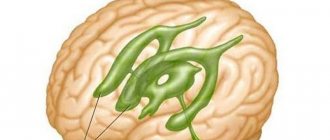
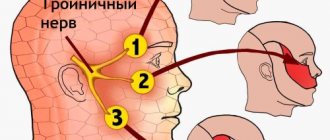
The nervous system plays one of the main roles in the human body. It is impossible to imagine how the body would move, how organs and systems would work, how feelings would be transmitted, if there were no innervation system in the body. The basis of this system is nerves. Most of the nerve pathways belong to the brain. Essentially all the nerves come out of the cranium. Of these there are 12 pairs, one of which is the ternary nerve. The ternary nerve tract is a complex plexus that is divided into three main nerves: the orbital, mandibular and maxillary nerves. In order to understand the functional significance and structure of the latter, it is necessary to first study the anatomical features of the ternary nerve tract.
Anatomy of the ternary nerve
The ternary is the fifth pair of cranial nerve tracts. Essentially it is mixed, that is, it contains various fibers, among which are the following types:
- sensory fibers are of two types - centripetal and afferent;
- motor fibers or centrifugal (thanks to these fibers, information passes to the brain through electrical impulses about pain sensations in both superficial tissues, for example, information about skin pain, burns, and information from deeper structures, such as proprioceptive receptors.
Tissue movement is carried out due to the presence of the motor nucleus, which provides the innervation system predominantly to the masticatory muscles. The ternary branches off from the brain in the pons. At the exit from the cranium, most of the fibers pass along the pyramid of the temporal bone. It is at the top of this bone formation that the nerve fibers are divided into three branches, which represent separate nerves, such as:
- Orbital;
- Mandibular;
- Maxillary nerve.
The ternary, together with all three branches, are of particular interest to neurologists; it is also the main one when examining facial paralysis. This is due to the fact that this path powers the entire human face, ensures motor activity of muscle tissue, sensitivity and conduction of impulses to the brain and back. It is quite often affected by exposure to negative factors, such as severe hypothermia of the facial part or the entire head, as well as injury or disease of the musculoskeletal system. Therefore, it is very important to monitor the health of the nervous system and avoid harmful factors.
Trigeminal neuralgia
Neuralgia is a paroxysmal pain that occurs along the sensory branches - mandibular and maxillary. It is unilateral in nature and is accompanied by painful contractions of the facial muscles and tics.
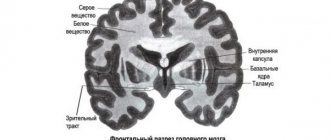
Pain syndrome is associated in 80-90% of cases with compression of the nerve along its path through the brain structures. Most often, irritation is associated with vascular pulsation or tumor growth. Rare causes of neuralgia are considered multiple sclerosis, which causes demyelination of the root at the level of the bridge.
Helpful information
Almost 60% of patients experience a cutting pain that shoots from the corner of the mouth to the corner of the jaw, along the third branch of the trigeminal nerve.
In another 30%, the attack begins from the upper lip or canine fossa to the eye or eyebrow, bypassing the orbit. The symptom is characteristic of damage to the second or first branches of the trigeminal nerve.
The pain begins with an “electric shock” sensation and reaches a peak within 20 seconds before giving way to a burning residual pain that lasts up to a minute. The patients wince and grimace, as if trying to avoid a sharp shot. Most often, an attack is provoked by a light touch: a breath of wind, shaving, chewing, brushing teeth or talking.
Functional tasks of departments
Each branch performs its own functional tasks:
- Orbital branch. It is considered the first and thinnest compared to the other two. The main functional task of this branch is reception. Thanks to it, innervation of the skin of the frontal part of the face, as well as some part of the temples and crown of the head, is ensured. It supplies the upper eyelid of the eyes, the back of the nose, and individual sinuses of the bone formations of the face with nerve fibers, and partially innervates the mucous membrane of the nasal passages. This branch contains approximately thirty bundles of fibers. This branch also enters the orbit through the outer wall of the ophthalmic sinus, where it branches into two more branches - trochlear and abducens. At the location of the superior orbital notch, the orbital ramus divides into three smaller fascicles, which are classified as lacrimal, frontal, and ciliated. This area is quite often injured due to its close location to the eye sockets, which are often injured by mechanical damage;
- Maxillary branch. The maxillary nerve exits the cranial cavity through the oval window. Thanks to this hole, the nerve pathway penetrates into the pterygopalatine fossa. The path then lies along this fossa and reaches the canal on the lower wall of the orbit. It then exits onto the superficial tissues of the face through the inferior orbital foramen. At this point, the maxillary branch divides into smaller fibrous bundles that intertwine with the facial nerves. Thus, the maxillary nerve enters the orbit through the inferior orbital fissure. The main functional task of this branch is to ensure the conduction of impulses from the skin of the lower eyelid, upper lip and lateral surface of the face. It is from the maxillary branch that nerves such as the zygomatic branch depart, as well as the superior alveolar branch, which forms a plexus near the teeth. This area is injured only in the case of severe injuries to the head, facial area, skull, neuritis, surgical interventions in the area of the teeth and nearby sinuses;
- Mandibular branch. It is considered the most complex plexus of the fifth pair. It includes almost the entire part of motor activity, as well as sensory fibers. The location features make it possible to innervate the muscle tissue of the lower jaw, as well as superficial structures and the skin of this area. At the exit from the cranium, the nerve bundle divides into two paths. One goes to the chewing muscles, the other to the mucous membrane of the cheeks and oral cavity. Doctors often consider this branch to be the main continuation of the trinity.
Thus, innervation of the facial part of the head, muscle tissue of the jaw, eyes, and nose is formed. To prevent damage to the nerve plexuses, it is recommended to avoid traumatic situations and promptly treat psychological disorders. Otherwise, defeat of the fifth pair leads to facial paralysis.
Symptoms
With inflammation of the submandibular nerve, symptoms are usually determined depending on the location of the pathological process. In most cases, acute pain occurs, which radiates along the affected fibers. But when the maxillary nerve is pinched, the symptoms may differ from the manifestations of mandibular neuralgia.
Traditionally, in addition to pain, the patient with neuritis decreases or increases the sensitivity of a particular part of the face.
Uneven contraction or tonic tension (spasm) of local muscle fibers is possible.
Signs of inflammation of the upper jaw
When the nerves of the upper jaw are damaged, sensitivity in the area decreases:
- maxillary sinus;
- upper cheek;
- lower eyelid;
- outer corner of the eye;
- side of the face;
- oral mucosa on the upper jaw;
- upper jaw.
The intensity of pain when nerves and jaw are damaged depends on the characteristics of the disorder. This symptom is acute and aching in nature. The pain may spread towards the eye, indicating damage to the entire trigeminal nerve. Also, with this localization of the pathological process, tic of the lower eyelid is often observed.
Signs of inflammation of the mandibular nerve
When the mandibular nerve fibers are damaged, symptoms appear as:
- decreased sensitivity in the area of the lower jaw and chin;
- paresis or paralysis of the muscles that provide chewing function;
- facial asymmetry.
If the nerve fibers of the lower jaw are affected, the patient experiences increased sensitivity of the hard tissue and mucous membrane to food or palpation.
Such susceptibility is observed both along the entire length of the affected fibers and in the following areas:
- gums;
- teeth;
- mandibular bone;
- language;
- sublingual area.
If paresis or paralysis develops, then a weak bite and the inability to pull the lower jaw upward are of concern. Due to the latter disorder, the patient's mouth remains constantly open.
Diagnostics
If damage to the mandibular nerve is suspected, an external examination of the patient and palpation of the problem area are first performed. This form of neuritis is indicated by the inability to close the jaws, muscle spasms, and painful sensations that occur when touched.
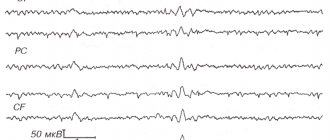
Additionally, CT, MRI and electromyography are performed. The first two methods help determine the causes of neuritis and identify the localization of the pathological process. EMG assesses the degree of conduction of nerve fibers and allows one to differentiate neuralgia from other pathologies that have similar symptoms.
Principles of pathology treatment
The main goal of treatment procedures is to relieve pain in the patient. Basically, doctors give preference to drug treatment, but physiotherapeutic procedures – treatment with dynamic currents, ultraphoresis, etc. – have an important positive effect.
Taking pharmacological agents helps relieve pain attacks. Initially, the doses of drugs are quite large, but subsequently they are reduced to reduce hepatotoxic and nephrotoxic effects.
Main classes of medications for treatment:
- Antiepileptic drugs;
- Antispasmodic and anticonvulsant drugs;
- B vitamins and antidepressants;
Medical specialists give preference to Finlepsin, Baclofen and Lamotrigine, since these drugs have shown the greatest effectiveness in the treatment of such pathology.
When the pain intensity is high, blocks of the corresponding nerve are often performed. This procedure is performed by injecting an anesthetic in close proximity to a nerve or ganglion to relieve pain.
The procedure is carried out in two stages, with two injections: intradermal and periosteal injection. The drugs of choice are Ledocaine and Diprosan, however, performing this procedure on your own is strictly prohibited, as there is a high probability of damage to important structures.
Symptom complex of lesion
The pain associated with damage or inflammation of this nervous structure is extremely intense, which causes significant discomfort for the patient. Often the ternary nerve can cause intense pain in the upper or lower jaw.
Such pain practically does not go away without treatment, so it is important to find a specialist who will prescribe quality treatment. In addition, there are points on the face that allow you to determine the level of damage - a separate root or the entire nerve as a whole.
Often, pathology occurs due to organic changes at the exit sites of the trigeminal nerve, since the nerve located there is most susceptible to compression and further inflammation. This may be indicated by pain around the eyes or nose.
The neuralgic condition is accompanied by a feeling of pain, which is similar to electric shocks. The pain may also spread to the cheek, forehead, or jaw areas. It is important to determine the source of trigeminal nerve damage in order to alleviate and eliminate discomfort.
Causes of pain
Pain can occur for various reasons, which may not go away on its own without treatment. For example, neuralgia can occur due to close contact between a nerve and a vessel (vein or artery), which will lead to inflammatory reactions. In addition, tumors can compress nerve structures, which will certainly lead to excessive irritation of the receptors. Remember that the trigeminal nerve is extremely sensitive to various pathological influences.
The symptom complex of neuralgia that affects the tertiary nerve is as follows:
- The appearance of “shooting” pain in the facial area;
- Changes in the sensitivity of the skin of the facial area;
- The pain intensifies with chewing, touching, and activity of the facial apparatus;
- The occurrence of paresis (an extremely unlikely situation);
- Painful sensations appear only on one side;
Another cause of pain may be pinched nerve structures. In such situations, the duration of pain can vary from a few seconds to hours. Such neuropathies are caused by unsuccessful plastic or dental operations, during which a pathological change in the surrounding structures occurred.
In this case, the patient is in an anxious state, which significantly affects the course of treatment. The patient is worried about not only his physical condition, but also his aesthetic one. Such worries can only intensify the pain experienced. It is important to ensure that the branches of the trigeminal nerve do not spread infectious agents between each other.
In addition to the mechanical nature of the cause, the trigeminal facial nerve can be affected by viral agents.
For example, a special herpes virus, which causes shingles, is capable of destroying the skin down to the nerve roots.
You can suspect herpes zoster (zoster disease) by:
- Herpetic rash on the skin;
- Changes in skin color and the appearance of edematous manifestations;
- Formation of bubbles with liquid of varying turbidity;
As you can see, there are a number of reasons that can cause neuralgia of the corresponding nerve. It is important not only to relieve pain, but also to get rid of the cause, and only a competent medical specialist can cope with this task.
Remember that the maxillary nerve and the infraorbital nerve lie extremely close, so if only one part is inflamed, the process can spread lower. It is extremely important that the pathology does not damage other cranial nerves, as this can lead to disruption of other vital functions of the human body.