Radiation proctitis is an inflammation of the rectum that occurs during radiation therapy for tumors of the pelvic organs. This condition is accompanied by pain in the rectum and anus, painful urge to defecate, diarrhea, and discharge of mucus and blood from the rectum.
The likelihood of radiation damage to the intestinal wall and the development of proctitis is directly related to the total focal dose received during RT. The optimal tolerated total focal dose in the pelvic area is 40-50 Gy. In this case, the probability of developing complications is about 3-5%. When the SOD increases to 65 Gy, radiation proctitis develops in half of the patients.
- Causes of intestinal inflammation after radiation therapy
- Phases of radiation damage
- Classification of radiation proctitis
- Symptoms of radiation proctitis
- How is radiation proctitis diagnosed?
- How is radiation proctitis treated?
- Forecast and prevention of radiation proctitis
Causes of intestinal inflammation after radiation therapy
The following mechanisms underlie radiation damage to the intestine:
- Damage to the intestinal epithelium that develops under the influence of ionizing radiation. This leads to its focal necrosis, desquamation (peeling) and atrophy.
- Development of nonspecific inflammation of the mucous membrane and submucosa. The tissues are infiltrated by neutrophils, hyperemia, swelling, and bleeding are observed.
- Due to trophic disorders (arterioles are damaged), the blood supply to the affected areas of the intestinal mucosa deteriorates, which further aggravates ischemia and necrosis. As a result, atrophic changes progress with the development of fibrosis of the submucosal layer.
- Against this background, pathogenic flora begins to join, which causes infectious complications, including sepsis.
The end result of long-term trophic disorders of the intestinal wall and necrosis is the formation of strictures (narrowing of the lumen), the formation of fistulous tracts, the formation of telangiectasias and the development of bleeding from them.
Phases of radiation damage
Depending on the timing of appearance, early and late radiation damage are distinguished. Early ones make themselves felt directly during radiation therapy, or within 100 days from the date of its completion. This period (100 days, or three months) is the deadline for epithelial recovery from sublethal damage. At this stage, the etiological factor is damage to the intestinal epithelium with the development of inflammatory reactions. If the radiation dose is small, the epithelium is restored quite quickly, and, accordingly, the mucous membrane returns to normal. On average, this takes about 2-4 weeks from the last radiation session.
Late radiation injuries develop 100 days after the end of radiation therapy. During this period, vascular disorders due to damage to the endothelium come first. Its cells become necrotic, and in order to restore them, the remaining endothelial cells begin to actively proliferate. This leads to obliteration of the lumen of blood vessels, the development of thrombosis, ischemia and trophic disorders. As a result, radiation vasculitis develops with bleeding, atrophic processes, fibrous changes, and the proliferation of scar tissue.
Radiation caries: clinical picture, treatment issues
Dmitrieva E.F. , dentist, TalismanDent M LLC, Chelyabinsk Nurieva N.S. , Doctor of Medical Sciences, Associate Professor of the Department of Orthopedic Dentistry of South Ural State Medical University
Worldwide, head and neck cancer accounts for about 10% of all malignancies [1]. Treatment of malignant neoplasms of the head and neck requires a multidisciplinary approach, the collaboration of doctors of various specialties: oncologist surgeon, radiologist, chemotherapist, radiologist, endoscopist, dentist, pathologist, cytologist, as well as doctors of some other specialties, each of whom is involved in making a diagnosis, assessing the degree of tumor spread, development of treatment tactics and its implementation [2]. The choice of strategy and treatment is mainly made between surgical treatment, radiation therapy and combined methods.
Radiation therapy is a treatment method using ionizing radiation. Among various treatment methods in clinical oncology, radiation therapy occupies one of the leading places. According to WHO, 70-75% of cancer patients require radiation therapy. Radiation can be radical, palliative, or used in combination with surgery. The advantages of radiation therapy include its good tolerability and the possibility of achieving a permanent cure in the early stages of some tumors while preserving the function of the affected organ. The use of radiation treatment as palliative, independent therapy in inoperable cases is the most effective among other treatment measures.
In independent radiation therapy of the head and neck organs, a selected rhythm of daily irradiation of 2 g (5 times a week; 10 g per week) is widely used to obtain a radical or palliative effect. The total focal dose in this case (with an average radiosensitivity of the tumor) is 60-70 g. Radiation therapy is carried out according to a split program: the first course - up to a total focal dose of 30 g, followed by a break in treatment for 2-3 weeks. The second course is also carried out with a single focal dose of 2 g up to a total focal dose of 40 g (total total dose – 70 g) [3].
However, the problem remains the rather high frequency of severe post-therapeutic complications, which significantly reduce the possibilities of the treatment method. A common complication of radiation therapy is radiation damage to teeth (Fig. 1).
Fig.1. Radiation necrosis of teeth after a course of radiation therapy (54 g)
One of the promising directions in this regard is the use of modern technical advances that make it possible to reduce the volume of undesirably irradiated normal tissues with a concentration of the maximum radiation dose at the tumor level and, on this basis, improve the results of treatment of this group of patients [4].
In order to increase the effectiveness of radiation therapy, the use of hyperfractionated irradiation regimens is justified. According to some domestic and foreign researchers, an increase in a single focal dose to 2.4-3 g, provided that the latter is administered in 2-3 fractions per day with an interval between fractions of at least 4 hours, is accompanied by an increase in the effectiveness of treatment of nasopharyngeal cancer by 20-30% [ 5,6]. In a study performed by S. L. Wolden et al., who conducted a comparative analysis of the results of irradiation in the usual dose fractionation regimen (1.8 g / 5 times a week / 70 g) and dynamic fractionation, when during the 5th and 6th weeks irradiation is performed using accelerated fractionation with a single dose of 1.6 g 2 times a day in combination with cisplatin chemotherapy. A statistically significant increase in the frequency of complete tumor resorption, relapse-free and overall survival was noted [14]. According to the results of studies by a number of authors, early radiation damage to the mucous membrane occurred much more often with hyperfractionation. However, the number of late radiation injuries was the same [7].
Equally important is the quality of radiation therapy. The use of special devices (headrests, masks made of hot-melt plastics) that fix a certain position of the patient during irradiation, individual dosimetric planning based on X-ray computed tomography and the formation of dynamically changing shaped irradiation fields using a multi-lift collimator help to increase the effectiveness of radiation therapy. In comparison with a standard radiation therapy program, the use of a conformal irradiation technique based on three-plane planning makes it possible to create an optimal ratio between the radiation dose delivered to the tumor and in the surrounding tissues [8].
Radiation damage to hard dental tissues with prolonged exposure to the body in small doses depends on the total dose, radiation exposure, radiation intensity and time factor. Changes in tooth tissues manifest themselves in the form of chalky spots, pigmentation, softening and necrosis of enamel and dentin (Fig. 2).
Fig.2. Radiation caries after a split course of radiation therapy
Large doses of radiation can lead to necrosis of large areas of enamel and dentin in the immune zones of teeth. Changes in the pulp manifest themselves in the form of hyalinization of the walls of blood vessels, vacuolar and fatty degeneration, atrophy and degeneration of odontoblasts, etc. The complex of pathomorphological changes in dental tissues with these lesions is in many ways reminiscent of dental caries, which gave rise to the introduction of the term radiation caries.
Radiation dental caries - (c. dentis radialis) generalized dental caries, developing as a complication of X-ray or radiotherapy of the maxillofacial area; occurs with pigmentation and softening of the surface layers and the formation of deep cervical cavities.
To date, no consensus has been developed regarding the mechanism and nature of changes in the tissues of the tooth and oral cavity due to radiation.
Ivanova L.A. believes that the breakdown of protein molecules, metabolic disorders, circulatory disorders, and hypoxia, which occur under the influence of ionizing radiation, collectively contribute to the development of unfavorable conditions for the existence of the pulp, and the longer they take place, the more severe the consequences can be for both the pulp and the hard dental tissues [9]. According to Barer G.M., Ivanchikova L.A., changes in hard tissues are based on damage to the protein matrix and disruption of the chemical bond between the mineral and protein fractions. Already during the irradiation process, the authors observed demineralization and destructive changes in the dentin and cementum of the teeth of experimental animals, which can be explained by the peculiarities of the histological structure of hard tissues, extremely low metabolism in them, and the inability of tissues to recover [10].
According to Okado Sh., 1979, the further development of changes in dentin that occurred during irradiation, characterized by ongoing demineralization, an increase in foci of destruction, destruction of the enamel-dentin junction, and the appearance of lacunar resorption of dentin at the border with the pulp is explained by both the reaction of the consequences and the influence of the damaged pulp, recovery of which after irradiation is incomplete. In the destruction of the enamel-dentin junction, the difference in the intensity of demineralization of enamel and dentin is important. The mineral saturation of dentin decreases to a much greater extent than enamel, which leads to disintegration of these tissues.
Ivanova L.A., Borovsky E.V., Segen I.T. and Nazarov G.I. indicate that the pathological process occurs simultaneously in many teeth, spreads around the necks and along the surfaces of the crowns, ending, as a rule, with a tooth fracture at the level of the gingival margin. The authors draw attention to the ineffectiveness of filling due to the appearance of new defects around the fillings, as well as in previously undamaged areas [9, 11, 12].
Changes in the oral mucosa, as indicated by Shchelkanogova M.G. et al., 1993, poor hygiene in combination leads to impaired self-cleaning of teeth; a critical situation is created on the enamel surface (pH 4-5 under plaque), which favors the demineralization of irradiated enamel. The sensitivity of teeth to changes in temperature, to pressure, to sweet and sour foods increases, the color changes (to light or dark gray), the enamel loses its shine and becomes brittle and fragile; the teeth are covered with a thick sticky plaque that is difficult to remove. Cariogenic microflora appears. Caries also occurs in relatively rarely affected areas (in the area of the tubercles, in the cutting areas). The most common type is cervical caries of the anterior teeth. The process is painless, progresses quickly and ends with the breaking off of the crowns.
The principles of prevention and treatment are reflected in the Dental Disease Section/International Society of Oral Oncology (ISOO) protocol (2010):
1. Use of fluoride-containing drugs. Remineralization therapy significantly reduces the risk of developing pathology of hard dental tissues (Level of Evidence: II, Grade of Recommendation: B), (Fig. 3).
Fig.3. Mouth guards for remineralizing therapy
2. Use of mouth rinses with chlorhexidine. The use of these drugs improves oral hygiene and also helps reduce the number of Streptococcus mutans. When prescribing chlorhexidine-containing rinses, it is necessary to take into account the possibility of such side effects as staining of tartar and changes in taste sensitivity (Level of Evidence: II, Grade of Recommendation: B).
3. Restoration of defects in hard dental tissues. To restore defects in hard dental tissues, it is recommended to use composite materials, hybrid glass ionomer cements and amalgam. The use of traditional GICs is less preferable (Level of Evidence: II, Grade of Recommendation: B) [13].
If the hard tissues of the tooth crown are damaged, treatment is carried out in several stages. First, necrotic masses are carefully removed from dental defects manually with an excavator so as not to penetrate into the tooth cavity, and then a calcifying paste is introduced, consisting of equal parts of calcium glycerophosphate powder, zinc oxide and glycerin. The paste is applied in a thin layer to the bottom and walls of the resulting cavity and covered with temporary filling material.
The next stage of delayed dental treatment is carried out after 1-1.5 months. It consists of removing non-viable, necrotic tooth tissue with a bur to a mineralized area of dentin or enamel, after which a calcifying paste is applied again and the teeth are filled with glass ionomer cements.
For deeper lesions, existing necrotic defects are eliminated with glass ionomer cements and after 3-4 months, if required by cosmetic restoration of the anterior teeth, part of the glass ionomer is removed and a composite filling material is applied on top.
Thus, radiation caries is a common complication of radiation therapy for oropharyngeal cancer. Today, opinions differ about the clinical picture, features of the course of the disease and treatment tactics. We have not found any data in the literature on the relationship between fractionation modes and radiation damage to teeth in the early and late stages, as well as on the effect of conformal irradiation on hard dental tissues. We plan to study the problem in more detail.
References: 1. Cherenkov V.G. Clinical oncology: textbook. manual for the postgraduate system. education of doctors / V.G. Cherenkov. – Ed. 3rd, rev. and additional – M.: MK, 2010. – 434 p. 2. Kropotov M.A. General principles of treatment of patients with primary head and neck cancer / M.A. Kropotov // Practical Oncology. – 2003. – T.4, No. 1. – P.1-7. 3. Oncology: textbook for universities / Velsher L.Z., Matyakin E.G., Duditskaya T.K., Polyakov B.I. – 2009. – 512 p. 4. Alieva S.B. Chemoradiation therapy for patients with locally advanced squamous cell cancer of the head and neck / S.B. Alieva // Practical Oncology. – 2008. – T.9, No. 1. – P.27-30. 5. Aliev B.M., Garin A.M., Koshaliev E.Sh. Comparative assessment of the effectiveness of radiation and chemoradiation treatment of locally advanced nasopharyngeal cancer in stages III-IV of the disease. Med. radiol. – 1987. – No. 7. – P. 25-30. 6. Aliev B.M., Garin A.M., Chuprik-Malinovskaya T.P. Nasopharyngeal cancer: experience with radiation and chemoradiotherapy // Vestn. OSC RAMS. – 1995. – No. 1. – P. 26-32. 7. Kanaev S.V. Radiation therapy for malignant tumors of the head and neck / S.V. Kanaev // Practical Oncology. – 2003. – T.4, No. 1. – pp. 15-24. 8. Chuprik-Malinovskaya T.P. Nasopharyngeal cancer: issues of diagnosis and treatment // Practical Oncology. – 2003. – T.4, No. 1. – pp. 38-44. 9. Ivanova L.A. Prevention of post-radiation lesions of teeth.//Methodological recommendations. – Perm, 1987. 10. Barer G.M. Changes in the ultrastructure of hard dental tissues after local irradiation // G. M. Barer, L. A. Ivanchikova; G. I. Nazarov // Dentistry. 1977. – No. 1. – P. 4-7. 11. Borovsky E.V., Sazonov N.I. Changes in the permeability of tooth enamel after remote gamma irradiation of the lower jaw // Dentistry. – 1978. – P.1-5. 12. Nazarov G.I. Changes in teeth and jaws after local gamma irradiation // Med. radiology. – 1975. – No. 8. – P.75-76. 13. Borovsky E.V. Restoration of radiation dental caries. Clinical example/E.V. Borovsky, I.M. Makeeva, E.A. Skatova // Pediatric dentistry and prevention: peer-reviewed scientific journal recommended by the Higher Attestation Commission. – 2012. – T. XI, No. 2. – P.11-19. 14. Wolden SL, Zelefsky MJ, Kraus DH et al. Accelerated concomitant boost radiotherapy and chemotherapy for advanced nasopharyngeal carcinoma // J. Clin. Oncol. – 2001/ – Vol. 19(4). – P. 1105-1110.
Article provided by the journal "Problems of Dentistry"
Classification of radiation proctitis
Depending on the severity, the following types of radiation proctitis are distinguished:
- Catarrhal proctitis. During the examination, a hyperemic, loose, edematous intestinal wall is discovered. There may be increased mucus production. This form of proctitis is considered mild.
- Erosive-desquamative proctitis. This form is manifested by foci of destruction of the epithelium with the formation of erosion - a tissue defect within the epithelial layer.
- Ulcerative proctitis - destruction spreads to deeper layers of tissue and involves the mucous membrane and submucosa in the process.
- Fistulous proctitis. A through perforation of the intestinal wall is formed with access to the pelvic cavity or with the involvement of nearby organs, for example, the bladder or vagina.
There is a classification of radiation proctitis based on the rectoscopic picture:
- There is local redness and friability of the intestinal mucosa, telangiectasias and dilated blood vessels are noted).
- Against the background of hyperemia and edematous intestinal mucosa, ulcers covered with a gray scab are found.
- Against the background of inflammatory lesions, strictures of the intestinal wall are detected.
- Against the background of ulcerative lesions, strictures and fistulas or intestinal perforation are detected.
Symptoms of radiation proctitis
Symptoms of acute radiation proctitis develop within 1-2 weeks after the start of radiation. It can be:
- Diarrhea.
- Pain in the rectal area or lower abdomen.
- Painful urge to defecate.
- Discharge of mucus from the anal canal or its admixture in the stool.
- Anal incontinence.
- Bleeding. In some patients, bleeding is profuse and leads to acute hemorrhagic anemia, which requires blood transfusion.
If there are no symptoms of acute radiation proctitis, this does not mean that long-term consequences will not occur. The frequency of late post-radiation proctitis is about 10% of the total number of cases. There is a latent period that lasts several months or even years. The clinical picture is characterized by the following symptoms:
- Pain in the right iliac region or rectum.
- Frequent stools, tenesmus.
- Presence of blood in the stool.
- When strictures form, constipation and partial intestinal obstruction may occur.
- When fistulas are forced, pathological cloudy vaginal discharge, pneumaturia (air in the urine), loose stools with impurities of undigested food are noted.
Depending on the severity of the disease, there are several degrees of the disease:
1st degree - mild proctitis. Accompanied by mild diarrhea, less than 5 times a day, there may be a discharge of small amounts of mucus and blood.
2nd degree - proctitis with a controlled course. Moderate diarrhea, more than 5 times a day. A large amount of mucus is released and there is bleeding.
3rd degree - proctitis with severe course. There are strictures and bleeding from the rectum requiring surgical intervention.
Grade 4 is a life-threatening course that requires immediate intervention. It is accompanied by intestinal obstruction, fistulas, and heavy bleeding.
Methods for treating uterine cancer through radiotherapy
Adenocarcinoma, neuroendocrine, small cell or squamous cell carcinoma is treated in several ways with radiation therapy. The malignant area is either exposed to external radiation therapy, or a radioactive source is placed in close proximity to the tumor.
In some cases, the disease requires the use of two methods of radiation therapy at once. Surgical and radiation methods are often combined. The decision on the optimal treatment method is preceded by a comprehensive diagnosis. The patient undergoes all the necessary tests to determine the form and stage of the formation.
External beam therapy
The intervention should be carried out in an outpatient setting. An oncological tumor on the cervix is exposed using a special device. Markers are applied to the patient's skin to direct the beams precisely to the target. The session lasts several minutes, during which no painful sensations occur. The course of radiation therapy can last 5-6 weeks. Procedures are prescribed 5 times a week. On Saturday and Sunday the patient rests.
Internal radiation therapy
Internal radiation therapy is often combined with external radiation or surgery. During the latter, a special applicator with tubes is installed in the uterus, which produce radiation into the area of pathological cells through a special lumen. Irradiation can be:
- high dose;
- low dose;
- impulsive.
The most popular is high-dose radiation, which can be carried out both in a hospital setting and in an outpatient clinic. Using the method, exophytic and endophytic types of cancer are successfully treated. The required high dose of radiation is received in several sessions lasting 2-3 days. The number of procedures is determined according to the condition of the cervix at the time of treatment. The applicators installed on the patient are either removed after each session or remain at the intervention site for the entire treatment period.
Low-dose radiation is a fairly lengthy procedure. A session can last from 12 hours to several days. The patient must remain in a supine position throughout the irradiation. Visits to relatives are strictly limited. If with low-dose exposure irradiation occurs continuously, then with pulsed exposure it occurs intermittently. The session is similar in duration and has restrictions to prevent exposure of other people and to prevent movement of the installed applicators.
How is radiation proctitis diagnosed?
Diagnosing diseases is not difficult. The key point here is the presence of a history of radiation therapy and its effect on the pelvic organs, increased frequency of stool, and the presence of pathological impurities in it.
If the course is prolonged, it is recommended to examine the rectum using a rectoscope or endoscope. This will allow you to detect multiple erosions, scar deformation, atrophic changes and telangiectasias and decide on the need for endoscopic or surgical treatment.
How is radiation proctitis treated?
If symptoms of radiation proctitis develop during radiation therapy, a revision of the radiation regimen is required. For mild damage, it is enough to increase the intervals between sessions. In more severe cases, the question arises of reducing the total focal dose or even canceling radiation therapy. In addition, treatment is required, which includes several areas:
- Diet food. An important part of the treatment of post-radiation proctitis is dietary nutrition. Food should contain an increased amount of protein, a sufficient amount of macro and micronutrients. It should also be chemically and physically gentle, i.e. you should avoid spicy, pickled, and canned foods. In addition, coarse plant fiber should be avoided so that it does not injure the already damaged intestinal wall.
- Conservative methods include drug therapy, therapeutic enemas, suppositories, etc. As part of independent treatment, it is used only for mild and moderate pathology; in other cases, it is used as part of complex treatment together with other treatment methods.
- Endoscopic methods - radiofrequency ablation, argon plasma coagulation, etc. Currently, these methods are the gold standard for the treatment of chronic forms of the disease and are mainly used to eliminate bleeding.
- Surgical methods include removal of the rectum with a stoma or coloanal anastomosis. They are used in severe cases when there is a threat to the patient's life. Surgical operations are used to eliminate strictures, fistulas and perforations of the intestinal wall.
Drug therapy for radiation proctitis
The following groups of drugs are used for drug therapy:
- Glucocorticosteroids are the main group of drugs used for moderate and severe proctitis. GCS have a powerful anti-inflammatory effect.
- Analgesics. Different groups of drugs are used, including narcotic drugs.
- 5-aminosalicylic acid (mesalazine) - has an anti-inflammatory and protective effect, thereby protecting the affected mucosa and stimulating its recovery.
- Antidiarrheal drugs. Enveloping and astringent agents and antispasmodics are used.
- Antibacterial drugs. They are prescribed for the treatment or prevention of bacterial complications of proctitis.
Given that the rectum is the terminal part of the digestive tract, many topical drugs are not effective enough when used in forms intended for oral administration. Therefore, preference is given to forms for local use - suppositories, enemas, powders, etc. They act directly on the intestinal wall and have an effect in the shortest possible time.
Surgical treatment of radiation proctitis and radiation injuries of the rectum
Surgical treatment is aimed at eliminating specific symptoms or complications of post-radiation proctitis. This may include continuous bleeding, fistulas and perforations of the intestinal wall, or strictures. Very rarely, surgery is used to relieve uncontrollable pain.
Before planning an operation, it is important to take into account that radiation damage reduces the regenerative capabilities of the tissue, so there is a high risk of complications, including bleeding, poor wound healing, infection and its generalization, as well as long-term negative effects such as severe scarring or anal sphincter failure.
Thus, classical surgical interventions in the acute period are risky, they do not allow complete control of bleeding and can lead to severe, life-threatening complications. Therefore, they are mainly used to eliminate the long-term consequences of radiation proctitis.
Endoscopic treatment methods
Endoscopic treatment methods are safer. They are based on the destruction of the affected part of the intestinal mucosa, followed by necrosis and replacement by healthy epithelium. For this purpose, radiofrequency ablation is used in particular. The method is based on local controlled heating of tissue to produce a thermal burn. The energy source here is radio frequency waves.
During the procedure, a special catheter is inserted into the patient's rectum, which will emit waves and heat the tissue. The standard depth of necrosis is several tenths of a millimeter, so 1-3 pulses are needed to treat one area of the mucosa. The energy intensity is adjusted automatically based on the current temperature of the tissue being treated. This allows you to avoid “overheating” and deep burns.
The advantage of endoscopic treatment is its bloodlessness, a high degree of control during the intervention, and quick results. It is most effective for bleeding. With just one procedure, you can coagulate all pathological blood vessels and stop even heavy bleeding. As a rule, for maximum results, the procedure is carried out 2-3 times at intervals of several months.
Radiation necrosis
The article was prepared by a specialist for informational purposes only. We urge you not to self-medicate. When the first symptoms appear, consult a doctor.
The use of ionizing radiation in the treatment of tumors, diseases of the blood, skeleton and various organs and systems is associated with the risk of complications. Often, people whose profession is related to radiation devices become victims of the negative effects of high-voltage radiation. The timing of the development of necrotic foci in tissues after irradiation depends on the dose, the volume of the irradiated area, etc.
Penetrating radiation can cause severe types of tissue necrosis. So far, the mechanism and nature of pathological changes from radiation have not been fully studied. It is known that the causes of radiation necrosis are vascular, morphological and degenerative disorders. The immunosuppressive effect of ionizing radiation on tissue is also possible.
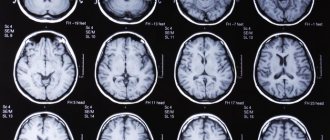
Irradiation of the body helps to suppress enzyme systems containing iron and tissues involved in the respiratory process in the aerobic phase. This entails the formation of under-oxidized metabolic products in the tissues. Radiation therapy can damage the nervous system and produce free radicals. Histological examination, as a rule, reveals demineralization of nerve fibers, compaction of the tissue of small arteries and necrosis of brain tissue.
The nerves of the brachial and lumbosacral plexus are susceptible to the development of radiation necrosis simultaneously with radiation necrosis of the Central nervous system. Radiation sickness is a consequence of the effect of X-ray gamma rays and neutron fluxes on the entire body. As a rule, the course of the disease is accompanied by necrosis. Regeneration in irradiated tissues is suppressed, the mucous membrane of the mouth and lips swells, and pinpoint bleeding may occur.
At the height of the disease, the general condition worsens, the trophism of the oral mucosa changes, a burning sensation, anemia, and dryness are observed. Radiation stomatitis occurs. The phenomena of hemorrhagic syndrome and the presence of infection (putrefactive) provoke the formation of ulcers and necrosis. Necrosis develops in the oral cavity, and is always most pronounced in the area adjacent to the mucous membrane of metal dentures and fillings; in such places more bacteria are usually present. Signs of damage to the edges of the gums and tonsils appear, followed by damage to the lateral surfaces of the tongue and palate, severe swelling of the lining of the mouth, lips and face.
After the edge of the gums becomes necrotic, they become loose and bleeding. Softening of the bone tissue of the alveolar process causes loosening and loss of teeth. Methods of therapeutic measures depend on the condition of various organs and systems. Without treatment, radiation necrosis has large lesions, but under the influence of glucocorticoids, the degree of active development decreases.
The best treatment for progressive radiation necrosis is surgery. Before any radiation exposure, it is necessary to take drugs that slow down radiochemical reactions. The risk of negative consequences from radiation therapy is reduced when using hormonal, antihistamine, and antibacterial agents.
To restore the functioning of the circulatory system and prevent hemorrhagic diathesis causing the development of necrosis, rutin, vikasol, calcium gluconate and a multivitamin complex are prescribed. If we consider irradiation of the hypothalamus and pituitary gland, then after this process disruptions occur in the endocrine system. A few months after radiation exposure, tooth enamel becomes dull, loses its shine, dark-colored areas of necrosis appear, and a loose necrotic mass forms.
Gradually, areas of necrosis cover a significant part of the tooth, cavities with uneven, corroded edges appear, and fillings fall out. Progressive radiation necrosis affecting the hard tissues of the tooth is treated in several stages by removing decomposed tissue and filling the bottom and walls of the cavity with calcifying paste. Before starting radiation therapy, to reduce the direct effect of radiation on the teeth, you need to wear a lead mouth guard, conduct a course of remineralization therapy and take antioxidants.
All these methods will maximally protect the body from negative consequences or reduce the degree of possible effects. Irradiation of intracranial tumors, neoplasms on the head and neck is unfavorable for the body. Subsequently, brain necrosis may occur. Such complications develop quickly or over several months and years. The mechanism that triggers the development of late necrosis of the central nervous system is considered to be damage to the vascular network of the brain.
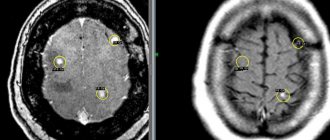
To determine the likelihood of developing radiation necrosis of the brain, the dose and duration of irradiation are taken into account. Clinical manifestations of this type of pathology are very diverse; they can be contributed to by different causes and conditions. If necrosis develops, excision of the affected tissue may be helpful.
Author of the article:
Mochalov Pavel Alexandrovich |
Doctor of Medical Sciences therapist Education: Moscow Medical Institute named after. I. M. Sechenov, specialty - “General Medicine” in 1991, in 1993 “Occupational diseases”, in 1996 “Therapy”. Our authors