Most often, the body reports malfunctions by the occurrence of pain. Pain can affect any part of the body and be of a completely different nature. When a person experiences shooting pain in the area of the eyes, temples, and ears, as a rule, we are talking about nerve damage.
There are many neuralgic facial pathologies that have similar symptoms. A very rare type of it is temporo-auricular neuralgia or Lucy Frey syndrome.
What is neuralgia of the auriculotemporal nerve?
From the name of the disease it is clear that it affects the nerve. Nerves in our body are a kind of conductors. They transmit signals from the brain throughout the body. Their network is represented by dozens of fibers, united in broad groups.
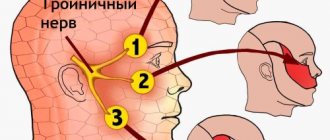
The network of nerves leaving the brain is called cranial. They are responsible for vision, hearing, smell, facial sensitivity and other important functions of the body. Part of the cranial system is the group of trigeminal nerves .
It is one of its many branches that is the auriculotemporal nerve. Its path runs through the temporal region and the front of the ear (through the concha and skin). It does not pass separately and is connected by other nerves of the cranial group. Thanks to it, the described areas of the body become sensitive.
Neuralgia of the auriculotemporal nerve is a rare disease. The disease is often called "Frey's syndrome" or "Frey-Bayarger syndrome" . This is due to the fact that the disease was first described by the French psychiatrist Bayarger. Later, in 1923, the Polish doctor Lucy Frey gave the set of symptoms considered by the Frenchman a more complete description and called them “auriculotemporal nerve syndrome.” Subsequently, this disease began to be named after Dr. Frey, and to this day this neurological pathology is called “Frey syndrome.”
It is worth noting that by “Frey's syndrome” doctors understand a specific set of complaints, the main one of which is sweating. That is, we are not talking about pain. The syndrome implies a specific manifestation of the disease - increased sweating and a number of related symptoms.
Neuritis symptoms
The clinic of neuritis is characterized by dysfunction of the innervated structures. Since most nerves are mixed, when they are damaged in the innervation zone, flaccid paresis (paralysis), muscle atrophy, decreased and loss of reflexes, impaired sensitivity and autonomic disorders (swelling, cyanosis, increased sweating, depigmentation, hair loss) occur.
With neuritis of the facial nerve, damage to the root or trunk of the facial nerve occurs at various levels, manifested by homolateral paresis or paralysis of the facial muscles.
Etiology of the disease
In medical practice, the main cause of the development of neuralgia of the auriculotemporal nerve is considered to be damage to the parotid salivary gland . It, in turn, can be caused by a number of the following reasons:
- Damage during surgery on the parotid gland.
- Postoperative complications.
- Jaw injuries (localized in the parotid-masticatory areas).
- Infectious diseases affecting the parotid glands.
Operations usually mean radical treatment of infectious mumps. During surgical treatment, a number of microscopic nerves in the temporal region are removed. Thanks to the regenerative properties of the body, these nerves are restored over time.
But in some cases, a failure occurs, and regeneration occurs due to their growth into the sweat glands on the skin. This explains the typical manifestation of Lucy Frey syndrome - increased sweating . A kind of replacement of the sweat glands with salivary glands occurs.
The mechanism for the development of postoperative complications is approximately the same: autonomic and other nerve fibers grow into skin scars, followed by irritation of the autonomic fibers of the greater auricular and auriculotemporal nerves.
Also, a prolonged inflammatory-purulent process can lead to the development of neuralgia . In particular, the complicated course of infectious parotitis. The process follows the same pattern. Due to the progression of the disease, part of the salivary glands begins to collapse, causing destructive changes in the auriculotemporal nerve that innervates it. Moisture and sweat are directly released on the face due to the fact that the nerve endings responsible for various functions grow together with sweat fibers.
Thus, inflammation of the auriculotemporal nerve is a specific disease. As a rule, you cannot get it just by catching a cold. Most often it occurs as a complication after surgery.
In the case of diseases that cause complications of this kind, we are talking primarily about mumps . It is not a cold, but an infectious disease and can be prevented by vaccination.
Another reason for the development of auriculotemporal neuralgia is damage to the main chain of sympathetic nerves in the neck. In extremely rare cases, Frey's syndrome can occur in newborns (most likely due to birth trauma).
Thus, the main factors in the development of neuralgia are:
- Infectious diseases.
- Postoperative complications.
- Injuries.
Causes, signs and treatment of Frey's syndrome
Frey's syndrome is a type of facial pain that is rare. What signs can be attributed specifically to this pathology, and why do those suffering from this disease hate chewing gum? By learning about the most effective methods of treating Frey's syndrome, you can get rid of the unpleasant condition faster.
Clinical picture of Frey's syndrome
Frey's syndrome is a set of some symptoms that were first described by the French psychiatrist Baillarger.
The pathology was described in more detail by the Polish scientist Lily Frey, which is why in foreign medical literature this problem is more often called “Frey-Baillarger Syndrome”.
If you look in medical dictionaries, pathology also has synonyms - auriculotemporal syndrome or parotid and temporal neuralgia.
That is, based on the name, the ear and temporal regions are affected as a result of a certain effect on the parotid salivary glands and, as a result, damage to the sympathetic and parasympathetic nerve fibers passing here is observed.
Why does Frey's syndrome appear?
SindromFrey is a diagnosis that in 90% of cases is given to patients due to an unforeseen complication of surgical intervention on the parotid salivary glands or others located within 1-3 cm of tissue. Often, after operations performed in the cervical spine, symptoms of Frey's syndrome appear.
Since, as a result of the surgeon's actions, the nerve endings may be cut in some way, their further development is disrupted, and the nerve fibers may grow excessively, causing discomfort to the patient, or join other glands, changing their own function, thereby also causing inconvenience.
In addition to incorrect actions of the surgeon, risk factors for the development of parotid neuralgia include:
- injuries and tumors of the neck and head;
- inflammatory processes;
- neuralgia of nearby areas.
There are frequent cases of the disease manifesting itself in people who are fond of piercing and scarring.
Neuralgia of the parotid and temporal region is a disease of adults; in rare cases, it is observed in newborns. The causes of the anomaly in children are birth injuries that lead to nerve compression. In persons under 30 years of age, the pathology, if it is not congenital, is not recorded in any source.
How not to miss the development of auriculotemporal syndrome?
Many patients notice signs of Frey's Syndrome several months after surgery. Symptoms are initially temporary and begin more often during meals, that is, during the process of chewing food. Signs of pathology disappear, accordingly, only when the chewing process is completed.
A person suffering from this disease can be recognized by the following signs:
- increased sweating in the ear area;
- redness and hyperthermia of the affected area;
- pain spreading to the lower face and ear;
- numbness of some areas of the skin;
- feeling of stuffiness in the ear.
In addition to the process of chewing, massage or involuntary pressure in the area under the jaw can lead to these unpleasant sensations.
Attacks occur more frequently, and if you do not respond to them, the symptoms will become more pronounced.
With obvious progress of neuralgia, Frey's syndrome will make its existence known even after minor stress or minor hypothermia. Therefore, it is better not to postpone a visit to the dentist.
How is the diagnosis done?
In order to accurately determine Frey's syndrome, it is necessary to exclude a number of other diseases, sometimes similar in several symptoms.
To do this, after an examination, which includes several otolaryngological methods, and collection of data from the patient, specific tests are performed. If at the time of an attack a 2% solution of novocaine is injected subcutaneously, the symptoms will disappear.
Or a solution of starch and iodine is applied to the affected area; when the process is stimulated, the area turns shades of blue.
As part of the diagnosis, radiography and ultrasound are required.
How to get rid of Frey's syndrome?
Parotid-temporal neuralgia can be subjected to conservative therapy and radical treatment methods. First of all, they try to get rid of the root cause of the pathology, eliminate the inflammatory or tumor process. Next, they begin to fight the symptoms of the syndrome.
There are 3 types of drug therapy:
- Analgesics, both tablets and subcutaneous injections, will help relieve pain.
- Ganglioblockers are used if there is a suspicion of excessive growth of the nerve ganglion.
- Antispasmodics and corticosteroid drugs are prescribed.
Physiotherapy procedures are used to assist drug treatment:
- Phonophoresis with corticosteroids and exposure to diadynamic currents are particularly successful.
- They use therapeutic muds and applications with natural ingredients.
If these methods remain powerless against auriculotemporal syndrome, regular injections of butolin toxin, better known in cosmetology as Botox, are used. This substance gives decent results - most symptoms disappear for the entire period of action of the drug. Typically injections are given every 9 months.
In more complex cases, it is possible to excise the nerve fibers in the problem area (maxillofacial surgery), but recently such measures have been carried out only as a last resort, when no other methods have helped. The refusal to perform operations is due to the fact that the percentage of partial loss of innervation of the face is high - by getting rid of one problem, the patient can suffer twice as much.
No one is immune from the manifestation of such a pathology. However, you can try to protect your own health by regular examination by specialists and timely treatment of pathologies. If auriculotemporal syndrome cannot be avoided, there is no need to delay treatment.
Source: https://stomastoma.ru/blog/sindrom-freja/
Clinical picture: symptoms and signs
Symptoms of the disease can be divided into two main groups:
- Pain syndrome.
- Specific manifestations.
The pain is usually localized in the temple area, in the ear, and also in the temporomandibular joint. It usually occurs during meals.
Specific manifestations include swelling in the area of inflammation (in the temple area), increased sweating and salivation, redness of the skin at the site of injury.
Typically, patients suffering from Frey's syndrome complain of:
- burning pain;
- throbbing pain that radiates to the lower jaw;
- attacks of sweating during meals (large drops of sweat appear on the forehead and temples);
- increased salivation.
In some cases, in addition to swelling and increased sweating, the patient experiences sensations of heat and tingling. The disease usually develops against the background of a so-called functional disorder of the nervous system.
All symptoms tend to manifest themselves and intensify while eating. This is due to the etiology of the disease. The patient reacts especially sensitively to sour and salty foods - they aggravate the symptoms.
Additional symptoms and manifestations that may be associated with Frey's syndrome include redness and warmth in the affected areas. This is a rare but important complaint.
Find out more about trigeminal neuralgia:
- inflammation of the nasociliary nerve and damage to the ear node;
- symptoms and diagnosis of trigeminal neuralgia;
- methods of treating the disease.
Trigeminal neuralgia (trigeminal neuralgia)
Signs
Most often, with inflammation of the trigeminal nerve, pain occurs in the jaw area and one half of the face, they are especially pronounced in the lower part of the face and jaw, in the area of the nose and eyes.
Many people experience pain for no reason, but most often it occurs after a car accident, a blow to the face, or after dental work at the dentist. In general, patients who experience such pain for the first time often think that their cause lies precisely in the teeth, because they usually begin in the area of the upper or lower jaw. However, neither treatment nor tooth extraction brings the slightest relief. The pain can be constant, sometimes intensifying, instantaneous, paroxysmal, throbbing. It can be typical and atypical. The typical type is characterized by periods of exacerbation, when the pain periodically subsides for a short time. In some patients it occurs rarely, once a day. Others are attacked every hour. The pain begins as if from an electric shock, reaches a peak within 20 seconds, lasts for some time and gradually subsides. Atypical - covers most of the face and is constant, without a period of pain subsiding. It is very difficult to treat such neuralgia.
Description
The trigeminal nerves are the fifth pair of twelve pairs of cranial nerves, their task is to provide sensitivity in the facial area. One trigeminal nerve comes from the left side of the face, the other from the right. Each of them has three branches: one innervates the eyes, upper eyelids and forehead skin, the second innervates the lower eyelids, cheeks, nostrils, upper lip and upper gums, the third provides sensitivity to the lower jaw, lower lip, gums and some masticatory muscles.
Trigeminal neuralgia can occur on its own or be a complication of any disease. The onset of a painful attack can be triggered by a light touch to the skin of the face, washing, shaving, brushing teeth, a blow to the nose, makeup, smiling, talking, chewing, and even a light blow of wind. Sometimes painful attacks follow each other with an interval of several minutes.
The cause of neuralgia is most often compression of the trigeminal nerve by the arteries or veins of the posterior cranial fossa, a vascular loop in a situation where there is a vascular anomaly, or a tumor of the cerebellopontine region. In young people, the development of trigeminal neuralgia is most often associated with multiple sclerosis, which leads to the destruction of the so-called myelin sheath of the nerve. Branches of the trigeminal nerve can also be compressed in the bony canals at the base of the skull through which they pass. Narrowing of bone canals can be congenital or acquired as a result of inflammatory processes (sinusitis, caries).
One of the common lesions of the trigeminal nerve is odontogenic neuralgia, which can last a very long time, even though the cause (malocclusion with constant trauma in the jaw joint, untreated teeth) has already been eliminated. Odontogenic neuralgia, as a rule, manifests itself as pain in the innervation zones of the second and third branches of the trigeminal nerve.
Trigeminal neuralgia should be differentiated from arthrosis or dysfunction of the temporomandibular joint, dental plexalgia, phantom toothache, multiple sclerosis, and glossopharyngeal neuralgia.
Diagnostics
The diagnosis is made based on the patient's complaints and examination by a neurologist. To rule out (detect) a tumor or signs of multiple sclerosis, magnetic resonance imaging (MRI) is prescribed. Examination with electromyography (EMG) and electroneurography (ENG) helps determine whether the patient actually has an effect on the trigeminal nerve.
Treatment
It is extremely difficult to get rid of trigeminal neuralgia; it is not always cured. But modern medicine can alleviate suffering. As a rule, a neurologist prescribes antihistamines, anticonvulsants, antispasmodics and vasodilators. Physiotherapeutic methods such as ionogalvanization with novocaine, amidopyrine, electrophoresis, ultraphonophoresis with hydrocortisone, transcranial methods of anesthesia and sedation, transcutaneous electrical stimulation, diadynamic therapy, infrared laser therapy, deep x-ray therapy help relieve pain... For dental plexalgia, treatment should begin with the prescription of general painkillers and local anesthetic action. First of all, non-narcotic analgesics are used.
For local anesthesia, local anesthetics are recommended: 5-10% anesthetic or lidocaine ointment, which is lightly rubbed into the pre-dried mucous membrane of the gums at the site of pain. The analgesic effect occurs immediately when rubbing the ointment in and lasts 15-30 minutes. You can use it 3-10 times a day.
If conservative therapy fails, surgical intervention is resorted to.
Prevention
To avoid the occurrence of trigeminal neuralgia, it is necessary to promptly treat inflammatory diseases of the paranasal sinuses, monitor the condition of the teeth and the entire dental system, do not overcool, avoid injuries, infections, intoxications and vitamin deficiencies.
© Dr. Peter
Diagnostic methods
When the first suspicious symptoms appear, the patient is recommended to consult a doctor for diagnosis.
To make an accurate diagnosis, the doctor studies all the symptoms and manifestations of the disease, the patient’s complaints, collects anamnesis, and examines the affected area. To make an accurate diagnosis, laboratory and instrumental studies are carried out , including specialized tests.
The essence of specialized tests is to carry out laboratory manipulations in order to confirm or refute the alleged diagnosis. The manipulations are aimed at identifying the body’s specific reaction to external stimuli (physical, chemical effects). Such tests are used in all branches of medicine, including neurology.
To diagnose Frey's syndrome, the following special test is used: iodine and starch are applied to the painful area . Then the salivary glands are stimulated. The test is considered positive if the treated area turns purple.
Another special test is based on the use of novocaine. The patient is injected intradermally with a 2% solution of novocaine. If the attack of pain stops, the test is considered positive.
Instrumental diagnostic methods include x-rays, ultrasound, and MRI of the affected area. All these studies are carried out to clarify the diagnosis if special tests and clinical manifestations do not provide a clear picture and confirm the disease. Such methods allow doctors to differentiate auriculotemporal neuralgia from other similar diseases.
Neuralgia treatment, how to treat neuralgia, intercostal neuralgia treatment, neuritis treatment
Complex treatment of neuritis and neuralgia (Saratov, Russia) includes a variety of effective techniques. Sarklinik knows how to treat and cure neuralgia neuritis !
Sign up for a consultation. There are contraindications. Specialist consultation is required.
Photo: Jabiru | Dreamstime.com\Dreamstock.ru. The people depicted in the photo are models, do not suffer from the diseases described and/or all similarities are excluded.
Related posts:
Vegetative vascular dystonia: treatment of VSD, how to treat VSD, symptoms, signs
Treatment of irritability and fatigue in Saratov, how to get rid of irritability
Brain stroke: ischemic, hemorrhagic, treatment, rehabilitation, consequences
Memory loss, treatment, amnesia, short-term, partial, temporary memory loss
Neuroses, neurosis, treatment of neurosis, neurasthenia, how to treat
Comments ()
How and from what should this disease be distinguished?
First of all, “Frey's syndrome” should be differentiated from other types of neurology that are similar in localization.
In particular, with neuralgia of the mandibular nerve. The diseases have similar symptoms, namely: pain in the temple and jaw.
It is also necessary to exclude ganglionopathy of the upper cervical sympathetic ganglion and neuralgia of the mandibular nerve.
Compression of the temporal nerve by a tumor can also cause similar neurological symptoms. To exclude oncology, high-precision instrumental studies are used: MRI, CT.
Treatment methods
Treatment can be either radical (surgery) or conservative (medication) . Specific tactics depend on the scale of the lesion, the stage of development of the disease, and medical history. In any case, the main goal is to eliminate the cause of the syndrome (infection, inflammation) as much as possible.
To combat symptoms use:
- Analgesics (for pain relief): analgin, sedalgin, novocaine.
- Nonsteroidal anti-inflammatory drugs (to relieve inflammation): ibuprofen, diclofenac.
- Sedatives.
- Anticholinergics.
- Vitamins of group B and C.
Physiotherapy procedures are also prescribed: electrophoresis with potassium iodide, lidase, phonophoresis 2%.
Radical treatment is sought if there is no effect from symptomatic treatment. The essence of the operation is to cut the auriculotemporal and greater auricular nerves.
What is neuralgia of the ear ganglion?
Pathology of the ear autonomic ganglion, which manifests itself in the form of paroxysms of vegetalgia and affects not only the ear, but also the ear region - neuralgia of the ear ganglion. During attacks, acute pain can radiate to the lower jaw, back of the head, shoulder girdle, arm and upper chest. May be accompanied by congestion, clicking, hypersalivation. In this case, hearing is not impaired. The pathology is diagnosed by a neurologist with the assistance of a dentist, otolaryngologist and other specialized specialists. Complex therapy includes medications for the relief of painful paroxysms, metabolic drugs, vascular and decongestants, as well as physiotherapeutic procedures and reflexology.
Possible consequences and complications
It should be understood that auriculotemporal neuralgia initially develops as a complication . In this regard, the specific consequences depend on the cause of the disease and the degree of neglect.
The stage and extent of damage can be determined by studying the symptoms. They may not include pain and may be limited to sweating and redness while eating. In this case, the stage is considered mild and can be easily treated conservatively.
In any case, it is necessary to identify the cause of such symptoms. Perhaps untreated inflammation is to blame. When it is eliminated, the symptoms should disappear. The pain can also have varying degrees of severity and occur only during eating, or be constant. In the second case, the stage is considered advanced and requires complex treatment.
Causes
There are several causes leading to ganglionitis:
Infectious pathologies
The disease manifests itself as a complication of inflammatory processes within the body that occur as a result of influenza, acute respiratory infections, inflammation of the membranes of the brain caused by adenomovirus or parainfluenza, epidemic mumps, rubella.
The causative agents of these diseases spread throughout the body through the bloodstream, affecting the hearing organs.
Toxic poisoning
Neuritis develops due to exposure to the following harmful substances in the body:
- medications (antibiotics, drugs for the treatment of cancer);
- hazardous industrial products (lead, mercury, gasoline, phosphorus, arsenic);
- nicotine and alcohol.
Traumatic brain injuries
They lead to abnormal changes in the body:
- impaired blood circulation;
- cerebral edema;
- microscopic hemorrhages from capillaries.
These phenomena affect the nerves and vessels supplying the hearing organs. The auricular nerve can be damaged by the edges of bone fragments due to injuries to the base of the skull.
Occupational hazards
This:
- prolonged stay in rooms with increased noise, for example, in workshops with industrial equipment;
- exposure to vibration noise on humans.
Age-related changes
Acoustic neuritis in older people occurs due to:
- arterial hypertension;
- insufficient supply of the arteries of the brain;
- consequences of a stroke.
In rare cases, pathology can develop against the background of allergic reactions. Neuralgia of the auditory canal is sometimes observed in divers due to injuries caused by sudden changes in pressure.
Prognosis and prevention
The prognosis will depend on the history of the disease, the stage of its development, and the totality of symptoms . With mild symptoms, the prognosis is most favorable. In case of severe pain, which is almost constant, differential diagnosis and long-term conservative treatment, including a set of procedures, are required.
Due to the fact that such neuralgia develops as a complication, the main essence of prevention is the early diagnosis and treatment of colds and viral diseases.
The development of diseases should not be allowed to occur. In the case of infectious diseases, in particular mumps, doctors recommend undergoing routine vaccination.
Symptomatic picture
Characteristic symptoms are attacks of vegetation. They occur in the ear, parotid area, or in front of the opening of the ear canal on the side of the affected area. The pain is intense or burning. It radiates to the neck, back of the head, lower jaw and shoulder girdle. Due to the mechanism of pain irradiation, it spreads to the upper part of the thoracic region and the arm on the affected side. The duration of the attack ranges from several minutes to an hour or more.
Occasionally, paroxysm is accompanied by clicking or congestion in the ear. They are caused by reflex muscle spasms of the auditory tube. Also, during an attack, hypersalivation is noted, while at rest increased salivation does not occur.
Neuralgia can be triggered by:
- Hypothermia;
- Consumption of hot food and drinks;
- High physical activity;
- Psycho-emotional stress.
Since the autonomic nervous system depends on external factors such as temperature changes, changes in daily patterns, barometric pressure, etc., the autonomic system has a rhythmic character. It occurs most often at night and in the evening. In spring and autumn, neuralgia may worsen.
Hearing function remains unchanged during the period of illness.