLE WITH DUCHENNE AND BECKER DYSTROPHY?
Duchenne muscular dystrophy
The progression of DMD is quite predictable. Children with this condition often start walking late. During this period, parents may notice an increase in calf muscles, or hypertrophy. During preschool age, children with DMD may appear clumsy and fall frequently. Soon problems appear with climbing stairs, getting up from the floor or running.
By school age, children may begin to walk on their toes or the balls of their toes with a slightly rolling gait. Their gait becomes wobbling and unsteady, and they can easily trip and fall. Trying to maintain balance, they stick out their stomachs and throw their shoulders back. There are also difficulties raising your arms.
Almost all children with DMD lose the ability to walk between 7 and 12 years of age. During adolescence, activity of the arms, legs, and trunk requires assistance or mechanical devices.
Becker muscular dystrophy
Often, a diagnosis of Becker muscular dystrophy cannot be made until adolescence or even early adulthood, for example when young people notice that they are having difficulty with physical education or military training. Trying to compensate for muscle weakness, boys begin to walk with a waddling gait, on their toes or balls of their feet, with their stomachs sticking out.
As with DMD, muscle wasting in BMD usually begins in the hip and pelvic area, hips and shoulders. However, in BMD, the degree of muscle degeneration varies widely between individuals. Some require a wheelchair by age 30 or later, while others make do with minimal aids such as a cane for many years.
WHAT TESTS ARE USED TO DIAGNOSE DMD/BMD?
When diagnosing any form of muscular dystrophy, the doctor usually begins by getting to know the patient and family history and performing a physical examination. There is quite a lot to be gleaned from this, including the nature of the weakness. The history and examination begins the long road to an upcoming diagnosis before any more complex diagnostic tests are performed.
Because the leg muscles are weakened, boys with DMD use a characteristic technique for getting up from the floor called the Gowers maneuver. They start by resting on their hands and knees, then lifting their pelvis, and then “walking” their hands up their legs to lift their entire body.
It is important to get a correct diagnosis because other diseases have some of the same symptoms as DMD/D. BMD can often go undiagnosed or be misdiagnosed as end-girdle muscular dystrophy (CLMD) or spinal muscular atrophy (SMA). For this reason, it is important to perform both genetic testing and a muscle biopsy before deciding that it is BMD.
The doctor also wants to determine whether muscle weakness is caused by problems in the muscle itself or in the nerves that control those muscles. The muscle-controlling nerves, or motor neurons, that come from the spinal cord and brain and travel to all the muscles can cause muscle weakness similar to that caused by muscle problems, although they are actually different things.
Usually the nature of the weakness can be clarified during a physical examination. Sometimes a special test called an electromyography or nerve conduction study is done. This test measures the electrical activity of the muscles and stimulates the nerves to see whether the problem lies in the muscles or the nerves.
At an early stage of diagnosis, doctors often prescribe a blood test to determine CPK levels. CPK stands for creatine phosphokinase, an enzyme that leaks from damaged muscles. When CPK levels in the blood are elevated, it usually means that muscles are being broken down by some pathological process such as muscular dystrophy or inflammation. Therefore, a high level of CPK suggests that muscle weakness is caused by pathological processes in the muscles themselves, but cannot indicate exactly what kind of muscle disease it may be.
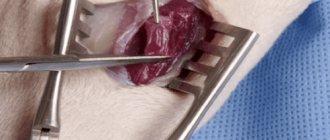
To determine which disease is causing the problems, the doctor may order a muscle biopsy, the surgical removal of a small piece of muscle from the patient. By examining this sample, the doctor can tell a lot about what is really going on with the muscles. Modern techniques allow, on the basis of a biopsy, to distinguish muscular dystrophies from inflammatory and other diseases, as well as to distinguish between various forms of dystrophies
Other tests using biopsies can provide information about what protein is present in muscle cells, and whether it is present in normal amounts and in the right place. This can help differentiate between DMD (no dystrophin) and BMD (some defective dystrophin). MRI (magnetic resonance) may also be prescribed. This painless scan allows the doctor to visually determine what is happening inside the weakened muscle.
The availability of DNA diagnostic tests, which use either blood cells or muscle cells to obtain precise genetic information, is rapidly evolving. You can ask your doctor or genetic counselor what tests are available. Because many men with BMD (and some with DMD) become fathers, it is important to know exactly what kind of inherited disease a person has. Sisters of people with DMD or BMD may also be tested to find out if they are carriers of the disease, as they may then have children with the condition.
IS THIS FAMILY?
Upon learning that a child has a genetic disease such as DMD or BMD, confused parents often ask: “But it didn’t happen in our family, how could it be genetic?”
DMD can run in a family, even if only one family member has it. This is due to the mechanism of inheritance of genetic diseases.
Both DMD and BMD are inherited in a so-called X-linked pattern. This means that the gene, the mutation in which causes the disease, is located on the X chromosome
Every male child receives an X chromosome from his mother, and a Y chromosome from his father, which makes him a boy. Female children receive two X chromosomes, one from each parent.
Each son born to a woman with a mutation in the dystrophin gene on one of her two X chromosomes has a 50% chance of inheriting the damaged gene and having DMD or BMD. Each daughter of such a woman has a 50% chance of inheriting the mutation and becoming a carrier. Carriers usually have no symptoms of the disease, but they may have children with the mutation or disease.
So how does a family with no history of DMD or BMD suddenly have a son with this disease?
There can be two explanations for this:
The genetic mutation that causes DMD or BMD can be present in women for generations without anyone knowing about it. There may not have been any boys born with the disease, or even if a boy in earlier generations had the disease, the relatives may not have known what the disease was.
Another explanation is that a child with DMD or BMD has a new genetic mutation that occurred during his or her fetal development. Once someone develops a genetic disease, even if the mutation is spontaneous (new) in that person, they can pass it on to their offspring.
Men with DMD or BMD cannot pass the damaged gene to their sons because they pass on a Y chromosome, not an X. But they can certainly pass it on to their daughters, since each daughter only receives an X chromosome from her father. They will be carriers, and each of their sons will have a 50% chance of having the disease, and so on.
A good way to learn more about your family's inheritance pattern is to talk to your doctor or genetic counselor. You can also view the brochure.
WOMEN AND DMD
Why don't girls get DMD or BMD? When a girl inherits the damaged gene from her mother, she usually also receives a “healthy” dystrophin gene from her father, which produces enough of the protein to prevent the disease from developing. Boys who inherit the mutant gene get sick because they lack the second dystrophin gene, which compensates for the damage to the first.
However, although girls usually do not have the full extent of DMD or BMD, some women who carry the damaged gene are still affected to some extent. A small percentage of women who carry the mutation are so-called “expressed carriers,” and the disease manifests itself in them in a mild form.
In such women, dystrophin deficiency can manifest as weakness in the muscles of the back, arms and legs and their rapid fatigue. Severe carriers also have heart problems, which may include shortness of breath or an inability to perform simple exercises. Heart problems, if left untreated, can be quite serious and even life-threatening.
It would be prudent for all women who are potential carriers of DMD/BMD to undergo a full diagnostic examination to determine their status. Subsequently, if carrier status is confirmed, regular strength assessment and cardiac monitoring may help manage symptoms that tend to worsen.
WHAT CAN BE DONE TO TREAT DMD/BMD?
Thanks to advances in many areas of medicine, there are very good therapeutic methods that can help with all manifestations of Duchenne and Becker muscular dystrophies. These methods of influence are constantly being improved. Using all available methods, patients can prolong their vigor, activity and life expectancy.
Contractures
The impact of the disease can be greatly minimized by keeping the body as flexible, straight and mobile as possible. There are several ways to achieve this.
As muscles break down, patients with muscular dystrophy often develop joint stiffness called contractures. If left untreated, they will become quite severe, causing discomfort and limiting mobility and flexibility. Contractures can affect the knees, hips, feet, elbows, wrists and fingers.
However, there are many ways to minimize and delay contractures. Range of motion exercises performed regularly help slow contractures by preventing tendons from shortening prematurely. It is important to have a physical therapist show you how to perform these exercises correctly.
Splints on the arms and legs can also help keep the limbs stretched and mobile, delaying the onset of contractures.
Once contractures form, surgery can help relieve them. A tendon lengthening procedure called Achilles tendon surgery is often performed to treat contractures in the ankle while the child is still able to walk. The child usually requires the use of splints on his legs after this.
Spinal curvature
In adolescents with DMD, the spine may gradually take on a curved shape. This curvature can occur from side to side (scoliosis), or in the longitudinal direction, taking on the shape of a hump (kyphosis). Sometimes those who still walk have a concave curvature in the lumbar spine, called lordosis.
Severe scoliosis can interfere with sitting, sleeping and even breathing, so it is advisable to prevent it.
You can consult a physiotherapist about what exercises are necessary to keep your back as straight as possible, as well as the correct positions while sitting and sleeping.
The surgical method of correcting the curvature involves inserting metal rods into the spine. Typically, such operations are performed at the age of 11-13 years.
Medicines
Medications are a group of drugs known as corticosteroids that have been shown to be effective in slowing the progression of DMD (there is limited evidence for or against corticosteroids in DMD)
In 2005, the American Academy of Neurology published guidelines for the use of these drugs in DMD. They are as follows:
•Prednisolone or deflazacort are effective in the treatment of DMD. Seven-year studies have shown that their use increases strength and improves muscle timing (such as time spent climbing stairs) and lung function
•Effective starting doses: 0.75 mg per kg body weight daily for prednisolone, and 0.9 mg per kg body weight daily for deflazacort
•The dose should be reduced in the presence of serious side effects such as significant weight gain, thinning of bones (osteoporosis), and behavioral problems. The most common side effects are weight gain and the formation of a round, puffy face.
•It is not yet clear that the use of deflazacort has fewer side effects than prednisolone
The optimal age for starting corticosteroid therapy has not been determined. Some doctors believe that it should be started immediately after diagnosis, while others prefer to wait until the boys first have problems with walking. Before starting corticosteroid therapy, the physician should discuss the expected benefits and potential side effects with the parents.
Calcium supplements and vitamin D are often prescribed in combination with prednisolone to counteract its unwanted effects on bones
A low-calorie, low-sodium diet is usually recommended to manage body weight and fluid retention observed with corticosteroids.
Sometimes, for DMD or BMD, medications are prescribed to reduce the workload on the heart (see "How else do DMD and BMD affect the body?" )
Retainers, verticalizers and wheelchairs
Braces, also called orthoses, support the lower leg and foot, or wrap around the knee. Ankle orthoses are sometimes prescribed for use at night to help prevent a child's foot from dropping during sleep.
Standing for periods of time during the day, even with minimal weight bearing, promotes better circulation, stronger bones and straighter spine. Walkers or standing chairs can help people with DMD and BMD with this. Some wheelchairs also have an upright position
Sooner or later, all boys with DMD require a wheelchair. Many people first use wheelchairs at school or for a walk, and continue to walk at home. With DMD, the need for constant use of a stroller usually occurs around the age of 12 years. Although many children and their parents perceive wheelchairs as a symbol of disability, most believe that using them allows them to be more mobile, active and independent than trying to walk at all costs on very weak legs.
Other devices may help those caring for people with DMD or BMD. Among the simplest are transfer platforms to help transfer from or to a wheelchair. You can also use mechanical (usually hydraulic) lifts, folding chairs and electronically controlled beds.
HOW OTHER DO DMD AND BMD AFFECT THE BODY?
Pain and sensitivity
You can rest easy knowing that muscle wasting in DMD and BMD is usually painless in itself. Some people report intermittent muscle spasms, which are usually relieved with over-the-counter pain relievers
Also, because muscular dystrophy does not directly affect the nerves, people with this disease retain normal touch and other senses. They also typically control the smooth, or involuntary, muscles of the bladder and bowel, and maintain normal sexual function.
Heart
Similar to the muscles of the limbs, the heart muscle can also be weakened due to a lack of dystrophin. Over time, sometimes even before the age of 10 years, cardiac problems associated with DMD can become life-threatening. Thus, careful monitoring of the cardiovascular system is necessary, usually performed by a pediatric cardiologist.
Due to dystrophin deficiency, people with DMD and BMD often develop cardiomyopathy, a weakness of the heart muscle. The muscle layer of the heart (myocardium) degenerates in the same way as skeletal muscle, which can lead to fatal cardiac problems
Some people with BMD have less severe skeletal muscle damage but still have serious cardiac problems
In 2005, the American Academy of Pediatrics formulated recommendations for people with DMD and BMD, as well as carriers of these diseases.
It is recommended that patients with DMD undergo a complete cardiac examination in early childhood, and then every 2 years until the age of 10 years. Thereafter, the examination should be carried out every year, or when symptoms of heart weakness, such as fluid retention and shortness of breath, appear.
For patients with BMD, screening is recommended at least every two years, starting at age 10 years.
Carriers of DMD and BMD have a higher than average risk of developing cardiomyopathy. Experts believe that carriers should undergo a complete cardiac examination in late adolescence or early adulthood, or rather - when symptoms appear, and thereafter - such examinations every 5 years, starting at 25-30 years of age
There is preliminary evidence that treatment with angiotensin-converting enzymes (ACEs) and beta blockers may slow heart muscle damage in DMD and BMD if treatment is started as soon as abnormal echocardiograms (ultrasounds of the heart) are detected, without waiting for symptoms to appear.
Some patients with BMD with serious cardiac problems but in good general condition have been successfully treated with heart transplantation.
Respiratory function
When boys with DMD reach about 10 years of age, the diaphragm and other muscles that control the lungs weaken, and the lungs are less efficient at their function. Problems that indicate insufficient respiratory function include headaches, decreased mental activity, difficulty concentrating or staying alert, and nightmares.
People with weakened respiratory systems are also more susceptible to infections and have difficulty coughing. Simple hypothermia can lead to the development of pneumonia. If an infection develops, it is important to get immediate medical attention to prevent severe respiratory failure.
When respiratory function weakens, families can purchase a ventilator or learn procedures to help clear the throat and keep the bronchi clear of secretions. You can get the necessary information from a therapist or pulmonologist
In some cases, forced ventilation may be required to ensure sufficient air movement into and out of the lungs. Sometimes a breathing mask is only required at night. If this is needed more often, a tracheotomy may be performed (a tube is inserted directly into the trachea to provide air into the lungs)
There are effective non-invasive ventilation systems that eliminate the need for tubes. Even for those who have tubes in their trachea, it is sometimes possible to remove them from the machine for periods of time during the day. More modern tubes have valves in their design that allow speech.
Intellectual abilities
About a third of boys with DMD have some degree of cognitive delay, some quite severely. Experts believe that a deficiency of dystrophin in the brain can cause cognitive and behavioral abnormalities. The learning difficulties seen in some people with DMD and BMD occur in three main areas: focusing, verbal learning and memory, and emotional interaction.
If there is a suspicion that the child has some delay in mental development, it is necessary to contact a pediatric neuropsychologist. If this is confirmed, educational and psychological intervention should be initiated immediately. The specialist can recommend exercises and other ways to interact with the child that will help him make up for this deficiency.
CAN SPECIAL DIETS OR EXERCISES HELP WITH DMD AND BMD?
Diet
Many people, when they hear the words “protein loss,” logically ask the question: “Do I need to consume more protein?” Unfortunately, consuming foods high in protein has no effect on the proteins missing in muscular dystrophy
There are no special dietary restrictions or supplements known to help with DMD or BMD. The combination of inactivity and weak abdominal muscles can cause severe constipation, so the diet should be high in fluids and fiber, with plenty of fresh fruits and vegetables.
Boys who use power wheelchairs, are taking prednisone, and are not very active may need to restrict calories to maintain weight. Obesity puts additional stress on already weakened muscles and the heart. Experts believe that a low-calorie diet does not have any harmful effects on muscles.
Those taking prednisone and those with heart problems may also need a low-sodium diet.
Exercises
Exercise can help build muscle, maintain a healthy cardiovascular system and promote overall well-being. However, with muscular dystrophy, excessive exercise can damage the muscles. Talk to your doctor about the best exercise routine. With DMD and BMD, moderate physical activity is possible, but not to the point of exhaustion.
Some experts recommend swimming and exercise in water (aquatherapy) as a good way to keep your muscles as toned as possible without overstraining them.
The supportive properties of water can help prevent some types of muscle strain and damage. Before starting any exercise program, you should have a cardiac evaluation.
Physical and occupational therapy
Physiotherapy is usually part of comprehensive therapy for DMD and BMD. A physical therapist should be consulted to assess your physical condition and develop a physical therapy program. The main goals of physiotherapy are to maintain joint mobility, prevent contractures and scoliosis.
Occupational therapy is more focused on specific activities and functions, as opposed to physical therapy, which focuses on mobility and, where possible, strengthening large muscle groups.
Occupational therapy can help with tasks related to work, leisure, and daily living, such as getting around, getting dressed, or using a computer.
HOW TO LIVE WITH THIS?
When one family member has DMD or BMD, the entire family experiences support needs and emotional reactions. Many people find help and support from religious sources, conversations with families with similar experiences, books on psychology, or consultations with specialists. Such specialists usually recommend the following:
For children
•Answer children's questions about illness as they grow older in honest and accessible language
•Always present the child as an individual, with the illness as only one aspect of his life
•Focus on what the child can do and help him do what he wants. Children often find ways to engage in sports or other hobbies
•Raise him as you would any other child, with patience, responsibility, hope and love. Avoid being overprotective and help him become independent.
•Participate in normal family activities, including vacations and entertainment. With imagination and patience, you can find ways to do almost anything
For family
•Be attentive to each other’s emotions and stress levels, be patient and kind
•Plan regular breaks from caring responsibilities
•Tackle illness-related problems as they arise. Don't Focus on Future Complications
•Give yourself credit for the effort expended and the difficulty of your responsibilities
•Organize a support team and ask for help when needed
Research to find treatments for DMD
Since 1986, when the gene whose mutations cause DMD and BMD was identified, scientists have made great progress in understanding the mechanisms of these diseases. Currently, several directions are being developed to find ways to stop or reverse muscle destruction in these diseases
Some researchers have created a working dystrophin gene without mutations, and are currently testing its safety in a small clinical trial involving boys with DMD.
Other researchers are testing PTC124, a drug that changes the way cells “read” genetic information. In approximately 15% of patients with DMD, the molecular stop signal is located too early for full-fledged dystrophin to be synthesized. PTC124 causes cells to ignore this signal
Still other researchers are experimenting with antisense nucleotides, compounds designed to encourage cells to bypass certain types of genetic errors, not just stop signals. These formulations have been laboratory tested and early clinical trials have shown promising results.
Other groups of researchers are using stem cells isolated from muscles, blood vessels or bone marrow in attempts to achieve muscle regeneration.
Finally, several groups are developing strategies to enhance the synthesis of the protein utrophin, which is very similar to dystrophin but is synthesized in people with DMD and BMD. Experiments show that increasing utrophin levels can compensate for dystrophin deficiency to some extent
You can read a summary of the main studies
Based on materials
Diagnostics
The clinical picture is very bright. Often the disease is diagnosed after clarifying a genetic history (presence of cases in the family) and a neurological examination. In the neurological status, the disappearance of knee reflexes is noted, a little later reflexes from the biceps and triceps disappear. Achilles reflexes are preserved for a long time.
Externally, deformation of the joints of the foot may be revealed, there are signs of cardiomyopathy: irregular pulse, dullness of heart sounds, dilation of the heart cavities according to EchoCG, changes in the electrocardiogram.
An important factor is the increase in the biochemical parameters of creatine phosphokinase (an enzyme indicator of muscle breakdown). The activity of this enzyme increases tens of times. There is a direct correlation between the degree of increase in enzyme activity and the severity of manifestations of Duchenne dystrophy. [!] In difficult diagnostic situations, a cytological examination is performed.
Complications
Duchenne muscular dystrophy shortens a person's life span. This is the main and most terrible consequence of the disease.
Complications from the musculoskeletal system:
- Osteoporosis is a decrease in bone density,
- Pathology of the joints - decreased mobility due to severe muscle weakness,
- Scoliosis, kyphosis, lordosis are various forms of spinal curvature.
Damage to the digestive organs:
- Constipation is the result of physical inactivity,
- Weight loss due to muscle breakdown,
- Violation of the process of chewing and swallowing requires feeding the patient through a tube.
Respiratory disorders:
- Shallow breathing
- Weak cough reflex
- Frequent ARVI,
- Lack of oxygen in the blood - headaches in the morning, awakenings at night, weakness, irritability, intense dreams.
People with Duchenne myopathy develop cardiomyopathy - myocardial weakness, manifested by increased fatigue, shortness of breath, swelling of the legs, and interruptions in heart function.
Timely diagnosis and effective therapy can delay the development of complications or completely prevent their occurrence.
Treatment and life prognosis
Treatment is symptomatic. Hormonal drugs are used to stop the destruction of muscle fiber, phospholipids to protect muscle cells from destruction, and elements of therapeutic exercises. Various orthopedic devices are being introduced into practice to facilitate movement. Massage is strictly contraindicated in most cases, as it can lead to accelerated muscle breakdown. Treatment of hereditary diseases is a matter of the future.
The life prognosis for patients is unfavorable. The course of the disease is progressive. Death is inevitable. As a rule, by the age of seven, severe symptoms develop, leading to complete immobility by the age of 13-14. Patients rarely live to 18-20 years of age.
Treatment process
Duchenne disease, like any other hereditary pathology, is incurable. Doctors provide symptomatic therapy that eliminates unpleasant symptoms, prevents the development of complications and prolongs the life of patients.
Comprehensive supportive treatment of the disease:
- Drug therapy slows but does not stop the progression of myopathy. Patients are prescribed glucocorticosteroid drugs “Prednisolone”, “Betamethasone”, cardiac drugs “Ri”, “Perindopril”, metabolic drugs “Mildronate”, “Riboxin”, “Cinnarizine”, multivitamins “Neuromultivit”, “Doppelherz”.
- Physiotherapy consists of passive stretching of the affected muscles, exercise therapy, massage, electrophoresis, hydrotherapy, inductothermy, laser therapy, and ultraphonophoresis.
- Diet therapy – complete nutrition with sufficient amounts of vegetable fats and animal proteins. Patients are advised to exclude strong tea and coffee, alcohol, spices, baked goods, chocolate, and fast food from their diet. Vegetable and fruit dishes, lactic acid products, cereal products, and eggs are healthy.
- To maintain the functioning of the respiratory system at an optimal level, patients need artificial ventilation, which saturates the blood with oxygen. To do this, various portable devices are used at home, and in the hospital, seriously ill patients have their trachea intubated or have a tracheostomy.
- Orthopedic care is necessary for all patients with Duchenne myopathy. Moreover, the older the child becomes, the more pronounced the signs of pathology are, which means the need for orthopedic devices is much greater. Standing machines, wheelchairs, special splints and corsets make life much easier for sick people.
- In some cases, patients require psychotherapeutic support. This is associated with the development of depression and suicidal tendencies in children. Not every teenage child can come to terms with his helplessness and life in a wheelchair.
- The use of stem cells and gene therapy are emerging trends in the treatment of hereditary diseases. By introducing healthy genes into the body or replacing ordinary cells with stem cells, it is possible to improve the functioning of the body at the cellular level and normalize the patient’s condition. Stem cells are used to restore damaged muscle fibers. Patients are given myogenic cells that produce normal dystrophin in sufficient quantities. Any scientific development, proven experimentally, gives patients hope for recovery.
Etiology
Until the end, the etiology of Duchenne-Aran disease is unknown. The hypothesis about the ethnological significance of vitamin E deficiency has not been proven. Hereditary and family cases occur only as rare casuistry. Nevertheless, some kind of congenital predisposition in the form of insufficient resistance of the cells of the anterior horns is easy to assume, since many patients exhibit features of a neuropathic constitution. Among the exogenous factors that may play a role in the development of the disease, injury to the central nervous system, various acute general infections, chronic infections, and intoxications are indicated. The question is also raised about the possible role of a specific virus in this disease. The vast majority of researchers consider chronic “poliomyelitis” of adults, which underlies Duchenne-Aran disease, as a purely degenerative, rather than infectious-inflammatory process. It must be especially emphasized that it has nothing to do with acute polio (Heine-Medin disease). Nevertheless, the significance of infection in this disease cannot be completely denied.
Skeletal muscle damage
Children are born without serious health problems. However, after just a few months, their motor development begins to lag. These kids are less active. Doctors and parents do not yet notice obvious deviations, attributing everything to temperamental characteristics.
The initial symptoms of the disease appear after the first steps. Children with Duchenne dystrophy constantly fall and walk on their toes. While most of their peers are already confidently standing on their feet, they stubbornly continue to experience difficulty moving.
The next stage in the manifestation of the disease is the period when babies acquire the ability to speak. They begin to complain to their parents about weakness and fatigue. Jumping on the playground, running, climbing horizontal bars - all these types of activities do not bring them pleasure.
What other symptoms does Duchenne muscular dystrophy have? Govers' disorder is considered a unique manifestation of the disease. Every time the child tries to get up from the floor, he uses his hands to help the weak leg muscles. To this end, he leans his limbs on himself, moving them all over his body.
The gradual progression of the disease leads to the fact that sick children by the age of 10-12 lose the ability to move independently. Most of them need a wheelchair. The ability to hold the body in an upright position lasts only until the age of 16.
Treatment
There is no effective treatment for Duchenne-Aran disease yet. Several courses of disinfectant therapy are carried out. If there is reason to suspect a history of lyuesa, antisyphilitic treatment is required. In all cases, massage, non-tiring physical therapy, iodine galvanization of the spine, and diathermy of the affected limbs are indicated. Vitamins B1, B12, E. Injections of ATP (monocalcium salt of adenosine triphosphoric acid); glutamic acid, blood transfusions. Prozerin, dibazol, galantamine.
Pathological anatomy
Anterior and posterior horns of the spinal cord
The pathological picture of the spinal cord in Duchenne-Aran disease is a slowly progressive atrophy of the cells of the anterior horns, especially those that give rise to the fibers of the anterior roots. Over time, these cells die, their decay products are removed from the central nervous system, and the place of ganglion cells is taken by neuroglia. The fibers of the anterior roots and their continuations in the peripheral nerves undergo degeneration and are replaced by connective tissue. The muscle fibers associated with the affected segments of the spinal cord also atrophy. On histological sections, the affected muscle fibers lie in small groups (which is typical for neurogenic amyotrophies). There is no inflammatory vascular-connective tissue reaction. Often in the spinal cord with Duchenne-Aran disease, thickening of the walls of blood vessels and narrowing of their lumen are observed.
Main reasons
Muscular dystrophy is a consequence of abnormalities in the genetic code of DNA. The mutation occurs in a gene located on the X chromosome. One of its sections is responsible for the production of a special protein - dystrophin. This substance at the microscopic level forms the basis of muscle fibers and performs several functions:
- maintenance of the cell skeleton;
- ensuring the ability of muscle fibers to contract and relax.
In this disease, dystrophin is absent or poorly synthesized. The level of “normal” protein does not exceed 3%. This mutation leads to the destruction of fibers in the muscles. They gradually degenerate and are replaced by fatty and connective tissue. As a result, the person loses the ability to move.
What type of inheritance does Duchenne muscular dystrophy have? The disease is transmitted according to a recessive trait. In the human body, all genes are paired. In order for pathological disorders to appear with a hereditary disease, the genetic defect must occur in one chromosome or in similar areas of both. In the second case, we are talking about a recessive type of inheritance.
If a genetic defect is diagnosed in only one chromosome, but the disease progresses, they speak of a dominant transmission trait. The recessive type is possible with simultaneous damage to identical DNA structures. When the second chromosome is absolutely “healthy”, pathology does not develop. Therefore, dystrophy is diagnosed only in males. They have one X chromosome in their genetic set, and the second (Y) is a pair.
What does science say about the fair sex? Duchenne muscular dystrophy is rarely diagnosed in girls. To do this, two pathological X chromosomes must match in the genotype, which is unlikely. Girls can only act as carriers of the disease and pass it on to their sons.