What is meningitis and why is it dangerous?
Meningitis is a disease that consists of inflammatory damage to the membranes of the brain and spinal cord. According to the ICD-10 classification, it has codes G0-G3. Pathology can occur as a complication of another disease or as an independent process.
The main routes of transmission for meningitis are airborne, vertical and blood contact. The source of infection in the disease are patients with severe forms of the disease, persons with nasopharyngitis and healthy carriers.
Doctors classify meningitis as a contagious disease. The most contagious forms of the disease include processes caused by meningococcus. Severe patients are dangerous to others in the first days of the development of pathology. Patients with meningococcal infection in the form of nasopharyngitis pose a danger to the environment for several weeks.
The release of meningococci into the environment by healthy carriers during sneezing and coughing occurs within 2-3 weeks. In some cases this period is more than 2 months. The greatest susceptibility to infectious agents is observed in children and patients with a weakened immune system.
Classification of meningeal signs
There are meningeal, cerebral, and general infectious signs, which always accompany pathologies associated with damage to the meningeal tissues of the brain. In the second case we observe:
- Pain in the head area, which often spreads diffusely, is bursting, tense, and painful.
- Nausea, which is usually accompanied by bouts of vomiting. Vomiting can occur spontaneously without a previous feeling of nausea and does not bring relief.
- Confusion, mental and motor agitation, hallucinations. In severe cases of pathology, coma and stupor occur.
- Convulsions of varying intensity and volume - from twitching of single muscles to generalized (distributed throughout the body) convulsive status.
Similar manifestations are characteristic of many CNS pathologies. They arise as a result of swelling of the brain structures, irritation of the meningeal parts of the brain, and disturbances in liquorodynamics. Pain in the head area is a typical meningeal symptom that appears at the onset of the disease and is observed throughout the entire period of its course, until recovery.
In newborns, cephalgic syndrome is often manifested by a characteristic hydrocephalic cry - piercing, sudden, sharp sounds that the baby makes even in an unconscious state, during sleep. Cephalgic syndrome is associated with irritation of nerve endings arising from the trigeminal and vagus nerves, as well as innervating the meninges and blood vessels located in the brain. Vomiting in infants is predominantly gushing in nature. General infectious signs include:
- Malaise, poor health.
- Increased irritability.
- Increased body temperature.
- Heart rhythm disturbances (bradycardia, tachycardia, arrhythmia).
- Hyperemia (redness, flushing) of the skin of the face.
- Rapid breathing.
The variability of individual manifestations should be taken into account. For example, the body temperature with purulent meningitis often exceeds 40°C; with the serous or tuberculous form of meningitis, the temperature is much lower; with the syphilitic form, the temperature remains normal. Direct meningeal symptoms include:
- Hyperesthesia – increased sensitivity to external stimuli.
- Muscle tension of the tonic type, including rigidity (inflexibility, hardness) of the neck muscles, reflexes described by Brudzinsky, Kernig, Lessage (in children).
- Typical reactions in the form of painful sensations when pressing on the area on the face where the trigeminal nerves exit, or on the eyeballs, are pathological reflexes described by Bekhterev, Mendel, Pulatov.
- Changes in neurological reflexes - periosteal (periosteal), tendon, abdominal. Characteristic is the revival of reflexes followed by an uneven decrease in reaction.
A full set of typical symptoms is observed in 7% of patients diagnosed with meningitis initiated by meningococci. In other cases, the manifestations are variable, many meningeal signs may be negative - not appear at all. The severity of manifestations depends on the age of the patient, the type and characteristics of the course of the disease.
Causes of meningitis
The main etiological factor in the development of the disease in adults is damage to the membranes of the brain by infectious agents. These include:
- Bacteria - meningococci, staphylococci, streptococci, tuberculosis and E. coli.
- Viruses are the causative agents of epidemic and herpetic mumps.
- Fungi - candida and mycoses.
Among the factors contributing to the activation of pathogenic microorganisms, the most common are:
- decreased immune defense due to chronic diseases or long-term use of chemical medications;
- regular overwork;
- unbalanced diet;
- metabolic disorders;
- insulin-dependent type of diabetes mellitus;
- diseases of the gastrointestinal tract;
- HIV infection;
- mosquito and tick bites.
In addition, the development of meningitis can be caused by complications of traumatic brain injury, pneumonia, sinusitis or purulent otitis.
Classification
Depending on the origin, the disease is divided into:
- Primary – occurs as an independent disease. The infection enters the oral and nasal cavities, from where it infects the meninges through the sinuses. Their direct infection is possible with open head injuries or during brain surgery with insufficient sterilization of instruments.
- Secondary - acts as a complication of an existing inflammatory process.
According to the localization of inflammation, they are distinguished:
- Basal meningitis – inflammation affects the base of the brain. The disease is characterized by meningeal and cranial nerve symptoms.
- Convexital - inflammation is based in the cerebral cortex. Characterized by psychomotor agitation.
- Total - affects the entire soft membrane of the brain.
- Spinal - affects only the soft membrane of the spinal cord.
According to the type of flow, they are distinguished:
- Fulminant – characterized by rapid development and swelling of the brain.
- Acute is the most common type. Combines cerebral and meningeal symptoms.
- Abortive – difficult to diagnose, symptoms of intoxication predominate.
- Recurrent – occurs in the presence of a chronic focus of infection.
The first signs of meningitis in an adult
The clinical picture of the pathology depends on the cause of its development. At the initial stages, patients experience nonspecific or subtle symptoms. The first signs of meningitis in adults are the development of meningeal syndrome, which includes:
- diffuse pain syndrome, aggravated by external factors;
- vomiting without nausea, which does not alleviate the patient’s condition;
- general weakness;
- fast fatiguability;
- increased excitability;
- irritability.
These symptoms may be confused with signs of arterial hypertension, mental stress and other pathologies. For this reason, the diagnosis can be confirmed only after the development of pathogenic processes. Common symptoms of meningitis in adults include:
- increased tone of the cervical and occipital muscles;
- hyperesthesia to light, sounds, touches;
- pain with pressure on the eyelids and eye movement;
- loss of appetite;
- rise in body temperature;
- pain in muscles and joints;
- clouding of consciousness.
Symptoms
Clinical manifestations of tuberculous meningoencephalitis in adults and children can be divided into three periods:
- Prodromal, or period of precursors, lasting from 3-5 to 21-26 days.
- The period of clinical manifestations of irritation of the meninges and cranial nerves.
- The period of clinical manifestations of brain tissue damage.
Difficulties in diagnosis at the onset of the disease are due to the fact that meningoencephalitis can develop against the background of an acute respiratory disease, influenza, etc.
In the prodromal period, symptoms of intoxication come to the fore:
- general weakness,
- headache,
- malaise,
- increased fatigue,
- lethargy,
- decreased performance,
- sweating,
- loss of appetite,
- sleep disturbance,
- irritability,
- periodically low-grade fever,
- vague lethargy
- apathy.
The prodromal period is modified by pronounced clinical manifestations of irritation of the meninges and cranial nerves. There are 4 syndromes characteristic of this period:
- general infectious,
- meningeal,
- symptoms of damage to cranial nerves and spinal roots,
- changes in cerebrospinal fluid.
1. General infectious syndrome - there is a constantly elevated temperature from subfebrile to hectic, preceding headache or occurring along with it.
2. Meningeal syndrome - tuberculous meningitis is characterized by its gradual development, but an acute onset also occurs. Meningeal syndrome includes :
- headache,
- nausea,
- vomit,
- hyperesthesia,
- characteristic meningeal posture,
- stiff neck,
- Kernig's, Brudzinski's symptoms, zygomatic Bekhterev's symptom, etc.
Headache - can be diffuse or localized (mainly in the forehead and back of the head). Its occurrence is associated with irritation of the sensory endings of the III pair of cranial nerves, as well as parasympathetic (X pair) and sympathetic fibers that innervate the meninges.
Vomiting accompanies headache, has a “fountain-like” character, does not bring relief, and does not depend on food intake. It is central in nature, caused by irritation of the receptors of the vagus nerve or its nuclei (located at the bottom of the IV ventricle) or the vomiting center in the medulla oblongata. General hyperesthesia and increased sensitivity are caused by irritation of the dorsal roots.
chicken” position is typical - the patient lies with his head thrown back, the torso is extended, the stomach is retracted (scaphoid), the legs are bent at the knees and pulled towards the stomach. This position is a consequence of tonic muscle contraction. A thrown back head is caused by stiff neck (increased tone of the neck extensor muscles).
The main clinical symptoms of tonic muscle tension are:
• A symptom of neck rigidity is tension in the muscles of the back of the head, sharp whiteness when trying to tilt the patient’s head forward and get the chin to the chest.
• Kernig's sign is the inability to straighten the leg at the knee joint, which was previously bent (at a right angle) at the knee and hip joints.
• Brudzinski's symptoms (there are four):
- First (upper) - when trying to bring the head to the chest, the lower limbs involuntarily bend at the knee joint
- Second (zygomatic) - upon percussion of the zygomatic arch the same reaction is observed;
- Third (middle or pubic) - pressing in the area of the pubic joint causes involuntary bending of the legs at the knee joints;
- Fourth (lower) - when trying to straighten one leg at the knee joint (study of Kernig's symptom), the other leg reflexively bends at the knee joint and is pulled towards the stomach.
• Bekhterev's symptom - with percussion of the zygomatic arch, the headache intensifies and a grimace of pain involuntarily appears on the corresponding side of the face.
3. Symptoms of damage to cranial nerves and spinal roots. The III, VI, VII, IX, X, XII pairs of cranial nerves are most often affected due to compression by exudate, as well as direct damage by the inflammatory process. When the third pair is affected, ptosis, mydriasis (pupil dilation), strabismus, and diplopia occur; VI pairs - convergent strabismus, diplopia; VII pairs - facial asymmetry due to peripheral paralysis of facial muscles (wrinkles on the forehead and face are smoothed out, the palpebral fissure becomes wider, the corner of the mouth is lowered); XII pairs - strabismus, paresis or paralysis of the corresponding half of the tongue, its atrophy. When you try to stick out your tongue, it deviates in the direction of the lesion.
Chorioretinitis also occurs, as well as lesions of the fundus: swelling of the optic nerve papillae, optic neuritis.
Chorioretinitis is an inflammation of the posterior part of the choroid and retina. Nodules appear on them - lymphoid infiltration with giant epithelioid cells or tuberculous granulomas with caseation. When chorioretinal changes are localized at the edge of the optic nerve head, neuroretinitis develops.
4. Changes in the cerebrospinal fluid - the cerebrospinal fluid is clear or opalescent, colorless, its pressure is increased. In patients with tuberculous meningitis, during puncture, cerebrospinal fluid flows out under pressure, often in drops or a stream (normally 20-40 drops per minute). It is forbidden to release CSF jets, because instant death of the patient may occur due to herniation of the medulla oblongata into the foramen magnum (herniation occurs as a result of a sharp decrease in pressure in the subarachnoid space of the spinal cord while maintaining increased fluid pressure in the subarachnoid space of the brain).
Tuberculous meningitis is characterized by the following changes in the cerebrospinal fluid :
- increase in protein content - 1-2 g / l or more, therefore the Pandi and Nonne-Appel reactions are positive;
- pleocytosis - an increase in the number of cells in the cerebrospinal fluid (on average 100-300 per mm3), lymphocytes (T-lymphocytes) predominate; Normally, 1 mm3 contains 10 leukocytes;
- for tuberculous meningitis there is a typical protein-cell dissociation, which occurs due to the predominance of stagnation over inflammatory phenomena. It is characterized by a high protein content in the cerebrospinal fluid and relatively little cytosis and indicates a significant disruption of the circulation of the cerebrospinal fluid. Less commonly, cell-protein dissociation occurs, which is not inherent in active tuberculous meningitis;
- decrease in the concentration of glucose (less than half of the glucose in the blood) and chloride (up to 110 mmol/l or less);
- after a day, a delicate fibrin film appears in the cerebrospinal fluid, in which mycobacteria are found only in 10-20% of patients.
The third period of clinical manifestations of brain tissue damage is characterized by symptoms of irritation and loss of functions from the brain substance. Symptoms of brain damage are aphasia, hemiparesis, hemiplegia, paralysis. These processes are based on progressive endarteritis of cerebral vessels with complete closure of their lumen, ischemia, and softening of the corresponding area of brain tissue.
Differential diagnosis of tuberculosis of the meninges and the central nervous system should be carried out with meningitis of another etiology: viral, meningococcal, staphylococcal. The clinical manifestations of meningoencephalitis are the same. They differ only in the composition of the cerebrospinal fluid.
The use of anti-tuberculosis drugs in the treatment of patients with tuberculous meningitis has significantly changed the clinical course and consequences of this serious disease. During the antibacterial period, patients with tuberculous meningitis were doomed. Now most patients with tuberculous meningitis can be cured. The success of treatment depends entirely on early diagnosis. The prognosis is favorable in cases where the diagnosis is made and treatment is started before the 10th day from the onset of headache. In cases of late diagnosis, the prognosis becomes unfavorable, since irreversible morphological changes are already occurring in the meninges and brain matter.
Types and symptoms of meningitis
Meningitis in adults is classified according to several criteria, including etiology, origin, rate of development and nature of the disease. Based on the causes of the development of the disease, there are:
- Bacteria
- Viruses
- Fungi
In some cases, the development of a mixed form of the disease is noted. It is characterized by the activation of several types of viruses and bacteria simultaneously.
Based on their origin, they distinguish between primary and secondary types of pathology. The first is the result of damage to the meninges by infectious agents, and the second is a complication of concomitant diseases.
The rate of development of pathogenic processes also plays a role in the classification of pathology. On this basis, the disease is divided into several types:
- Acute meningitis. It is caused by purulent infectious processes and is characterized by a sharp increase in body temperature. It is characterized by an acute increase in clinical symptoms with a rapid deterioration of the patient's condition. In the absence of timely assistance, the patient may die within two days after the onset of the disease.
- Subacute meningitis. Inflammatory processes in this type of pathology are sluggish in nature. Their development can be paroxysmal, with a period of rise and fall of the clinical picture. They appear gradually over 1-2 months.
- Chronic meningitis. The disease is benign. The duration of development of pathological processes ranges from several months to 20-25 years. During this time they have an intermittent character.
- Reactive meningitis. The disease develops rapidly due to damage to the body by meningococci, streptococci, pneumococci, as well as in the presence of sinusitis, pneumonia, otitis and other diseases. Death occurs within one day.
Understanding the nature of the course of pathological processes during meningitis in adults allows us to prescribe the most effective treatment tactics. According to this parameter, the disease is divided into several types:
- Serous meningitis. This is an aseptic type of pathology, during which a high level of lymphocytes is noted in the cerebrospinal fluid. Among the subtypes of this form of the disease are viral and tuberculous meningitis. The first is accompanied by the development of pathological processes due to mumps or the action of the herpes virus. The disease occurs with severe intoxication of the body. With tuberculous inflammation of the membranes, the disease occurs against the background of activation of Koch's bacilli. Often it occurs in a chronic or subacute form, which is not dangerous to the health of people around.
- Purulent meningitis. This form of the disease develops when meningococcal bacteria enter the body. The accumulation of purulent masses contributes to a sharp deterioration in the patient’s condition and the rapid spread of pathological agents throughout the body.
The development of inflammatory processes in the meninges is accompanied by a number of specific and nonspecific clinical signs. These include:
- a sharp deterioration in health;
- fast fatiguability;
- general weakness;
- tinnitus;
- increased body temperature above 39°C;
- loss of appetite, weight loss;
- vomiting that does not bring relief;
- migraines with varied localization and high intensity;
- a characteristic burgundy-colored rash on the skin;
- cognitive impairment;
- loss of consciousness;
- skin hyperesthesia;
- convulsions;
- stiffness of the muscles of the back of the head and neck.
The symptoms of diseases of different etiologies have their own characteristics. Viral meningitis develops over several days. Initially, the disease has signs of a cold, but over time the clinic acquires a specific character. When the body is affected by bacteria, symptoms increase much faster.
Important information
If any signs of meningitis are detected in adults, you should immediately consult with specialized specialists. Detection of pathological processes in the early stages of disease development significantly improves the prognosis in the future.
Symptoms of the disease
The disease begins acutely with an increase in temperature to 39–40 degrees and is accompanied by chills.
The main symptoms in the first stages of the disease:
heat;- chills;
- Strong headache;
- nausea and vomiting not dependent on food intake;
- positive reaction to Kernig and Brudzinsky tests;
- muscle stiffness in the back of the neck and back;
- convulsions.
By the third day, the intensity of symptoms increases, and increased sensitivity to auditory, tactile and visual stimuli is added. The patient complains of too bright light, loud sounds and painful touch.
More severe disorders often appear, such as paralysis and partial memory loss. This suggests that the inflammation spread to the brain tissue and led to the development of meningoencephalitis.
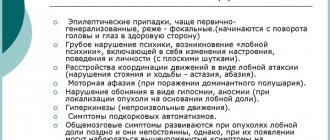
Depending on the location of the source of inflammation, the following symptoms are added::
- visual and hearing impairment;
- hallucinations;
- rave;
- psychomotor agitation;
- double vision.
Important! If you notice these symptoms, seek medical attention immediately. Timely initiation of treatment will avoid serious complications.
Diagnosis of the disease
The first suspicions that a person has meningitis are noted when intense headaches, vomiting without nausea, an increase in body temperature above 39°C, a specific rash and meningeal symptoms appear. In order to confirm the diagnosis, a number of instrumental and laboratory research methods are prescribed. These include:
- general blood and urine analysis;
- blood chemistry;
- coagulogram, which makes it possible to assess the patient’s blood clotting parameters;
- bacterial seeding of cerebrospinal fluid and nasopharyngeal mucus to determine pathogenic microflora;
- encephalography using contrast agents;
- electrocardiography;
- chest x-ray;
- computed and magnetic resonance imaging.
Diagnostic methods
To make a diagnosis of purulent meningitis, the following tests are performed :
- blood analysis;
- Analysis of urine;
- cerebrospinal fluid puncture.
First of all, pay attention to the presence of meningeal symptoms:
Stiffness of the muscles of the back of the neck and back, due to which the patient cannot tilt his head to his chest.- A positive reaction to the Kernig test means the patient cannot fully straighten his legs.
- A positive reaction to the Brudzinski test - the patient does not control the flexion of the legs at the knees and hip joint.
Also, upon examination, the extinction of the abdominal reflexes and the strengthening of the deep ones are revealed.
In some cases, a rash appears on the body , especially in the mouth area. This symptom is more typical for children, but also occurs in adults. If present, fragments of the rash are also taken for analysis.
When collecting cerebrospinal fluid, its cloudy color, the presence of pus and the high pressure with which it flows out are noted. Laboratory tests reveal a high protein content and neutrophilic pleocytosis in the cerebrospinal fluid, low sugar and chloride content, and a high number of leukocytes in the blood and an increase in ESR.
If secondary meningitis is suspected, an x-ray of the lungs and sinuses is performed to identify the original source of infection.
Treatment
Therapy in adults involves the use of combined drug treatment. The main groups of drugs in this case are:
- Broad-spectrum antibacterial agents - Cefotaxime, Cefuroxime, Banepenem, Ampicillin, Vancomycin, Amoxicillin.
- Antiviral drugs - Oseltamivir, Acyclovir, Remantadine.
- Antifungal drugs - Amphotericin, Fluconazole.
- Non-steroidal anti-inflammatory drugs - Nimesulide, Ibuprofen, Indomethacin.
- Diuretics – Lasix, Furosemide, Diacarb.
- Analgesics – Paracetamol, Pentalgin, Ketanov, Baralgin.
- Corticosteroids – Dexamethasone, Prednisolone, Hydrocortisone, Betamethasone.
Also, treatment of meningitis in adults may be accompanied by the prescription of solutions to detoxify the body. The use of colloids and crystalloids helps eliminate toxins, which are products of the decomposition of viruses and bacteria.
Treatment of meningitis
Meningitis is a direct indication for hospitalization of the patient. Therapeutic tactics are etiotropic in nature and are aimed at eliminating the primary source of infection. The effect of etiotropic treatment must be assessed by analyzing clinical data and the results of microscopic examination of the cerebrospinal fluid.
In the treatment of bacterial meningitis, both in children and adults, the main emphasis in drug therapy is on the prescription of antibacterial drugs in large doses. The choice of antibiotic depends on the causative agent of the infection.
If the inflammatory process is of viral origin, it is important to use antiviral drugs, in particular Viferon. And with fungal etiology, meningitis is treated with antimycotic drugs.
Along with therapeutic measures aimed at eliminating the cause of the disease, the use of detoxification and restorative therapy is very important.
In order to prevent seizures, the use of lytic mixtures (pipolfen, aminazine, novocaine) is recommended. If the course of meningitis is complicated by cerebral edema or Waterhouse-Friderichsen syndrome, it is advisable to use corticosteroids (dexamethasone). Also, if necessary, symptomatic treatment of pain and hyperthermia is carried out.
Complications and consequences of meningitis in adults
Various forms of meningitis are dangerous due to the development of severe complications. Among them, the most dangerous are:
- Infectious-toxic shock. Its development is due to the absorption by cells of pathogenic microorganisms and their metabolic products. This condition is accompanied by a sharp drop in body temperature, the appearance of hyperesthesia, increased agitation and breathing problems. In the absence of assistance, the patient's death occurs within 2-3 hours.
- Brain swelling. The pathology develops acutely, with a rapid increase in body temperature and impaired consciousness of the patient. Characteristic signs of pathogenic processes are loss of consciousness, sudden jumps in blood pressure and changes in heart rate, pulmonary edema, and increased breathing. Death occurs as a result of paralysis of the respiratory muscles.
- Hydrocephalus, hormonal imbalance, deafness, paresis, paralysis, epilepsy. These conditions act as consequences of past illnesses. They can lead to serious complications that reduce quality of life. To minimize the risk of developing these pathologies, you need to promptly seek help from doctors.
Vaccination against meningitis
The main method of preventing the disease is the regular use of vaccines that prevent damage to the body by meningococci, as well as chickenpox viruses, measles, rubella, pneumococcal and hemophilic pathogens. Most vaccinations are performed in childhood according to the vaccine calendar. Vaccination against meningococcal infection is carried out every 3 years.
Today, inflammatory processes in the meninges are a serious problem in medicine. If you detect the first signs of pathology, you should immediately seek help from specialized specialists. Timely treatment prevents the development of dangerous complications and improves the prognosis in the future.
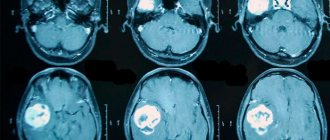
Which method of diagnosing meningitis to choose: MRI, CT, angiography
Selection method
- MRI.
Is MSCT of the brain informative for inflammation of the membranes?
- Usually normal picture
- There may be minor hydrocephalus or hyperdense substrate in the basal cisterns (purulent exudate).
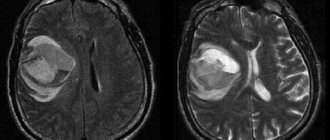
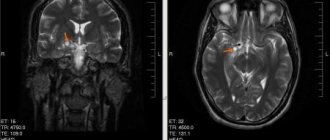
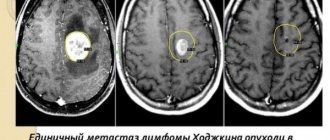
What will MRI images of the brain show in meningitis?
- Increased signal intensity from the pia mater and sometimes from the dura mater on post-contrast images
- Hyperintense areas on T2-weighted images and on native T1-weighted images (pus or serous effusion in the subdural or subarachnoid space)
- Purulent meningitis is usually localized in the frontoparietal region, tuberculous meningitis is usually localized in the basal regions