From the creation of the world
The most interesting discoveries in the world of neurosurgery have been made by scientists. Some of the skulls discovered at the Chauchilla necropolis in Peru clearly show signs of trepanation. Moreover, what especially surprised the researchers was that new bone tissue grew at the edges of these holes. This means that people lived after the operations he performed, and for quite a long time. Based on the shape of the holes, the researchers were able to determine that doctors were already using quite good instruments at that time. The operation itself was carried out by scraping out the bone using various chisels, nippers and conical cutters. The Incas also knew how to correct bone defects plastically using gold and silver plates.
For what reasons ancient doctors risked performing such complex operations is unclear to modern scientists. Some of them were performed to correct traumatic brain injuries, but some skulls no longer have any damage. Some of the finds found were from infants, which allowed scientists to assume that doctors tried to treat infantile convulsions using this method. And a number of the skulls belonged to young people, suggesting that neurosurgery was used for ritual activities, such as rites of passage. And the pharaohs of Egypt made such holes so that after death it would be easier for the soul to leave the body.
"Exorcism of an evil spirit." What doctors' mistakes cost patients their health?
More details
Early postoperative consequences
Frequent complications after craniotomy include bleeding. They can occur both during the surgical intervention itself and immediately after its completion. Due to the abundant blood supply to the tissues of the head, the patient can lose a significant amount of blood in a short period of time.
In this case, emergency blood transfusion (transfusion of someone else's blood) may be required. Therefore, in the preoperative period, if the patient’s condition allows, a full laboratory and instrumental examination is performed. This includes determining the blood group and Rh factor, since when massive bleeding develops, every second counts.
At the present stage of development of neurosurgical technology, unintentional damage to the brain is extremely rare. However, in some situations it is quite possible. Depending on the degree of damage (size and depth) of the brain matter, further consequences are formed. If the so-called “silent” areas are damaged, there are no manifestations, but if the integrity of the functional departments is damaged, a neurological deficit of varying severity may develop.
The brain reacts to damage (concussion, bruise or penetrating wounds) in a very similar way. Edema and swelling of its substance develops. At the histological level, this is manifested by the release of a significant amount of liquid blood from the capillary bed into the interstitial space and the “leakage” of nerve fibers by it. This leads to a significant increase in the volume of the medulla. The brain seems to be pressing on the skull from the inside. When trephination is carried out carelessly or inadequate infusion therapy, the brain substance is displaced into the trepanation hole with the development of damage, ruptures and other irreparable changes in the structure.
Considering the complexity of any intervention on the brain and the seriousness of the reasons that may be the reason for this intervention, there remains the risk of death right on the operating table. In this case, a number of circumstances that are beyond the control of medical personnel are decisive.
The duration of some operations for craniotomy is associated with the risk of complications that are not a direct consequence of the intervention itself. Firstly, these may be the consequences of a long stay in a narcotic sleep. Which is associated with many respiratory and cardiac disorders.
The patient's limbs may remain in an unnatural position for a long time. This is associated with an increase in pressure on individual neurovascular bundles and can lead to damage to these structures and the occurrence of flaccid paralysis and paresis in the postoperative period.
Staying in one position for several hours in the absence of spontaneous breathing (since such surgical interventions are performed under inhalation anesthesia) can cause the development of pneumonia.
From Hippocrates to the Middle Ages
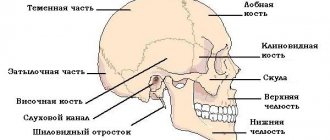
The procedure for craniotomy was also described by one of the most popular doctors of antiquity, Hippocrates . He advised the use of this type of operation (and this is described in detail in his works) to treat cranial injuries, as well as to get rid of epilepsy. In his work “On Head Wounds,” the ancient doctor described in great detail the structure of the skull and the types of injuries for which intervention was indicated.
Article on the topic
Wheel of history. What is Hippocrates famous for? Five centuries later, Galen used this Hippocratic base to perform the trephination procedure for hydrocephalus.
In the Middle Ages, aesculapians became skilled in matters of neurosurgery. For them, this method of treatment was an excellent option for relieving a person of constant headaches and cramps. At the same time, as notes preserved from those times note, the doctor had to be strong enough, because after cutting the skin, he needed to break the bones of the skull with tools like a chisel and a hammer. And it was necessary to act in such a way as not to damage the brain. After the operation, the hole in the head was not closed, but simply covered with skin.
Over time, instruments changed, and doctors began to use a special drill for trepanation. Researchers are also surprised by another fact - despite the fact that there was no anesthesia at that time, the percentage of surviving patients was quite high.
Possible complications
The operation is performed under general anesthesia; in some cases, part of the intervention takes place under local anesthesia, that is, the person remains conscious. After trephination, the patient is admitted to the intensive care unit or recovery room. When the patient comes to his senses without incident, he is transferred to the neurosurgery department, the duration of his stay there is about 2 weeks.
The consequences of trephination (anesthesia) may be thirst, headache, but this is not critical. But swollen facial tissues and bruises around the eyes may indicate the progression of cerebral edema. There are a number of other possible complications after this surgery.
- The occurrence of inflammatory processes in the wound, encephalitis, meningitis is a consequence of infections.
- Neurological disorders (convulsions, problems with coordination of movements, intellectual disorders) are associated with damage to the meninges and tissues.
- Deformation of the skull after removal of part of the bone, formation of a keloid scar.
Unpleasant consequences after craniotomy (headaches, dizziness, memory impairment) may be associated not so much with the operation itself, but with the brain disease for which the intervention was performed.
First scientific works
In 1518, the first practical manual on neurosurgery was published, authored by Berengario di Capri . Basically it describes how the author was able to cure, and quite successfully, a fracture of the occipital bone in Lorenzo de' Medici . At the same time, general recommendations are also included in the work.
The next person to contribute to the development of trephination and neurosurgery in general was the French surgeon and man considered the father of modern medicine, Ambroise Paré . In his works, he described in detail the instruments used and the technique used for trephination, removal of osteomyelic bone, drainage of hematomas and empyema, and also proposed a method for restoring depressed skull fractures.
Question answer
How to keep your brain healthy?
The development of neurosurgery was continued by the English physician Thomas Willis , who published “Cerebral Anatomy” in 1664.
It became for its time the most complete guide in such a complex matter. He was the first to propose the term “neurology,” understanding it as the science of neurons. At the same time, in parallel with science, the surgical skills of doctors also developed, on which a lot depends on the issue of neurosurgery. In the Middle Ages, options such as raspators, elevators and cutters were already actively used. The first cases of neuro-oncosurgery are described in works dating back to the 18th century.
Preparing for surgery
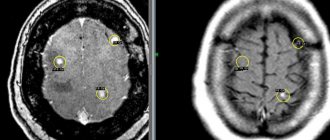
If penetration into the cranial cavity is necessary, good preparation of the patient for surgery is important. If there is enough time, the doctor prescribes a comprehensive examination, including not only laboratory tests, CT and MRI, but also consultations with specialists and examinations of internal organs. An examination by a therapist is required to decide whether the intervention is safe for the patient.
However, it happens that the opening of the skull is performed urgently, and then the surgeon has very little time, and the patient undergoes the necessary minimum of studies, including general and biochemical blood tests, a coagulogram, MRI and/or CT scan to determine the state of the brain and the localization of the pathological process. In the case of emergency trephination, the benefit in the form of preserving life is higher than the probable risks in the presence of concomitant diseases, and the surgeon decides to operate.
During a planned operation, after six o'clock in the evening the day before, it is forbidden to eat and drink, the patient once again talks with the surgeon and anesthesiologist, and takes a shower. It is advisable to rest and calm down, and in case of severe anxiety, sedatives may be prescribed.
Before the intervention, the hair on the head is carefully shaved, the surgical field is treated with antiseptic solutions, and the head is fixed in the desired position. The anesthesiologist puts the patient under anesthesia, and the surgeon begins the manipulations.
Opening the cranial cavity can be done in different ways, therefore the following types of trepanation are distinguished:
- Osteoplastic.
- Resection.
Regardless of the type of surgery planned, the patient must be placed under general anesthesia (usually nitrous oxide). In some cases, trepanation is performed under local anesthesia with a solution of novocaine. To enable artificial ventilation of the lungs, muscle relaxants are administered. The surgical area is carefully shaved and treated with antiseptic solutions.
Russian experience
Excavations and studies have shown that various operations on the skull were carried out already in the 10th–11th centuries in Kievan Rus. And Slavic doctors coped with the task no worse than the ancient Egyptians and Greeks.
In the 18th century, a technical revolution occurred in European countries, and industry began to produce more professional instruments necessary to perform such complex interventions. In Russia, they also established the production of instruments, after which neurosurgery rapidly stepped forward. Since 1738, all full-time doctors, including military personnel, had full-fledged surgical kits, which included instruments for craniotomy.
The first anatomical atlas was published in Russia in 1744. Its author was Martyn Shein . At that time, trepanation was already quite common and in demand - it was widely used for various traumatic brain injuries. Even in the examination papers of medical schools, questions about this procedure appeared. And they were often given paramount importance.
At the same time, trepanation was used exclusively as a forced method of treatment, i.e., only in cases where it was impossible to do without it. How the procedure took place can be found in the descriptions written by the doctors involved in the procedure. From one of these you can find out that a man’s “head was broken... the skull was pressed into the brain by two fingers... with great difficulty these fragments were taken out, here a cruel mother was found (dura mater) broken... the wounded man, being treated by the chief physician Martyn Shein, who from the brain itself, he scooped out up to 4 ounces of ounces (1 ounce is equal to 29.86 g), after 2 months and 8 days he recovered, the brain was filled, the cruel mother added in the broken hole.”
"Wild" medicine. How were primitive people treated in the Stone Age?
More details
Types of trepanations and indications for them
In modern medicine, craniotomy is also called craniotomy (but not brain trepanation). Another name does not change the fact that this is a very complex surgical procedure. The emergence of new methods of combating many brain diseases makes it possible to resort to it less often than before. However, two types of such operations on the skull still take place in neurosurgical practice - osteoplastic, resection trepanation.
Features of osteoplastic craniotomy
Trepanation is done when you need to gain access directly to the contents of the skull for surgical treatment:
- malformations of the skull and brain;
- tumors;
- intracerebral hematomas (for example, with hemorrhagic stroke);
- vascular aneurysm;
- abscesses;
- brain damage by parasites.
The operation begins with choosing a location for the burr hole: it should be as close as possible to the affected area. First of all, the surgeon cuts the soft tissue in a horseshoe shape so that the base of the flap is located in the lower part, since the blood vessels pass from bottom to top, and it is very important not to violate their integrity. Next, using special instruments, the periosteum and bone are dissected at an angle of 45°. Such a cutting angle is necessary so that the outer surface of the bone flap exceeds the inner one, and when restoring the integrity of the skull, the removed fragment does not fall inward. Having reached the meninges, the surgeon performs manipulations directly in the cranial cavity (removes the tumor, eliminates hemorrhage).
The craniotomy ends with suturing:
- the dura mater of the brain is sutured with absorbable threads;
- the flap is fixed with special threads or wire;
- the skin and muscles are sutured with catgut.
Carrying out resection trepanation
The pretexts for performing resection craniotomy are pathologies that provoke a rapid increase in intracranial pressure, which threatens life, or contribute to the displacement of brain structures, which is fraught with their infringement and death. These conditions include:
- cerebral hemorrhages;
- cerebral edema;
- injuries (bruises, hematomas, crushing tissue as a result of an impact);
- inoperable large tumors.
Trepanation in such cases is a palliative procedure, that is, it does not eliminate the disease, but only eliminates a dangerous complication.
Resection craniotomy of the skull is also called decompression craniotomy, since it is performed to reduce pressure inside the skull. Its peculiarity is that the bone fragment is not returned to its place. If the threat to life disappears over time, the hole can be closed with synthetic material.
The best place for surgery is the temporal area. Here, after removal of the bone flap, the membrane of the brain will be protected by the powerful temporalis muscle.
How is resection craniotomy performed? As with osteoplastic craniotomy, soft tissue and bone are cut. The bone fragment is removed so that the diameter of the hole is 5 - 10 cm. Having discovered swelling of the brain membrane, the surgeon is in no hurry to dissect it so that there is no displacement of the brain structures. To eliminate intracranial hypertension, you first need to make several punctures of the cerebrospinal fluid, and then cut the lining of the brain. When this manipulation is completed, the tissues (with the exception of the dura mater) are sutured.
Craniotomy of any kind can last several hours, and is used only for serious indications that threaten the patient's life. No one will perform such an operation, for example, in case of a mini-stroke - to eliminate its consequences, there are more gentle methods of therapy.
Contraindications to trepanation are terminal conditions (severe shock, extreme coma), septic processes.
Active development
The period of particularly active development of neurosurgery occurred in the second half of the 18th century. Giovanni Morgagni appeared , which linked nosology and a specific pathological substrate. She completely changed the philosophy of all European medicine and justified the removal of tumors in the skull. The first neuro-oncosurgical operations were performed on tumors that destroyed the cranial vault. The explanation for this choice was simple: such neoplasms were diagnosed quite easily. But at the same time, mortality rates during such interventions were quite high. So, for example, in Paris, over the course of 6 years, all the patients who underwent trepanation died.
Craniotomy.
Craniotomy is a stage of neurosurgical operation, the essence of which is to “cut out” a section of the bone of the cranial vault to form a trepanation window to access the brain. At the end of the operation, the bone fragment must be put in place and, if necessary, fixed.
This is not a separate type of operation and must be indicated in its full name. For example, “Craniotomy. Removal of acute subdural hematoma" or "Craniotomy. Removal of an intracerebral tumor of the left frontal lobe.”
The term consists of two Greek words: cranion (Greek, kranion - skull) and tomia (Greek, tome - cut). Literally means an incision or dissection of the skull.
Closer to the goal
Such a famous doctor as Nikolai Pirogov . Mention of such an important area of medicine can be found in the “Elements of General Military Field Surgery” under his authorship. In his work, the doctor presented an in-depth analysis of morphological changes and other mechanisms that accompany craniocerebral injuries. His work was based on the study of 20 trepanations he independently performed.
Article on the topic
Military field doctor. How did Nikolai Pirogov come up with anesthesia? Despite the fact that in the 19th century a fairly serious and detailed base was collected - both anatomical and technical, good experience was gained, all attempts at successful operations were broken by purulent complications. After all, the opening of the meninges was, in fact, an open wound through which bacteria easily penetrated. The situation changed when doctors began to use not only anesthesia, but also antiseptic drugs during operations.
The priority of separating neurosurgery into a separate field of medicine belongs to Russia. This was first stated in 1893 by Kazan University professor L. A. Malinovsky. It was he who, in his report, formulated the basic principles of neurosurgery and raised the question of special training for a surgeon operating on the central nervous system.
Today, this branch of medicine represents a precise and consistent intervention that helps to cope with the severe consequences of damage to the brain and spinal cord, as well as correcting the functioning of the nervous system. Modern tools and techniques allow doctors to literally work miracles. And doctors have been working towards this result for thousands of years.
Recovery after craniotomy
The first postoperative day is decisive for the patient. He is transferred to the intensive care ward, where vital processes are supported by special medical devices.
The medical staff vigilantly monitors the patient's awakening after anesthesia.
If necessary, the surgical wound is drained, ensuring the removal of excess fluid. The cleanliness of the drainage requires careful care, since infection can lead to meningitis.
Craniotomy is a serious operation and the stitches are removed after 7-10 days.
The length of stay in intensive care is at least a week and depends solely on the speed of the patient’s recovery abilities.
Drug treatment during the rehabilitation period is aimed at preventing the development of complications or the emergence of new pathologies.
- Painkillers are required. Patients are concerned about both real and phantom pain, including psychosomatic pain.
- Antibiotics help prevent inflammation.
- Antiemetics and anticonvulsants prevent the most common brain injury syndromes.
- Diuretics are used to prevent brain swelling.
The bandage is changed daily, and after two days the patient tries to get up. With a good recovery rate, after a few days the patient can move around independently quite confidently.
Recovery is not limited to the hospital. After returning home, the patient must also carefully follow all medical instructions. Strictly prohibited:
- lifting weights more than 3 kg;
- bends;
- smoking and alcohol;
- stress.
Even if there are no obvious errors in pronunciation, regular sessions with a speech therapist are recommended to eliminate speech disorders.
Daily short, accompanied walks and a balanced, low-salt diet are helpful.
If the emotional background of a patient prone to depression cannot be corrected, you need to consult a psychologist.