Human anatomy is undoubtedly a major core subject for study in medical schools. Despite the fact that normal human anatomy is a discipline that stood at the origins of the development of medicine, a large number of scientific works still appear that make adjustments to modern anatomical atlases.
It would seem that human anatomy cannot change so quickly with the course of evolution, but our understanding of it is constantly improving as new research methods appear - evidence of this is provided by ever new versions of the anatomy atlas.
Atlas of anatomy Sinelnikova R.D. in 4 volumes, this is perhaps the most authoritative and time-tested source of knowledge on this topic. It is constantly republished, delighting us with its visual illustrations and text accessible to everyone. Many students tried to download Sinelnikov’s atlas for study, but the links either did not work, or there was a virus in the folder... We solved this problem by making a website dedicated to this source.
The main goal of studying human anatomy is to create a fundamental knowledge base for students for further study of other medical disciplines. It is difficult to imagine mastering a curriculum in physiology, pathological physiology, pathological and topographic anatomy, operative surgery, and a whole range of clinical disciplines without a thorough study of normal human anatomy.
It is very important for a student to have a visual image of the material studied; for this it is necessary to study human anatomy in pictures. The main feature of this science. of course, is the structuring of its sections and subsections, as well as a clear systematization of the entire nomenclature.
Thus, we can distinguish the following directions that correspond to each system:
- osteology (section on the bones of the human skeleton). Studies the skeleton, both as a whole mechanism and as individual bones. There is also a study of age-related changes in bones.
- syndesmology (joints, ligaments). An extremely important section for future orthopedists and traumatologists.
- myology (muscular system). He studies not only the structure, but also the development and physiology.
- splanchnology (internal organs). Includes the anatomy of the endocrine, digestive, respiratory, excretory and genitourinary systems.
- angiology (vessels and their derivatives). Information is presented on the structure of blood and lymphatic vessels.
- neurology (central and peripheral nervous system). An extremely important section for successful diagnosis of diseases and perhaps the most difficult.
- aesthesiology (the science of the sense organs). Everything about vision and hearing. And also about taste, olfactory and tactile sensitivity. Closely related to neurology.
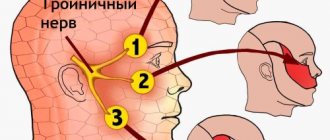
Branches of the trigeminal nerve: mandibular nerve
The mandibular nerve (n. mandibularis) is the third branch of the trigeminal nerve, is a mixed nerve and is formed by sensory nerve fibers coming from the trigeminal ganglion and motor fibers of the motor root (Fig. 1, 2). The thickness of the nerve trunk ranges from 3.5 to 7.5 mm, and the length of the extracranial part of the trunk is 0.5-2.0 cm. The nerve consists of 30-80 bundles of fibers, including from 50,000 to 120,000 myelinated nerve fibers.
Rice. 1. Mandibular nerve, left view. (Mandibular ramus removed):
1 - auriculotemporal nerve; 2 —
middle meningeal artery; 3 - superficial temporal artery; 4 - facial nerve; 5 - maxillary artery; 6—inferior alveolar nerve; 7 - mylohyoid nerve; 8—submandibular node; 9— internal carotid artery; 10—mental nerve; 11 - medial pterygoid muscle; 12—lingual nerve; 13— drum string; 14 - buccal nerve; 15 - nerve to the lateral pterygoid muscle; 16 - pterygopalatine node; 17 - infraorbital nerve; 18 - maxillary nerve; 19 - zygomaticofacial nerve; 20—nerve to the medial pterygoid muscle; 21 - mandibular nerve; 22 - chewing nerve; 23 - deep temporal nerves; 24 - zygomaticotemporal nerve
Rice. 2. Mandibular nerve, view from the medial side:
1—motor root; 2—sensitive root; 3—greater petrosal nerve; 4— lesser petrosal nerve; 5—nerve to the tensor tympani muscle; 6, 12— drum string; 7—auriculotemporal nerve; 8—inferior alveolar nerve; 9—mylohyoid nerve; 10—lingual nerve; 11 - medial pterygoid nerve; 13 - ear node; 14 - nerve to the muscle that strains the velum palatine; 15 - mandibular nerve; 16 - maxillary nerve; 17 - optic nerve; 18 - trigeminal node
The mandibular nerve provides sensory innervation to the dura mater of the brain, skin of the lower lip, chin, lower part of the cheek, anterior part of the auricle and external auditory canal, part of the surface of the eardrum, mucous membrane of the cheek, floor of the mouth and anterior two-thirds of the tongue, teeth of the lower jaw , as well as motor innervation of all masticatory muscles, the mylohyoid muscle, the anterior belly of the digastric muscle and the muscles that strain the tympanic membrane and the velum palatine.
From the cranial cavity, the mandibular nerve exits through the foramen ovale and enters the infratemporal fossa, where it divides near the exit site into a number of branches. Branching of the mandibular nerve is possible either according to the scattered type (more often with dolichocephaly) - the nerve breaks up into many branches (8-11), or according to the main type (more often with brachycephaly) with branching into a small number of trunks (4-5), each of which is common to several nerves.
Three nodes of the autonomic nervous system are associated with the branches of the mandibular nerve: the ear (ganglion oticum); submandibular (ganglion submandibulare); sublingual (ganglion sublinguale). From the nodes postganglionic parasympathetic secretory fibers go to the salivary glands.
The mandibular nerve gives off a number of branches.
1. The meningeal branch (r. meningeus) passes through the foramen spinosum along with the middle meningeal artery into the cranial cavity, where it branches in the dura mater.
2. The masticatory nerve (n. massetericus), predominantly motor, often (especially in the main form of branching of the mandibular nerve) has a common origin with other nerves of the masticatory muscles. It passes outward over the upper edge of the lateral pterygoid muscle, then through the notch of the mandible and is embedded in the masseter muscle. Before entering the muscle, it sends a thin branch to the temporomandibular joint, providing its sensitive innervation.
3. Deep temporal nerves (n. temporales profundi), motor, pass along the outer base of the skull outward, bend around the infratemporal crest and enter the temporal muscle from its inner surface in the anterior (n. temporalis profundus anterior) and posterior (n. temporalis profundus posterior ) departments.
4. The lateral pterygoid nerve (p. pterygoideus lateralis), motor, usually leaves a common trunk with the buccal nerve, approaches the muscle of the same name, in which it branches.
5. Medial pterygoid nerve (n. pterygoideus medialis), mainly motor. It passes through the ear ganglion or is adjacent to its surface and follows forward and down to the inner surface of the muscle of the same name, into which it penetrates near its upper edge. In addition, near the ear node, it gives the nerve to the muscle that tenses the velum palatine (n. musculi tensoris veli palatine), the nerve of the muscle that tenses the tympanic membrane (n. musculi tensoris tympani), and the connecting branch to the node.
6. The buccal nerve (p. buccalis), sensitive, penetrates between the two heads of the lateral pterygoid muscle and runs along the inner surface of the temporal muscle, spreading further along with the buccal vessels along the outer surface of the buccal muscle to the corner of the mouth. On its way, it gives off thin branches that pierce the buccal muscle and innervate the mucous membrane of the cheek (to the gum of the 2nd premolar and 1st molar) and branches to the skin of the cheek and corner of the mouth. Forms a connecting branch with the branch of the facial nerve and with the ear ganglion.
7. The auriculotemporal nerve (p. auriculotemporalis), sensitive, starts from the posterior surface of the mandibular nerve with two roots covering the middle meningeal artery, which then connect into a common trunk. Receives from the ear ganglion a connecting branch containing parasympathetic fibers. Near the neck of the articular process of the lower jaw, the auriculotemporal nerve goes upward and through the parotid salivary gland enters the temporal region, where it branches into terminal branches - the superficial temporal (rr. temporales superficiales). Along its path, the auriculotemporal nerve gives off the following branches:
1) articular (rr. articulares), to the temporomandibular joint;
2) parotid (rr. parotidei), to the parotid salivary gland. These branches contain, in addition to sensory ones, parasympathetic secretory fibers from the ear ganglion;
3) the nerve of the external auditory canal (n. meatus acustuci externi), to the skin of the external auditory canal and the eardrum;
4) anterior auricular nerves (auriculares anteriores), to the skin of the anterior part of the auricle and the middle part of the temporal region.
8. Lingual nerve (p. lingualis), sensitive. It originates from the mandibular nerve near the foramen ovale and is located between the pterygoid muscles anterior to the inferior alveolar nerve. At the upper edge of the medial pterygoid muscle or slightly lower, the chorda tympani (chorda tympani), which is a continuation of the intermediate nerve, joins the nerve. As part of the chorda tympani, the lingual nerve includes secretory fibers that go to the submandibular and sublingual nerve ganglia, and taste fibers to the papillae of the tongue. Next, the lingual nerve passes between the inner surface of the lower jaw and the medial pterygoid muscle, above the submandibular salivary gland along the outer surface of the hyoglossus muscle to the lateral surface of the tongue. Between the hypoglossal and genioglossus muscles, the nerve splits into terminal lingual branches (rr. linguales).
Along the course of the nerve, connecting branches with the hypoglossal nerve and the chorda tympani are formed. In the oral cavity, the lingual nerve gives off the following branches:
1) branches to the isthmus of the pharynx (rr. isthmi faucium), innervating the mucous membrane of the pharynx and the posterior part of the floor of the mouth;
2) the hypoglossal nerve (n. sublingualis) departs from the lingual nerve at the posterior edge of the hypoglossal node in the form of a thin connecting branch and spreads forward along the lateral surface of the sublingual salivary gland. Innervates the mucous membrane of the floor of the mouth, gums and sublingual salivary gland;
3) lingual branches (rr. linguales) pass along with the deep arteries and veins of the tongue through the muscles of the tongue forward and end in the mucous membrane of the apex of the tongue and its body to the border line. As part of the lingual branches, taste fibers pass to the papillae of the tongue, passing from the chorda tympani.
9. Lower alveolar nerve (n. alveolaris inferior), mixed. This is the largest branch of the mandibular nerve. Its trunk lies between the pterygoid muscles behind and lateral to the lingual nerve, between the mandible and the sphenomandibular ligament. The nerve enters, together with the vessels of the same name, into the mandibular canal, where it gives off multiple branches that anastomose with each other and form the lower dental plexus (plexus dentalis inferior) (in 15% of cases), or directly the lower dental and gingival branches. It leaves the canal through the mental foramen, dividing before exiting onto the mental nerve and incisive branch. Gives the following branches:
1) the mylohyoid nerve (n. mylohyoides) arises near the entrance of the inferior alveolar nerve into the mandibular foramen, is located in the groove of the same name in the branch of the mandible and goes to the mylohyoid muscle and the anterior belly of the digastric muscle;
2) the lower dental and gingival branches (rr. dentales et gingivales inferiors) originate from the lower alveolar nerve in the mandibular canal; innervate the gums, alveoli of the alveolar part of the jaw and teeth (premolars and molars);
3) the mental nerve (p. mentalis) is a continuation of the trunk of the lower alveolar nerve as it exits through the mental foramen from the canal of the mandible; here the nerve is divided fan-shaped into 4-8 branches, among which there are mental branches (rr. mentales), to the skin of the chin and lower labial (rr. labials inferiors), to the skin and mucous membrane of the lower lip.
The ear ganglion (ganglion oticum) is a rounded, flattened body with a diameter of 3-5 mm; located under the foramen ovale on the posteromedial surface of the mandibular nerve (Fig. 3, 4). The lesser petrosal nerve (from the glossopharyngeal) approaches it, bringing preganglionic parasympathetic fibers. A number of connecting branches extend from the node:
1) to the auriculotemporal nerve, which receives postganglionic parasympathetic secretory fibers, which then go as part of the parotid branches to the parotid salivary gland;
2) to the buccal nerve, through which postganglionic parasympathetic secretory fibers reach the small salivary glands of the oral cavity;
3) to the drum string;
4) to the pterygopalatine and trigeminal nodes.
Rice. 3. Autonomic nodes of the head, view from the medial side:
1 - nerve of the pterygoid canal; 2 - maxillary nerve; 3 - optic nerve; 4 - ciliary node; 5 - pterygopalatine node; 6 - greater and lesser palatine nerves; 7 - submandibular node; 8 - facial artery and nerve plexus; 9 - cervical sympathetic trunk; 10, 18 - internal carotid artery and nerve plexus; 11—superior cervical ganglion of the sympathetic trunk; 12 - internal carotid nerve; 13 - drum string; 14 - auriculotemporal nerve; 15 - lesser petrosal nerve; 16 - ear node; 17 - mandibular nerve; 19 - sensitive root of the trigeminal nerve; 20 - motor root of the trigeminal nerve; 21 - trigeminal node; 22 - greater petrosal nerve; 23 - deep petrosal nerve
Rice. 4. Ear node of an adult (preparations by A.G. Tsybulkin):
a — macromicroscopic specimen, stained with Schiff’s reagent, UV. x12: 1 - mandibular nerve in the foramen ovale (medial surface); 2— ear node; 3 - sensitive root of the ear node; 4 - connecting branches to the buccal nerve; 5 - additional ear nodes; 6 - connecting branches to the auriculotemporal nerve; 7 - middle meningeal artery; 8 - lesser petrosal nerve;
b — histotopogram, hematoxylin-eosin staining, UV. x10x7
The submandibular ganglion (ganglion submandibulare) (size 3.0-3.5 mm) is located under the trunk of the lingual nerve and is connected to it by nodal branches (rr. ganglionares) (Fig. 5, 6). Along these branches the preganglionic parasympathetic fibers of the chorda tympani go to the node and end there. The branches extending from the node innervate the submandibular and sublingual salivary glands.
Rice. 5. Submandibular ganglion, lateral view. (Most of the lower jaw has been removed):
1 - mandibular nerve; 2 - deep temporal nerves; 3 - buccal nerve; 4 _ lingual nerve; 5 - submandibular node; 6 - submandibular salivary gland; 7 - mylohyoid nerve; 8 - inferior alveolar nerve; 9 - drum string; 10 - auriculotemporal nerve
Rice. 6. Submandibular node (preparation by A.G. Tsybulkin):
1 - lingual nerve; 2 - nodal branches; 3 - submandibular node; 4 - glandular branches; 5 - submandibular salivary gland; 6 - branch of the submandibular node to the sublingual gland; 7 - submandibular duct
Sometimes (up to 30% of cases) a separate sublingual ganglion (ganglion sublingualis) is found.
Human anatomy S.S. Mikhailov, A.V. Chukbar, A.G. Tsybulkin
Published by Konstantin Mokanov
Inflammation of trigeminal neuralgia: causes
What are the causes of inflammation, neuritis, trigeminal neuralgia? The causes of trigeminal neuralgia are various inflammatory (inflammation), traumatic (damage), toxic, infectious (infections, including herpes - postherpetic neuralgia), allergic, infectious-allergic, metabolic effects. Compression of nerves (pinching) in bone, musculoskeletal and osteoarticular canals, prolonged microtrauma, especially in combination with hypothermia, and foci of focal infection also play an important role.
Possible causes of nerve damage
The main cause of severe pain in the chin area is neuralgia of the lower branch of the trigeminal nerve. Inflammation occurs for various reasons:
- dental diseases of the oral cavity (gingivitis, periodontal disease, periodontitis);
- caries of molars, wisdom teeth, pulpitis;
- severe hypothermia in a draft;
- stressful situations;
- infection of the salivary glands;
- pathologies of the temporomandibular joint;
- incorrect and abnormal bite.
Neuritis or neuralgia of the mandibular nerve may indicate hidden infections in the body. Sometimes the problem occurs with a sharp decrease in iron levels, chronic anemia, multiple sclerosis or herpes.
Often the cause of pain is associated with improper removal of molars. Trauma to the nerve endings occurs, compression occurs with severe swelling of the mucous membranes of the gums. The main signs by which neuralgia can be distinguished:
- sensitivity over the masticatory muscles decreases;
- swelling appears in the chin area;
- severe pain occurs along the location of the nerve;
- Teeth ache, spasms radiate to the ear, upper neck, temple.
For diagnosis, a dentist or neurologist uses tests for tactile response and pain sensitivity. Doctors evaluate the patient's ability to open and close the jaw.
Primary trigeminal neuralgia, secondary trigeminal neuralgia
There are primary trigeminal neuralgia (idiopathic, essential, typical) and secondary trigeminal neuralgia (symptomatic trigeminal neuralgia).
With primary neuralgia (mainly of central origin), attacks occur for no reason or are provoked by any movements of the facial muscles.
Secondary neuralgia is usually a complication of the primary disease, has a predominantly peripheral genesis and is often caused by pathological processes in the dentofacial area. The pain is almost constant, periodically intensifying in the form of attacks lasting up to several hours.
Features of the anatomical structure
The mandibular joint is one of the most complex in structure. This is a paired joint located on the sides of the head in the lower part of the skull. It has a compact structure that does not affect the functioning of numerous blood vessels and nerve endings. It is protected from external influences by a dense muscular frame.
The mandibular nerve (in Latin n. mandibularis) is responsible for the coordinated functioning of the joint. This is the large third part of the trigeminal ganglion, which is formed from a large number of endings, cells and axons.
Basic characteristics in anatomy:
- It is of a mixed type: it contains cells from the trigeminal nerve and sensory fibers from the motor branch.
- The thickness can reach 7 mm.
- Consists of 80 ultra-sensitive beams.
The hole through which the mandibular nerve exits the cranial cavity is called “oval”. The trunk enters a special infratemporal fossa, where it is divided into several functional parts. Depending on the genetic features of the structure, it can have from 8 to 11 branches or 5 large fibers with increased sensitivity.
Areas and organs that are innervated by the branches of the mandibular nerve:
- gums, roots of the teeth of the lower jaw (dental plexus);
- skin of the cheeks, face, chin;
- mucous membranes in the mouth;
- eardrum, ear canal, concha;
- the temporal region is predominantly at the entrance to the ear;
- salivary glands;
- papillae on the tongue;
- masticatory muscles.
The nerve provides innervation to the temporomandibular joint. The dental plexuses may pass through this place and the root of the wisdom tooth may be located. Therefore, pain of varying levels of intensity often occurs, which may indicate pulpitis or advanced caries.