Our “Neurosciences for Everyone” section already has two subsections. The first is large articles devoted to general issues: how the nervous system appears, how it works, and so on. The second is articles devoted to tools and methods of neuroscience. MRI, , TMS and other scary abbreviations. However, this set is definitely missing one more, thickest deck of cards: the cellular anatomical one. After all, the nervous system consists of a large number of cell types, and the brain has many different parts, which are constantly mentioned in our news and articles. Therefore, we are starting the third series of articles, which we tentatively called “Details”. And the first article in this series will be devoted to one of the most famous types of cells in the cerebellum (a structure about which an article is yet to come): Purkinje cells.
Purkinje cells (red). Photo by Yinghua Ma and Timothy Vartanian, Cornell University, Ithaca, NY Part of the exhibit Life:Magnified by ASCB and NIGM
Structure
Cross section of the cerebellum folium.
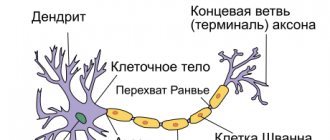
(Purkinje cell labeled in top center.) Silver stain of the cerebellum showing Purkinje cells. Purkinje cells. Belshovsky stain. Image of cerebellar Purkinje cells expressing tdTomato on a confocal microscope. These cells are among the largest neurons in the human brain (Betz cells are the largest),[3] with an intricately designed dendritic arbor, characterized by a large number of dendritic spines. Purkinje cells are found within the Purkinje layer of the cerebellum. Purkinje cells are aligned like dominoes stacked in front of each other. Their large dendritic branches form almost two-dimensional layers through which parallel fibers from deeper layers pass. These parallel fibers make relatively weaker excitatory (glutamatergic) synapses to spines in the Purkinje cell dendrite, whereas climbing fibers originating from the inferior olivary nucleus in the medulla provide very powerful excitatory effects on the proximal dendrites and cell somas. In parallel, fibers pass orthogonally through the dendritic branch of the Purkinje neuron, numbering up to 200,000 parallel fibers[4], forming a granule-cell-Purkinje cell synapse with one Purkinje cell. Each Purkinje cell receives approximately 500 climbing fiber synapses, all of which originate from a single climbing fiber.[5] Both basket and stellate cells (found in the cerebellum). molecular layer) provide inhibitory (GABAergic) input to the Purkinje cell, with basket cells synapsing with the axon initial segment of the Purkinje cell, and stellate cells with dendrites.
Purkinje cells send inhibitory projections to the deep cerebellar nuclei and represent the only output of motor coordination in the cerebellar cortex.
Molecular
The Purkinje layer of the cerebellum, which contains the cell bodies of Purkinje and Bergmann glia, express a large number of unique genes.[6] Purkinje gene markers have also been proposed by comparing the transcriptome of Purkinje-deficient mice with the transcriptome of wild-type mice.[7] One illustrative example is Purkinje cell protein 4 (PCP4) knockout mice, which exhibit impaired locomotor learning and markedly altered synaptic plasticity in Purkinje neurons.[8][9] PCP4 accelerates both the association and dissociation of calcium (Ca2+) with calmodulin (CaM) in the cytoplasm of Purkinje cells, and its absence impairs the physiology of these neurons.[8][9][10][11]
Development
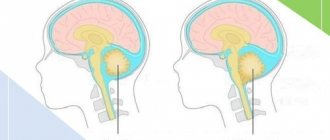
Mammalian embryonic studies have detailed the neurogenic origin of Purkinje cells. [12]. Early in development, Purkinje cells arise in the ventricular zone of the neural tube, which is the precursor to the nervous system in the embryo. All cerebellar neurons are derived from the germinal neuroepithelium of the ventricular zone. [13]. Purkinje cells are specifically formed from precursors in the ventricular neuroepithelium of the embryonic cerebellar rudiment. [14]. The first cells to emerge from the cerebellar primordium form a cap over a diamond-shaped cavity in the developing brain called the fourth ventricle, forming the two hemispheres of the cerebellum. Purkinje cells, which develop later, belong to the central part of the cerebellum called the vermis. They develop in the cerebellar primordium, which covers the fourth ventricle and below a fissure-like area called the isthmus of the developing brain. Purkinje cells migrate to the outer surface of the cerebellar cortex and form a layer of Purkinje cells.
Purkinje cells are born during the earliest stages of cerebellar neurogenesis. Neurogenin-2 together with neurogenin-1 are transiently expressed in restricted domains of the ventricular neuroepithelium during the time window of Purkinje cell genesis. [15]. This spatiotemporal distribution pattern suggests that neurogenins are involved in the specification of phenotypically heterogeneous subsets of Purkinje cells ultimately responsible for scaffolding the cerebellar topography.
There is evidence in mice and humans that bone marrow cells either fuse or generate cerebellar Purkinje cells, and it is possible that bone marrow cells, either by direct formation or by cell fusion, may play a role in repairing damage to the central nervous system. [16][17][18][19][20] Further evidence points to the possibility of a common stem cell ancestor among Purkinje neurons, B lymphocytes, and aldosterone-producing cells of the human adrenal cortex.[19]
What are they needed for
The role of Purkinje cells in how we move cannot be overstated. They receive excitatory impulses from the liana-shaped fiber and mossy fibers of the cerebellum and send inhibitory impulses (we remember that GABA is the main “brake” of the brain) to the deep layers of the cerebellum - its nucleus. If we translate this activity into simple language, then Purkinje cells play a critical role in motor learning, balance and coordination of movements. It is easy to verify this by knowing two facts: firstly, in humans, Purkinje cells mature relatively late, by the age of eight, and secondly, they are very sensitive to the effects of alcohol. And that is why children and drunks move so awkwardly. By the way, the most developed Purkinje cells are found in people who have been involved in complexly coordinated movements since childhood: acrobatics, gymnastics, figure skating or dancing.
Single Purkinje cell
Text: Alexey Paevsky
Read materials from our website on Facebook , VKontakte , Yandex-Zen and the Telegram channel , and also follow the new pictures of the day on Instagram .
Function
Purkinje cell protein 4 (PCP4) is markedly immunoreactive in human cerebellar Purkinje cells.
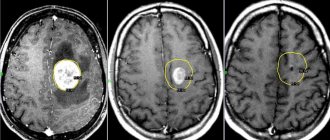
Top to bottom 40X, 100X and 200X microscopic magnifications. Immunohistochemistry was performed based on published methods.[8] Microcircuit of the cerebellum. Excitatory synapses are designated (+) and inhibitory synapses are designated (-). MF: Mossy fiber. DCN: Deep cerebellar nuclei. IO: Inferior Olive. CF: Climbing fiber. GC: Granular cell. PF: Parallel fiber. PC: Purkinje cell. GgC: Golgi cell. SC: Stellate cell. BC: Basket cell. Purkinje cells exhibit two distinct forms of electrophysiological activity:
- Simple spines
occur at a frequency of 17–150 Hz (Raman and Bean, 1999) either spontaneously or when Purkinje cells are activated by synaptically parallel fibers, the axons of granule cells. - Complex spikes
are slow bursts with a frequency of 1–3 Hz, characterized by an initial long burst of large amplitude followed by a high-frequency burst of action potentials of smaller amplitude. They are caused by activation of climbing fibers and may involve the generation of calcium-mediated action potentials in dendrites. After complex bursts, simple bursts can be suppressed by a powerful complex input pulse.[21]
Purkinje cells exhibit spontaneous electrophysiological activity in the form of sodium- and calcium-dependent spike trains. This was originally shown by Rodolfo Llinas (Llinas and Hess (1977) and Llinas and Sugimori (1980)). P-type calcium channels were named after the Purkinje cells where they were first discovered (Llinas et al. 1989), which are critical for cerebellar function. We now know that activation of a Purkinje cell by fiber climbing can switch its activity from a quiescent state to a spontaneously active state and vice versa, serving as a kind of switch.[22] These results were contradicted by research suggesting that such switching by fiber climbing occurs predominantly in anesthetized animals and that Purkinje cells in awake animals tend to operate almost continuously in the upstate.[23] But this latest study has itself been called into question.[24] Since then, switching of Purkinje cells has been observed in awake cats.[25] A computational model of the Purkinje cell showed that intracellular calcium calculations are responsible for the switch.[26]
The results showed that Purkinje cell dendrites release endocannabinoids that can temporarily inhibit both excitatory and inhibitory synapses.[27] The intrinsic activity pattern of Purkinje cells is set and controlled by the sodium-potassium pump.[28] This suggests that the pump may not simply be a homeostatic pump, a housekeeping molecule for ion gradients. Instead, it could be a computational element in the cerebellum and cerebrum.[29] Indeed, a mutation in the Na+-K+ pump causes rapid onset of parkinsonian dystonia; its symptoms indicate that it is a cerebellar pathology.[30] Additionally, using the poison ouabain to block Na+-K+ pumps in the cerebellum of living mice causes ataxia and dystonia.[31] Numerical modeling of experimental data suggests that in vivo the Na+-K+ pump produces long stationary points (>> 1 s) to fire the Purkinje neuron; they may have a computational role.[32]Alcohol suppresses Na+-K+ pumping in the cerebellum, which is likely why it disrupts cerebellar computation and body coordination.[33][34]
Clinical significance
In humans, Purkinje cells can be damaged for a variety of reasons: from toxic exposure, such as alcohol or lithium; autoimmune diseases; genetic mutations causing spinocerebellar ataxia, gluten ataxia, Unverricht-Lundborg disease, or autism; and neurodegenerative diseases that are not known to have a genetic basis, such as multiple system atrophy of the cerebellar type or sporadic ataxias.[35][36]
Gluten ataxia is an autoimmune disease caused by ingestion of gluten.[37] Purkinje cell death due to gluten exposure is irreversible. Early diagnosis and treatment with a gluten-free diet can improve ataxia and prevent its progression.[35][38] Less than 10% of people with gluten ataxia have any gastrointestinal symptoms, but about 40% have intestinal involvement.[38] It accounts for 40% of ataxias of unknown origin and 15% of all ataxias.[38]
The neurodegenerative disease spinocerebellar ataxia type 1 (SCA1) is caused by unstable polyglutamine expansion within the Ataxin 1 protein. This defect in the ataxin 1 protein causes disruption of mitochondria in Purkinje cells, leading to premature degeneration of Purkinje cells.[39] As a consequence, motor coordination decreases and death eventually occurs.
Some pets can develop a condition in which Purkinje cells begin to atrophy shortly after birth, called cerebellar abiotrophy. This can result in symptoms such as: ataxia, intention tremor, hyperresponsiveness, lack of reflex, a dangerous or high-stepping gait, an apparent lack of awareness of foot position (sometimes standing or walking with the foot inverted), and a general inability to sense space and distance.[ 40] A similar condition known as cerebellar hypoplasia occurs when Purkinje cells fail to develop in the womb.
or die before birth.
The genetic conditions ataxia, telangiectasia and Niemann-Pick disease type C, as well as cerebellar essential tremor, involve progressive loss of Purkinje cells. In Alzheimer's disease, spinal pathology is sometimes observed, as is loss of dendritic branches of Purkinje cells.[41] Purkinje cells can also be damaged by rabies virus migrating from a peripheral site of infection into the central nervous system.[42]
Recommendations
- Jones, Daniel (2011). Roach, Peter; Setter, Jane; Esling, John (ed.). Cambridge Dictionary of English Pronunciation
(18th ed.). Cambridge University Press. ISBN 978-0-521-15255-6. - Komuro, Y.; Kumada, T.; Ono, N.; Foote, K. D.; Komuro, H. (January 1, 2013), Rubinstein, John L. R.; Rakic, Pasko (ed.), "Chapter 15 - Migration in the Cerebellum", Cell Migration and the Formation of Neural Connections
, Oxford: Academic Press, pp. 281–297, doi:10.1016/b978-0-12-397266-8.00030-2 , ISBN 978-0-12-397266-8, received 2020-11-18 - Purves D, Augustine GJ, Fitzpatrick D, Hall WC, LaMantia A, McNamara JO and White LE (2008). Neurology.
4th ed . Sinauer Associates. pp. 432–4. ISBN 978-0-87893-697-7. - Tyrrell, T; Willshaw, D. (1992-05-29). "The cerebellar cortex: its modeling and the relevance of Marr's theory". Philosophical Transactions of the Royal Society of London.
Series B, Biological Sciences .
336
(1277):239–57. Bibcode:1992RSPTB.336..239T. Doi:10.1098/rstb.1992.0059. PMID 1353267. - Wadiche, J. I.; Yar, C. E. (2001-10-25). "Multivesicular release at climbing fiber–Purkinje cell synapses". Neuron
.
32
(2): 301–13. Doi:10.1016/S0896-6273(01)00488-3. PMID 11683999. - Kirsch, L; Liskovich, N; Chechik, G. (December 2012). Ohler, Uwe (ed.). "Localization of genes in cerebellar layers by ISH image classification". PLoS computational biology
.
8
(12): e1002790. Bibcode:2012PLSCB...8E2790K. Doi:10.1371/journal.pcbi.1002790. PMC 3527225. PMID 23284274. - Rong, Y; Wang T; Morgan J. (2004). "Identification of candidate Purkinje cell markers by gene expression profiling in wild-type and pcd3j mice." Molecular Research of the Brain
.
13
(2): 128–145. doi:10.1016/j.molbrainres.2004.10.015. PMID 15582153. - ^ a b c
Felizola S.J., Nakamura Y., Ono Y., Kitamura K., Kikuchi K., Onodera Y., Ise K., Takase K., Sugawara A., Hattangadi N., Rainey V. E. ., Sato F., Sasano N. (April 2014).
"PCP4: a regulator of aldosterone synthesis in human adrenal tissues". Journal of Molecular Endocrinology
.
52
(2): 159–167. doi:10.1530/JME-13-0248. PMC 4103644. PMID 24403568. - ^ a b
Wei P., Blandon J. A., Rong Y., Zakharenko S. S., Morgan J. I. (2011).
"Impaired locomotor learning and altered cerebellar synaptic plasticity in pep-19/PCP4 null mice." Mol.
Cell. Biol .
31
(14):2838–44. Doi:10.1128/MCB.05208-11. PMC 3133400. PMID 21576365. - Putkey JA, Kleerekoper Q, Gaertner TR, Waxham MN (2004). "A novel role for IQ motif proteins in the regulation of calmodulin function". J Biol.
Chem .
278
(50):49667–70. Doi:10.1074/jbc.C300372200. PMID 14551202. - Kleerekoper QK, Putkey JA (2009). "PEP-19, an intrinsically disrupted regulator of calmodulin signaling." J Biol.
Chem .
284
(12):7455–64. Doi:10.1074/jbc.M808067200. PMC 2658041. PMID 19106096. - Sotelo S, Rossi F (2013). "Migration and differentiation of Purkinje cells". Handbook of the Cerebellum and Cerebellar Diseases
. Doi:10.1007/978-94-007-1333-8_9. - Hoshino M (2006). "Molecular machinery governing the specification of GABAergic neurons in the cerebellum". Cerebellum
.
5
: 193–198. - Carletti B, Rossi F (2008). "Neurogenesis in the cerebellum". Neuroscientist
.
14
: 91–100. - Zordan, P., Croci, L., Hawkes, R., Consales, G. G. (2008). "Comparative analysis of proneural gene expression in the embryonic cerebellum". Dev Din
.
237
: 726–735. - Hess DC, Hill WD, Carroll JE, Borlongan CV (2004). "Do Bone Marrow Cells Generate Neurons?" Archives of Neuroscience
.
61
(4):483–485. Doi:10.1001/archneur.61.4.483. PMID 15096394. - Weimann JM, Johansson CB, Trejo A, Blau HM (2003). "Stable reprogrammed heterokaryons form spontaneously in Purkinje neurons after bone marrow transplantation." The Nature of Cell Biology
.
5
(11): 959–966. doi:10.1038/ncb1053. PMID 14562057. - Alvarez-Dolado M., Pardal R., Garcia-Verdugo J.M., Fike J.R., Lee H.O., Pfeffer K., Lois S., Morrison S.J., Alvarez-Builla A. ( 2003). "Fusion of bone marrow cells with Purkinje neurons, cardiomyocytes and hepatocytes." Nature
.
425
(6961):968–973. Bibcode:2003Natura.425..968A. doi:10.1038/nature02069. HDL:2027.42/62789. PMID 14555960. - ^ a b
Felizola S. J., Katsu K., Ise K., Nakamura Y., Arai Y., Sato F., Sasano H. (2015).
"Expression of pre-B lymphocyte protein 3 (VPREB3) in the adrenal cortex: precedent for a non-immunological role in human normal and tumor tissues". Endocrine pathology
.
26
(2): 119–28. Doi:10.1007/s12022-015-9366-7. PMID 25861052. - Kemp, K., Wilkins, A., Bran, N. (2014). "Cell Fusion in the Brain: Two Cells Forward, One Cell Back." Acta Neuropathologica
.
128
(5):629–638. Doi:10.1007/s00401-014-1303-1. PMC 4201757. PMID 24899142. - Eric R. Kandel, James H. Schwartz, Thomas M. Jessel (2000). Principles of Neuroscience.
4/e. McGraw-Hill. pp. 837-40. - Loewenstein, Y., Mahon, S., Chadderton, P., Kitamura, K., Sompolinski, N., Yarom, Y., et al. (2005). "Bistability of cerebellar Purkinje cells modulated by sensory stimulation". Nature Neuroscience
.
8
(2): 202–211. Doi:10.1038/nn1393. PMID 15665875. - Schonewille M, Khosrovani S, Winkelman BH, Hoebeek FE, DeJeu MT, Larsen IM, et al. (2006). "Purkinje cells in awake animals operate at elevated membrane potential." Nature Neuroscience
.
9
(4): 459–461. Doi:10.1038/nn0406-459. PMID 16568098. - Loewenstein, Y., Mahon, S., Chadderton, P., Kitamura, K., Sompolinski, N., Yarom, Y., et al. (2006). “Purkinje cells in awake animals operate at elevated membrane potential—the answer.” Nature Neuroscience
.
9
: 461. doi:10.1038/nn0406-461. - Yartsev M.M., Givon-Majo R., Maller M., Donchin O. (2009). "Purkinje cell arrest in the cerebellum of the awake cat." Frontiers in Systems Neuroscience
.
3
: 2. doi:10.3389/neuro.06.002.2009. PMC 2671936. PMID 19390639. - Forrest MD (2014). “Intracellular calcium dynamics enable the Purkinje neuron model to perform switching and gain computations on inputs.” Frontiers in Computational Neuroscience
.
8
: 86. doi:10.3389/fncom.2014.00086. PMC 4138505. PMID 25191262. - Kreitzer AC, Regehr WG (March 2001). "Retrograde inhibition of presynaptic calcium influx by endogenous cannabinoids at excitatory synapses onto Purkinje cells." Neuron
.
29
(3): 717–27. Doi:10.1016/S0896-6273(01)00246-X. PMID 11301030. - Forrest MD, Wall MJ, Press DA, Feng J (December 2012). Tsymbalyuk G (ed.). "The sodium-potassium pump controls intrinsic activation of the cerebellar Purkinje neuron." PLoS ONE
.
7
(12):e51169. Bibcode:2012PLoSO ... 751169F. Doi:10.1371/journal.pone.0051169. PMC 3527461. PMID 23284664. - Forrest MD (December 2014). “The sodium-potassium pump is the information processing element of brain computation.” Frontiers of Physiology
.
5
(472): 472. doi:10.3389/fphys.2014.00472. PMC 4274886. PMID 25566080. - Cannon C (July 2004). "Paying the price of being pumped: dystonia due to mutations in the Na+/K+-ATPase." Neuron
.
43
(2): 153–154. doi:10.1016/j.neuron.2004.07.002. PMID 15260948. - Calderon, D. P., Fremont, R., Krenzlin, F., Khodakha, K. (March 2011). "Neural substrates of rapidly developing dystonia-parkinsonism". Nature Neuroscience
.
14
(3): 357–65. Doi: 10.1038 / No. 2753. PMC 3430603. PMID 21297628. - Forrest MD (2014). “Intracellular calcium dynamics enable the Purkinje neuron model to perform switching and gain computations on inputs.” Frontiers in Computational Neuroscience
.
8
: 86. doi:10.3389/fncom.2014.00086. PMC 4138505. PMID 25191262. - Forrest, M.D. (April 2015). "Modeling the effects of alcohol using a detailed Purkinje neuron model and a simpler surrogate model that runs >400 times faster." BMC Neuroscience
.
16
(27): 27. doi:10.1186/s12868-015-0162-6. PMC 4417229. PMID 25928094. - Forrest, Michael (April 2015). "the_neuroscience_reason_we_fall_over_when_drunk." Science 2.0
. Date accessed: May 2015.. Check date values in: | access date = (help) - ^ a b
Mitoma H, Adhikari K, Aeschlimann D, Chattopadhyay P, Hadjivassiliou M, Hampe CS et al. (2016).
"Consensus document: neuroimmune mechanisms of cerebellar ataxia". Cerebellum
(Consideration).
15
(2): 213–32. Doi:10.1007/s12311-015-0664-x. PMC 4591117. PMID 25823827. - Jaber M (2017). "The cerebellum as a major player in movement disorders associated with autism spectrum disorders." Encephalus
(Consideration).
43
(2): 170–175. doi:10.1016/j.encep.2016.03.018. PMID 27616580. - Sapone A, Bai JC, Ciacci S, Dolinsek J, Green PH, Hadjivassiliou M, Kaukinen K, Rostami K, Sanders DC, Schumann M, Ullrich R, Villalta D, Volta U, Catassi S, Fasano A (2012). "The Spectrum of Gluten-Related Diseases: Consensus on New Nomenclature and Classification." BMC Medicine
(Consideration).
10
: 13. doi:10.1186/1741-7015-10-13. PMC 3292448. PMID 22313950. - ^ a b c
Hadjivassiliou M., Sanders D.D., Aeschlimann D.P.
(2015). "Gluten-Related Disorders: Celiac Ataxia." Dig Dis
(Consideration).
33
(2): 264–8. Doi:10.1159/000369509. PMID 25925933. - Stucki, D. M., Ruegsegger, S., Steiner, S., Radeke, J., Murphy, M. P., Zuber, B., Saxena, S. (August 2021). “Mitochondrial dysfunction contributes to the progression of spinocerebellar ataxia type 1 and may be improved by the mitochondria-targeted antioxidant MitoQ” (PDF). Free Radich.
Biol. Med .
97
: 427–440. doi:10.1016/j.freeradbiomed.2016.07.005. PMID 27394174. - For references, see the extensive references and bibliography in the article on Cerebellar abiotrophy, linked at the beginning of this paragraph.
- Mavroudis, IA; Fotiu, D.F.; Adipepe, L.F.; Manani, M. G.; Njau, SD; Psaroulis, D; Costa, V.G.; Baloyannis, S. J. (November 2010). "Morphological changes in human Purkinje cells and deposition of neuritic plaques and neurofibrillary tangles on the cerebellar cortex in Alzheimer's disease." American Journal of Alzheimer's Disease and Other Dementias
.
25
(7): 585–91. Doi:10.1177/1533317510382892. PMID 20870670. - Fekadu, Makonnen (27 March 2009). "Rabid encephalitis, Negri bodies in the cytoplasm of cerebellar Purkinje cell neurons." CDC/Frontal Cortex Inc. Retrieved June 21, 2013. Note: Not peer-reviewed.
Links[edit]
- Jones, Daniel (2011). Roach, Peter; Setter, Jane; Esling, John (ed.). Cambridge Dictionary of English Pronunciation
(18th ed.). Cambridge University Press. ISBN 978-0-521-15255-6. - Komuro, Y.; Kumada, T.; Ono, N.; Foote, K. D.; Komuro, H. (January 1, 2013), Rubinstein, John L. R.; Rakic, Pasko (ed.), "Chapter 15 - Migration in the Cerebellum", Cell Migration and the Formation of Neural Connections
, Oxford:. Academic Press, pp. 281-297, DOI: 10.1016/b978-0-12-397266-8.00030-2, ISBN 978-0-12-397266-8, retrieved November 18, 2021 - Purves D, Augustine GJ, Fitzpatrick D, Hall, Toilet, LaMantia A, McNamara JO and White LE (2008). Neurology. 4th ed
. Sinauer Associates. pp. 432–4. ISBN 978-0-87893-697-7. - Tyrrell, T; Willshaw, D. (1992-05-29). "The cerebellar cortex: its modeling and the relevance of Marr's theory". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences
.
336
(1277):239–57. Bibcode: 1992RSPTB.336..239T. DOI: 10.1098/rstb.1992.0059. PMID 1353267. - Wadiche, J. I.; Yar, C. E. (2001-10-25). "Multivesicular release at climbing fiber–Purkinje cell synapses". Neuron
.
32
(2): 301–13. DOI: 10.1016/S0896-6273(01)00488-3. PMID 11683999. - Kirsch, L; Liskovich, N; Chechik, G. (December 2012). Ohler, Uwe (ed.). "Localization of genes in cerebellar layers by ISH image classification". PLoS computational biology
.
8
(12): e1002790. Bibcode: 2012PLSCB...8E2790K. DOI: 10.1371/journal.pcbi.1002790. PMC 3527225. PMID 23284274. - Rong, Y; Wang T; Morgan J. (2004). "Identification of candidate Purkinje cell markers by gene expression profiling in wild-type and pcd3j mice." Molecular Brain Research
.
13
(2): 128–145. DOI: 10.1016/j.molbrainres.2004.10.015. PMID 15582153. - ^ a b c
Felizola SJ, Nakamura Y, Ono Y, Kitamura K, Kikuchi K, Onodera Y, Ise K, Takase K, Sugawara A, Hattangady N, Rainey WE, Satoh F, Sasano H (April 2014).
"PCP4: a regulator of aldosterone synthesis in human adrenal tissues". Journal of Molecular Endocrinology
.
52
(2): 159–167. DOI: 10.1530/JME-13-0248. PMC 4103644. PMID 24403568. - ^ a b
Wei P., Blandon J. A., Rong Y., Zakharenko S. S., Morgan J. I. (2011).
"Impaired locomotor learning and altered cerebellar synaptic plasticity in pep-19/PCP4 null mice". Mol.
Cell. Biol .
31
(14):2838–44. DOI: 10.1128/MCB.05208-11. PMC 3133400. PMID 21576365. - Putkey JA, Kleerekoper Q, Gertner TR, Waxham MN. (2004). "A novel role for IQ motif proteins in the regulation of calmodulin function". J Biol. Chem
.
278
(50):49667–70. DOI: 10.1074/jbc.C300372200. PMID 14551202. - Kleerekoper QK, Putkey JA (2009). "PEP-19, an intrinsically disrupted regulator of calmodulin signaling". J Biol. Chem
.
284
(12):7455–64. DOI: 10.1074/jbc.M808067200. PMC 2658041. PMID 19106096. - Jump up
↑ Sotelo C, Rossi F (2013).
"Migration and differentiation of Purkinje cells". Handbook of the Cerebellum and Cerebellar Diseases
. DOI: 10.1007/978-94-007-1333-8_9. - Jump up
↑ Hoshino M (2006).
"Molecular machinery governing the specification of GABAergic neurons in the cerebellum". Cerebellum
.
5
: 193–198. - Carletti B, Rossi F (2008). "Neurogenesis in the cerebellum". Neurologist
.
14
: 91–100. - Zordan R, Croci L, Hawkes R, Consalez GG. (2008). "Comparative analysis of proneural gene expression in the embryonic cerebellum". Dev Dyn
.
237
: 726–735. - Hess DC, Hill WD, Carroll JE, Borlongan CV (2004). “Do bone marrow cells generate neurons?” . Archives of Neuroscience
.
61
(4):483–485. DOI: 10.1001/archneur.61.4.483. PMID 15096394. - Weimann JM, Johansson CB, Trejo A, Blau HM (2003). "Stable reprogrammed heterokaryons form spontaneously in Purkinje neurons after bone marrow transplantation". The Nature of Cell Biology
.
5
(11): 959–966. DOI: 10.1038/ncb1053. PMID 14562057. - Alvarez-Dolado M, Pardal R, Garcia-Verdugo JM, Fike JR, Lee Ho, Pfeffer K, Lois S, Morrison SJ, Alvarez-Builla A (2003). "Fusion of bone marrow cells with Purkinje neurons, cardiomyocytes and hepatocytes". Nature
.
425
(6961):968–973. Bibcode: 2003Natur.425..968A. DOI: 10.1038/nature02069. HDL: 2027.42 / 62789. PMID 14555960. - ^ a b
Felizola S. J., Katsu K., Ise K., Nakamura Y., Arai Y., Sato F., Sasano H (2015).
"Expression of pre-B lymphocyte protein 3 (VPREB3) in the adrenal cortex: precedent for a non-immunological role in human normal and tumor tissues". Endocrine pathology
.
26
(2): 119–28. DOI: 10.1007/s12022-015-9366-7. PMID 25861052. - Kemp K, Wilkins A, Secularism N (2014). "Cell fusion in the brain: two cells forward, one cell back". Acta Neuropathologica
.
128
(5):629–638. DOI: 10.1007/s00401-014-1303-1. PMC 4201757. PMID 24899142. - Eric R. Kandel, James H. Schwartz, Thomas M. Jessell (2000). Principles of Neuroscience.
4/e. McGraw-Hill. pp. 837-40. - Loewenstein Y, Mahon S, Chadderton P, Kitamura K, Sompolinsky H, Yarom Y, et al. (2005). "Bistability of cerebellar Purkinje cells modulated by sensory stimulation". The Nature of Neuroscience
.
8
(2): 202–211. DOI: 10.1038/nn1393. PMID 15665875. - Schonewille M, Khosrovani S, Winkelman BH, Hoebeek FE, DeJeu MT, Larsen IM, et al. (2006). "Purkinje cells in awake animals operate at elevated membrane potential." The Nature of Neuroscience
.
9
(4): 459–461. DOI: 10.1038/nn0406-459. PMID 16568098. - Loewenstein Y, Mahon S, Chadderton P, Kitamura K, Sompolinsky H, Yarom Y, et al. (2006). “Purkinje cells in awake animals operate at elevated membrane potential—the answer.” The Nature of Neuroscience
.
9
: 461. DOI: 10.1038/nn0406-461. - Yartsev M.M., Givon-Majo R, Maller M, Donchiny O (2009). "Purkinje cell arrest in the cerebellum of the awake cat". Frontiers in Systems Neuroscience
.
3
: 2. doi: 10.3389/neur.06.002.2009. PMC 2671936. PMID 19390639. - Jump up
↑ Forrest MD (2014).
"Intracellular calcium dynamics allows a Purkinje neuron model to perform switching and gain calculations on its inputs". Frontiers in Computational Neuroscience
.
8
: 86. DOI: 10.3389/fncom.2014.00086. PMC 4138505. PMID 25191262. - Kreitzer AC, Reger WG (March 2001). "Retrograde inhibition of presynaptic calcium influx by endogenous cannabinoids at excitatory synapses onto Purkinje cells." Neuron
.
29
(3): 717–27. DOI: 10.1016/S0896-6273(01)00246-X. PMID 11301030. - Jump up
↑ Forrest MD, Wall MJ, Press DA, Feng J (December 2012).
Tsymbalyuk G (ed.). "The sodium-potassium pump drives intrinsic excitation of the cerebellar Purkinje neuron". PLoS ONE
.
7
(12):e51169. Bibcode: 2012PLoSO...751169F. DOI: 10.1371/journal.pone.0051169. PMC 3527461. PMID 23284664. - Jump up
↑ Forrest MD (December 2014).
"The sodium-potassium pump is the information processing element of brain computation". Frontiers of Physiology
.
5
(472): 472. DOI: 10.3389/fphys.2014.00472. PMC 4274886. PMID 25566080. - Cannon C (July 2004). "Pump toll: dystonia from mutations in Na+/K+-ATPase". Neuron
.
43
(2): 153–154. DOI: 10.1016/j.neuron.2004.07.002. PMID 15260948. - Calderon DP, Fremont R, Kraenzlin F, Khodakhah K (March 2011). "Neural substrates of rapidly developing dystonia-parkinsonism". The Nature of Neuroscience
.
14
(3): 357–65. DOI: 10.1038/nn.2753. PMC 3430603. PMID 21297628. - Jump up
↑ Forrest MD (2014).
"Intracellular calcium dynamics allows a Purkinje neuron model to perform switching and gain calculations on its inputs". Frontiers in Computational Neuroscience
.
8
: 86. DOI: 10.3389/fncom.2014.00086. PMC 4138505. PMID 25191262. - Forrest MD (April 2015). "Modeling the effects of alcohol on a detailed Purkinje neuron model and a simpler surrogate model that runs >400 times faster". BMC Neuroscience
.
16
(27): 27. DOI: 10.1186/s12868-015-0162-6. PMC 4417229. PMID 25928094. - Forrest, Michael (April 2015). "the_neuroscience_reason_we_fall_over_when_drunk". Science 2.0
. Retrieved May 2015. Check date values in: |access-date=(help) - ^ a b
Mitoma H., Adhikari K., Aeschlimann D., Chattopadhyay P., Hadjivassiliou M., Hampe S.S.
et al. (2016). "Consensus document: neuroimmune mechanisms of cerebellar ataxia". Cerebellum
(review).
15
(2): 213–32. DOI: 10.1007/s12311-015-0664-x. PMC 4591117. PMID 25823827. - Jump up
↑ Jaber M (2017).
"The cerebellum as a major player in movement disorders associated with autism spectrum disorders." Encephala
(Review).
43
(2): 170–175. DOI: 10.1016/j.encep.2016.03.018. PMID 27616580. - Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, Kaukinen K, Rostami K, Sanders DS, Schumann M, Ullrich R, Villalta D, Volta U, Catassi C, Fasano A (2012). "The spectrum of gluten-related disorders: consensus on new nomenclature and classification". BMC Medicine
(Review).
10
: 13. DOI: 10.1186/1741-7015-10-13. PMC 3292448. PMID 22313950. - ^ a b c
Hadjivassiliou M, Sanders JD, Aeschlimann JP.
(2015). "Gluten-Related Disorders: Celiac Ataxia." Dig Dis
(Review).
33
(2): 264–8. DOI: 10.1159/000369509. PMID 25925933. - Stuckey DM, Ruegsegger S, Steiner s, Radecke J, Murphy MP, Zuber V, Saxena S (August 2016). "Mitochondrial abnormalities contribute to the progression of spinocerebellar ataxia type 1 and may be improved by the mitochondria-targeted antioxidant MitoQ" (PDF). Free Radich. Biol. Med
.
97
: 427–440. DOI: 10.1016/j.freeradbiomed.2016.07.005. PMID 27394174. - For references, see the extensive references and bibliography in the article on cerebellar abiotrophy, linked at the beginning of this paragraph.
- Mavroudis, IA; Fotiu, D.F.; Adipepe, L.F.; Manani, M. G.; Njau, SD; Psaroulis, D; Costa, V.G.; Baloyannis, S. J. (November 2010). "Morphological changes in human Purkinje cells and deposition of neuritic plaques and neurofibrillary tangles on the cerebellar cortex in Alzheimer's disease." American Journal of Alzheimer's Disease and Other Dementias
.
25
(7): 585–91. DOI: 10.1177/1533317510382892. PMID 20870670. - Fekadu, Makonnen (27 March 2009). "Rabid encephalitis, Negri bodies in the cytoplasm of cerebellar Purkinje cell neurons". CDC/Frontal Cortex Inc. Retrieved June 21, 2013. Note: Not peer reviewed.