Anatomy
From above, the spinal cord passes into the medulla oblongata. Below, in the area of 1-2 lumbar vertebrae, the section ends with a point - a cone. In this area, a terminal (terminal) thin thread departs from it. This is a rudiment of the caudal (caudal) part of the spinal cord. The diameter of the structure is different in different areas. The spinal cord has thickenings in the lumbar and cervical regions. There is gray matter here. The thickenings are caused by the innervation of the lower and upper extremities.
There is a median fissure on the anterior surface, and a groove on the posterior surface. These elements divide the brain into left and right interconnected halves. In each of them, the posterior and anterior lateral grooves differ. The first is the area where the posterior sensory roots of the spinal nerves emerge, and the motor elements depart from the second. The lateral grooves are the boundaries between the posterior, lateral and anterior funiculi. Inside the spinal cord there is a central canal - a fissure. It is filled with liquor. The canal ends blindly from below (the terminal ventricle, which in an adult is completely or partially overgrown), and from above it passes into the fourth ventricle.
Diseases of peripheral processes
The main and most frequently diagnosed lesion of the peripheral plexuses, which is accompanied by functional disorders, is neuropathy or neuritis. Symptoms characteristic of a violation of motor, sensory, and autonomic function occur. The person feels pain that radiates along the affected segment.
Diseases that occur with dysfunction of the roots include: degenerative and dystrophic processes, metabolic disorders, inflammation of the roots and pinching by a tumor, osteophytes, hernia or other neoplasm.
Other peripheral plexus disorders:
- polyneuropathy, when several or many processes are involved in the lesion;
- plexitis is a disease characterized by damage to the entire plexus;
- radiculoneuritis is a simultaneous pathological process in the roots of the spinal canal and trunks;
- myeloradiculoneuritis - a condition characteristic of damage to the spinal cord, nerve trunks and roots;
- radiculitis – symptoms characteristic of injury to the spinal cord roots;
- ganglionitis is a pathological process characterized by damage to the intervertebral nodes.
Common forms of dysfunction of the peripheral nervous system are vertebrogenic diseases, for example, osteochondrosis. More often, the lesion involves structures that pass through narrow bony canals, such as the ischial process.
Departments
The spinal cord has the following parts:
- Coccygeal
- Sacral.
- Lumbar.
- Chest.
- Cervical.
Each part has segments. Pairs of spinal nerves extend along the entire length of the cord. There are 31 in total. The number of spinal nerves, depending on the segment, is as follows:
- Coccygeal - 1-3.
- Sacral – 5.
- Lumbar – 5.
- Infants – 12.
- Neck – 8.
Below, the spinal nerves form the cauda equina. During the growth of the body, the cord does not have time to reach the length of the canal. In this regard, the spinal nerves are forced to descend, exiting the foramina.
Nerve plexus diseases
Diseases of the spinal nerves affect the main functions of the body, including reflex and motor, as well as sympathetic. It is possible to determine which nerves suffer from inflammation by determining in which areas the innervation is impaired.
In particular, disturbances in the activity of the brachial plexus can be expressed in a number of consequences related to the functioning of the neck. In addition, the patient's fingers become numb. In the future, this can lead to weakening of the forelimbs as a whole. As a result, a person will be unable to hold them in weight or even lift them.
If disturbances appear in the meningeal branch, then the patient suffers from neurological disorders. In particular, his mandibular and trigeminal nerves become inflamed.
With inflammation of the nerves in the chest area, the patient suffers from neuralgia with intercostal localization. He experiences shortness of breath and pain, the causes of which he often sees as heart disease. However, their real source is precisely the problem with the nerves in this department.
Diseases of the sacral plexus will result in disturbances in the activity of organs localized in the pelvis. There may be numbness of the skin in this area. In serious cases, we can talk about paralysis of the lower limbs. A person may also suffer from dysfunction of the reproductive system; problems with the sciatic nerve, in particular, can lead to this consequence. In addition, pinching it can cause difficulty urinating and defecating, as well as pelvic pain.
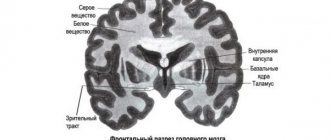
Internal Contents
The spinal cord contains white and gray matter. The latter consists of neurons. They form three columns in the halves of the spinal cord: lateral, posterior and anterior. In cross section, each of them looks like horns. There are narrow posterior and wide anterior horns. The lateral one corresponds to the vegetative intermediate column of the gray part. The anterior horns contain motor neurons, the lateral horns contain autonomic intercalary neurons, and the posterior horns contain sensory neurons. Renshaw cells are located in this same area. These are inhibitory neurons that slow down motor neurons from the anterior horns. The gray matter is surrounded by white matter, which forms the cords of the spinal cord. There are three of them in each half: side, rear and front. The cords consist of fibers running longitudinally. They, in turn, form bundles of nerves - pathways. Descending - extrapyramidal and pyramidal - are located in the anterior cords, in the white matter. In the laterals – ascending and descending:
- Lateral spinothalamic.
- Rear and anterior (Flexig and Gowers).
- Lateral (pyramidal) corticospinal.
- Red nuclear.
The white matter of the posterior cord includes ascending pathways:
- Burdach's bundle (wedge-shaped).
- Gaulle bundle (thin).
Shells
The outside of the spinal cord is covered by three structures:
- Arachnoid medium.
- Solid outer.
- Soft inner.
The epidural space is located between the periosteum of the spinal canal and the dura mater. It is filled with venous plexuses and fatty tissue. Between the arachnoid and dura mater there is the subdural space. It is permeated with thin connective tissue crossbars. The soft membrane is separated from the arachnoid by the subarachnoid subarachnoid space. It contains liquor. Cerebrospinal fluid is formed in the choroid plexuses located in the ventricles of the brain. Renshaw cells protect the central nervous system from overexcitation.
Prevention of violations
To eliminate the risk of disease of the nerve trunks and root sheaths, it is recommended first of all to lead a healthy and active lifestyle: stop smoking, drinking alcohol, and taking drugs.
You also need to maintain a balanced diet, including a sufficient amount of vegetables and fruits, meat, fish, seafood, and nuts. It is recommended to promptly identify and treat provoking infectious diseases and pathologies of non-infectious etiology.
It is necessary to exclude hypothermia, especially local. It causes the development of an inflammatory process in muscle structures that compress the endings, thereby causing pain symptoms.
If neurological symptoms are detected, you should immediately visit a doctor and undergo a comprehensive diagnosis. The sooner the cause of the disturbance in the structure and function of the plexuses is discovered, the more favorable the prognosis.
Functions of the spinal nerves
There are two of them. The first - reflex - is performed by nerve centers. They represent segmental working zones of unconditioned reflexes. The neurons of the centers communicate with organs and receptors. Each transverse section - a metamer of the body - has sensitivity transmitted from three roots. Innervation of skeletal muscles is also carried out by 3 adjacent spinal segments. Efferent impulses are also transmitted to the respiratory muscles, glands, blood vessels and internal organs. The overlying regions of the central nervous system regulate the activity of the periphery through segmental spinal regions. The second task - conduction - is performed thanks to descending and ascending paths. With the help of the latter, information is transmitted from temperature, pain, tactile and proprioceptors of tendons and muscles through neurons to the rest of the central nervous system to the cerebral cortex and cerebellum.
Ascending Paths
These include:
- Anterior spinothalamic. This is the afferent pathway of pressure and touch.
- Lateral spinothalamic. This is the path of temperature and pain sensitivity.
- Posterior and anterior spinocerebellar. These are afferent pathways of muscle-articular sensitivity of the cerebellar direction.
- Bundles of Burdach (wedge-shaped) and Gaulle (thin). These are afferent pathways for transmitting cortical muscle-articular sensitivity from the lower half of the torso and legs and from the upper body and arms, respectively.
Spinal nerve formation
How does this happen? The spinal nerve is formed by connecting the posterior sensory and anterior motor areas. At its exit from the intervertebral foramen, fiber separation occurs. As a result of this, branches of the spinal nerves are formed: posterior and anterior. They perform mixed tasks. The meningeal and white communicating branches also depart from the spinal nerves. The first return to the spinal canal and innervate the dura mater. The white branch approaches the nodes of the sympathetic trunk. Against the background of various curvatures of the spine (scoliosis, kyphosis, pathological lordosis), deformation of the intervertebral foramina occurs. As a result, the spinal nerves become pinched. This leads to various kinds of violations.
Spinal nerves
The spinal nerves are divided into 8 pairs of cervical, 12 thoracic, 5 lumbar, 5 sacral and one pair of coccygeal nerves according to the brain regions.
After leaving the intervertebral foramen, each mixed nerve (Fig. 298) is divided into two mixed branches: the posterior thin and short, the branches of which branch with their motor fibers in the muscles of the spine, and the sensory fibers end in the skin of the posterior surface of the body, and the anterior thick and long - for muscles and skin of the trunk and limbs. In addition to these two large branches, the mixed spinal nerve sends out two small branches, of which one returns back to the spinal canal and innervates the hard shell of the spinal cord there, and the second connects to the node of the sympathetic trunk.
Rice. 298. Diagram of the formation and branches of the spinal nerve. 1 - cutaneous branch; 2 - medial branch of the posterior branch of the nerve; 3 - posterior root of the spinal cord; 4 - posterior median sulcus of the spinal cord; 5 - posterior horn of the gray matter of the spinal cord; 6 - lateral cord of the spinal cord; 7 - anterior horn of the gray matter of the spinal cord; 8 and 9 - medial and lateral cutaneous branches; 10 and 16 - anterior branch of the spinal nerve; 11 and 15 - small muscle branches; 13 - lateral cutaneous branch of the anterior branch; 12, 14 - its medial and lateral branches; 17 - posterior branch of the nerve; 18, 19 - its branches; 20 - spinal node; 21 - sympathetic node
All anterior branches of the spinal nerves (except the thoracic ones) are connected to each other in the form of loops and form nerve plexuses (plexus). There are cervical, brachial, lumbar, sacral, and coccygeal plexuses. Separate nerves, mostly of a mixed nature, depart from the plexuses, although a few branches contain only sensory fibers.
Cervical plexus
(plexus cervicalis) (Fig. 299) is formed from the anterior four upper cervical nerves. It is located on the anterior surface of the scalene muscles near their places of attachment to the transverse processes of the cervical vertebrae and is covered in front by the upper part of the sternocleidomastial muscle. The branches of the cervical plexus are divided into superficial (cutaneous, sensory) and deep (muscular, motor). Superficial branches innervate the skin of the neck, back of the head, and auricle. The deep branches supply the cervical muscles (the scalenes and all those lying below the hyoid bone) and the diaphragm. One of these deep branches is the nerve of the thoracoabdominal septum (n. phrenicus) * - this is the longest nerve of the cervical plexus, which is of great practical importance. It arises from the IV cervical nerve, runs along the anterior surface of the anterior scalene muscle, then passes between the subclavian artery and vein, descends down into the chest cavity, passes here between the pleura and the pericardium, reaches the diaphragm and branches in it. This nerve supplies the diaphragm with its motor fibers, and the pericardium, pleura, peritoneum and ligaments of the liver with sensory fibers. When this nerve is irritated, hiccups and contraction of the diaphragm are often observed.
* (From the Greek word phren - diaphragm.
)
Rice. 299. Nerves of the head and neck (cervical plexus). 1 - cutaneous nerve of the neck; 2 - supraclavicular nerves; 3 - great auricular nerve; 4 - lesser occipital nerve; 5 - accessory nerve (XI pair of cranial nerves); 6 - posterior branch of the second cervical spinal nerve; 7, 9, 10, 11 - branches of the trigeminal nerve (V pair of cranial nerves); 8 - facial nerve (VII pair of cranial nerves). The branches of the facial nerve to the facial muscles are shown
Brachial plexus
(plexus brachialis) (Fig. 300, 301) consists of the anterior branches of the four lower cervical nerves and partly one of the thoracic nerves. It is located in the neck between the anterior and middle scalene muscles. From the plexus itself, short motor branches extend to the muscles of the shoulder girdle. The plexus forms three large nerve trunks, which, surrounding the subclavian artery, go down with it and, bending over the rib, enter the axillary fossa. Mixed and sensory nerves that innervate the entire upper limb already depart from these nerve bundles.
Rice. 300. Brachial plexus. 1 - superior cervical sympathetic node; 2 - longus colli muscle; 3 - anterior branch of the V cervical nerve; 4 - anterior branch of the VI cervical nerve; 5 - ascending cervical artery; 6 - anterior branch of the VII cervical nerve; 7 - vertebral artery; 8 - anterior branch of the VIII cervical nerve; 9 - shield-cervical trunk; 10 - costocervical trunk; 11 - vagus nerve (cut); 12 - internal artery of the mammary gland; 13 - phrenic nerve; 14 - anterior scalene muscle (cut); 15 - subclavian artery; 16 - transverse artery of the neck; 17 - prothoracic nerves (branches to the pectoralis major muscle); 18 - medial trunk of the brachial plexus; 19 - median nerve; 20 - lateral trunk of the brachial plexus; 21 - trapezius muscle; 22 - middle and posterior scalene muscles
Rice. 301. Nerves of the brachial plexus. 1 - short head of the biceps muscle; 2 and 17 - pectoralis major muscle; 3 - coracobrachial muscle; 4 - deltoid muscle; 5 - axillary artery; 6 and 18 - pectoralis minor muscle; 7 - collarbone; 8 and 15 - subclavian artery; 9 - suprascapular nerve; 10 - phrenic nerve; 11, 13 — brachial plexus; 12 - middle scalene muscle; 14 - vertebral artery; 16 - 1st rib; 19 - serratus anterior muscle; 20 - branches of the brachial plexus; 21 - anterior edge of the vastus dorsi muscle; 22 - axillary nerve; 23 - ulnar nerve; 24 - cutaneous medial nerve of the forearm; 25 - median nerve; 26 - brachial artery; 27 - musculocutaneous nerve
The sensory long nerves include mainly two nerves: the medial cutaneous nerve of the shoulder (n. cutaneus brachii medialis) and the medial cutaneous nerve of the forearm (n. cutaneus antibrachii medialis). Both nerves innervate the skin of the shoulder and forearm throughout the inner (ulnar) side of the upper limb. There are five mixed nerves of the plexus: The musculocutaneous nerve (n. musculo-cutaneus) (Fig. 302) pierces the coracobrachial muscle. This nerve innervates all the muscles of the anterior surface of the shoulder: biceps, coracobrachialis and brachialis (forearm flexors); its sensitive branch supplies the skin of the lateral side of the forearm.
Rice. 302. Nerves of the shoulder. 1 - brachioradialis muscle; 2 - muscular branches of the median nerve; 3 - brachial artery; 4 - medial cutaneous nerve of the forearm; 5 - lateral cutaneous nerve of the forearm; 6 and 11 - biceps muscle; 7 - median nerve; 8 and 13 - musculocutaneous nerve; 9 - pectoralis major muscle; 10 - coracobrachial muscle; 12 - deltoid muscle; 14 - coracoid process; 15 - part of the pectoralis minor muscle; 16 - collarbone; 17 and 19 - brachial plexus; 18 - axillary artery; 20 - subscapularis muscle; 21 - tendon of the vastus dorsi muscle; 22 - axillary nerve; 23 - radial nerve; 24 and 28 - ulnar nerve; 25 - muscle branches from the radial nerve; 26 and 27 - long and medial head of the triceps brachii muscle; 29 - brachialis muscle
The axillary nerve (n. axillaris) is quite thick, but shorter than the others, goes to the shoulder behind the artery of the same name, then, bending around the humerus in the area of the surgical neck, goes to the back of the shoulder and innervates the deltoid muscle and the shoulder joint; its sensitive branch passes to the skin of the lateral surface of the shoulder; this is the shortest of the five mixed nerves of the plexus, and the rest are long and run along the entire length of the upper limb.
The ulnar nerve (n. ulnaris) comes from the medial trunk of the brachial plexus. From the inner surface of the shoulder, the nerve passes in the middle to the back side and runs along the back surface of the medial condyle of the shoulder, covered only by skin and fascia (nerve bruises sometimes occur here, causing sharp pain). On the forearm, it is located next to the ulnar artery and gives off a number of muscle branches, innervating the flexor carpi ulnaris and part of the flexor digitorum profundus. Continuing onto the hand, the ulnar nerve gives branches to the skin of the 5th and 4th fingers, to the interosseous and lumbrical muscles, and to the hypothenar muscles. Its dorsal branch innervates the ulnar half of the skin of the dorsum of the hand. With paralysis of this nerve, the fingers take on a characteristic claw-like position, since the action of the lumbrical and interosseous muscles that flex the main phalanges is lost, or the action of the muscles that flex the nail and middle phalanges is retained.
The radial nerve (n. radlalis) is the most powerful nerve of the upper limb; it innervates all the posterior muscles and the skin of the dorsal surface of the upper limb, i.e. all extensors of the shoulder (triceps and ulnaris), forearms, supinator and brachioradialis muscle, as well as the bursa of the elbow joint and the skin of the posterior surface of the shoulder, forearm and radial half of the dorsum brushes Coming from the posterior bundle of the brachial plexus, the radial nerve spirals around the humerus, passes along with the deep brachial artery in the canal formed by the bone and the triceps muscle, and appears in the lateral groove of the cubital fossa. Here it is divided into two branches - superficial and deep. The first goes to the skin of the dorsal surface of the hand and innervates its radial half, the second - to the muscles of the dorsal surface of the forearm.
The median nerve (n. medianus) (Fig. 303) begins with two legs from the lateral and medial trunks of the brachial plexus. It is located along the inner edge of the shoulder next to the brachial artery, under the edge of the biceps muscle; here, the nerve does not give branches. Descending onto the forearm, it pierces the pronator teres, branches and innervates most of the flexors of the forearm (except for the flexor carpi ulnaris and part of the deep flexor digitorum), part of the lumbrical interosseous muscles and the skin of 31/2 fingers, as well as the pronators and the wrist joint. On the palmar surface of the hand, the median nerve gives motor branches to the thenar muscles and sensory branches to part of the skin of the palmar surface.
Rice. 303. Nerves of the forearm. 1 - biceps brachii; 2 - radial nerve; 3 - deep branch of the radial nerve; 4 - its muscular branches; 5 - brachialis muscle; 6 to 10 - superficial branch of the radial nerve; 7 - radial artery; 8 and 11 - brachioradialis muscle; 9 - interosseous membrane; 12 - palmar transverse carpal ligament; 13 and 17 - ulnar artery; 14-18 - ulnar nerve; 15 and 25 - median nerve; 16 - flexor carpi ulnaris; 19 - palmar interosseous artery; 20 - dorsal interosseous artery; 21 - common interosseous artery; 22 - ulnar artery; 23 - muscular branches of the median nerve; 24 - ulnar nerve; 26 - brachial artery
The median and ulnar nerves do not give branches to the shoulder; on the forearm (Fig. 303) most of the branches give rise to the median nerve, on the hand - the ulnar nerve.
Intercostal nerves
(nn. intercostales) (Fig. 304) also belong to the group of mixed nerves. The anterior branches of the thoracic nerves do not form a plexus; they each run independently, parallel to one another along the intercostal spaces in the number of 12 pairs, located between the internal and external intercostal muscles, giving off sensitive branches to the skin and motor branches to the intercostal muscles. The upper six intercostal nerves supply the skin, mammary gland and chest muscles, and the lower six enter the abdominal muscles and innervate the abdominal muscles and abdominal skin.
Rice. 304. Intercostal nerves of the right side. 1, 2, 7, 15 - intercostal nerves and their branches to the muscles and skin of the chest; 3, 5, 6, 12, 13 - branches of the intercostal nerves to the muscles and skin of the abdominal wall; 4 - sheath of the rectus abdominis muscle; 3 - 1st rib; 9, 10 - branches of the lumbar plexus to the abdominal wall; 11 - transverse abdominal muscle; 14 - XII rib
From each of the anterior branches of the intercostal nerves a connecting branch departs to the border trunk of the sympathetic nervous system. The posterior branches of the intercostal nerves innervate the skin and muscles of the back.
Lumbar plexus
(plexus lumbalis) is formed from the anterior branches of the XII thoracic and four upper lumbar nerves. It is located on the transverse processes of the lumbar vertebrae in the thickness of the iliopsoas muscle. The nerves from this plexus emerge from under the outer edge of the muscle, while some of them pierce the muscle and exit onto its anterior surface. The short branches of the plexus supply the iliopsoas muscle, quadratus lumborum muscle, lower abdominal muscles, and pubic skin with their sensory and motor fibers.
The iliohypogastric nerve (n. iliohypogastricus) consists of fibers belonging to the XII intercostal nerve (called subcostal) and the branch of the I lumbar spinal nerve. It first runs on the anterior surface of the quadratus lumborum muscle and then between the transversus abdominis and internal oblique muscles. Innervates the broad abdominal muscles, pyramidalis muscle, skin of the suprapubic and gluteal regions.
The ilioinguinal nerve (n. ilioinguinalis) innervates the lower parts of the abdominal muscles, exits through the external opening of the inguinal canal into the skin of the scrotum in men or the labia majora in women.
The nerve of the genital organs and thigh (n. genito-femoralis) is divided into two branches. One of them leaves the pelvis through the vascular lacuna, accompanying the femoral artery, and branches in the skin of the thigh under the inguinal ligament in the area of the oval fossa and slightly below it in the upper third of the thigh. Its other branch passes through the inguinal canal, innervating the levator testis muscle along the way, exits through the external opening of the canal and branches in the upper medial part of the thigh and in the skin of the scrotum in men or the labia majora in women.
Of the long branches of the lumbar plexus (Fig. 305), the largest is the femoral nerve (n. femoralis), it passes under the inguinal ligament through the muscle lacuna, splits into many branches and innervates the muscles (quadriceps and together with the obturator nerve - adductors), the skin of the anterior surface of the thigh, skin on the medial surface of the leg and foot, as well as the knee joint. The long branch of the femoral nerve is the long internal cutaneous nerve of the lower limb (n. saphenus), which descends along the medial surface of the thigh, leg and foot, accompanying the vein of the same name.
Rice. 305. Nerves of the anterior surface of the thigh. 1 - anterosuperior iliac spine; 2 - Pupart's (inguinal) ligament; 3 - lumboiliac muscle; 4 and 8 - sartorius muscle; 5 - rectus femoris muscle; 6 - vastus lateralis muscle; 7 - vastus medialis muscle; 9 and 16 - femoral artery; 10 - great saphenous nerve (n. saphencs); 11 - long adductor muscle of the thigh; 12 - obturator nerve; 13 - spermatic cord; 14 - pectinate muscle; 15 - femoral vein; 17 - inferior epigastric artery; 18 - femoral nerve
The obturator nerve (n. obturatorius) descends down to the lateral wall of the pelvic cavity, from there through the obturator canal it enters the thigh and innervates the adductor muscles of the thigh, hip joint and skin of the inner surface of the thigh.
The lateral cutaneous nerve (n. cutaneus femoris lateralis) is sensitive and innervates the skin of the anterolateral and lateral surface of the thigh.
Sacral plexus
(plexus sacralis) (Fig. 306, 307, A and B) is formed from the anterior branches of the V lumbar and four sacral nerves. This is the largest plexus of the human body. It lies in the pelvis on the anterior surface of the piriformis muscle. Short and long branches also extend from it. The constituent anterior rami converge towards the greater sciatic foramen, forming a thick triangular plate, the apex of which becomes the sciatic nerve.
Rice. 306. Sacral and coccygeal plexus (diagram). 1 - ponytail; 2 - V lumbar vertebra; 3 - sacral vertebrae; 4 - anterior branches of the sacral nerves; 5 - pudendal nerve; 6 - branch to the rectum; 7 - branches to the muscles of the perineum; 8 - branches to the genitals; 9 - cavernous bodies; 10 - internal obturator muscle; 11 - pubic fusion; 12 - sciatic nerve; 13 - posterior cutaneous nerve of the thigh; 14 - branches to the gluteal muscles; 15 - branches to the muscles of the posterior surface of the hip joint; 16 - branches to the fascia lata of the thigh; 17 - iliac crest; 18 - external iliac vessels; 19 - coccygeal plexus
Rice. 307. Nerves of the sacral plexus (posterior surface of the thigh and lower leg). A - thigh. 1, 2 - superior gluteal artery and nerve; 3, 6 - sciatic nerve; 4 - artery accompanying the sciatic nerve; 5, 7, 15, 16 - muscular branches of the sciatic nerve; 8 - biceps femoris muscle; 9 - tibial nerve; 10 - peroneal nerve; 11 - lateral cutaneous nerve of the calf; 12 - cutaneous branch; 13 - tibial nerve; 14 - its muscular branch; 17 - posterior cutaneous nerve of the thigh; 18 - lower nerves of the ischium; 19, 22 - inferior gluteal nerve; 20, 21 - internal pudendal artery and nerve. B - shin. 1 - sciatic nerve; 2, 3 - peroneal nerve; 4, 13 - tibial nerve; 5, 8, 10, 11, 12, 15, 16, 17 - its muscular branches; 6 - lateral cutaneous nerve of the calf; 7 - muscular branches of the peroneal nerve; 9 - peroneal artery; 14 - tibial artery; 18 - popliteal artery
The short branches of the plexus include two gluteal nerves (n. glutaeus superior and n. glutaeus inferior), innervating the gluteal muscles and the pudendal nerve (n. pudendus), supplying the skin and muscles of the perineum.
The long branches include the sciatic nerve and the posterior cutaneous nerve of the thigh. The sciatic nerve (n. ischiadicus) is the thickest of all the nerves of the body. It leaves the pelvic cavity through the infrapiriform foramen, then lies between the muscles of the back of the thigh, where it gives branches to the flexors of the leg and to the adductor muscles of the thigh. Somewhat before reaching the popliteal fossa, the sciatic nerve is divided into two terminal branches - the tibial and peroneal nerves.
The tibial nerve (n. tibialis) (see Fig. 307) at the top of the leg is located under the soleus muscle, and at the bottom, together with the posterior tibial artery and veins behind the medial malleolus. It innervates all the flexors on the back of the leg. Curving around the inner ankle of the leg, it passes to the foot, where it divides into branches that innervate the skin and muscles of the sole.
The peroneal nerve (n. peronaeus) (Fig. 308) goes around the outside of the fibula and passes to the anterior surface of the leg; it innervates the knee joint, the skin and muscles of the lateral and anterior surface of the leg and the dorsum of the foot.
Rice. 308. Nerves of the anterior side of the leg. 1 - muscular branches of the deep peroneal nerve; 2 and 7 - anterior tibial artery; 3 - extensor digitorum longus; 4 - peroneal muscles; 5 and 9 - deep peroneal nerve; 6 - superficial peroneal nerve; 8 - tendon of the third peroneal muscle; 10 - dorsal artery of the foot; 11 - tendon of the anterior tibialis muscle; 12 - interosseous membrane; 13 - tibialis anterior muscle; 14 - patella
The posterior cutaneous nerve of the thigh (n. cutaneus femoris posterior) is a purely sensory nerve. It leaves the pelvis along with the inferior gluteal nerve and is located under the skin of the posterior thigh, innervating its skin, as well as the skin of the lower part of the gluteal region.
The pudendal plexus (plexus pudendus) comes from the anterior branches of the II, III and IV sacral spinal nerves and is in connection with the sacral and coccygeal plexuses, located below the piriformis muscle. Its branches supply the skin and muscles of the perineum, external genitalia and part of the pelvic organs. Its largest branches are: a) the perineal nerve (n. perinei) and b) the dorsal nerve of the penis n. dorsalis penis (in women - n. dorsalis clitoridis).
The coccygeal plexus (plexus coccygeus) is formed from the anterior branches of the V sacral and the only coccygeal nerves. Its thin stem innervates the skin of the perineum between the coccyx and the anus.